Multifocal Cutaneous Tuberculosis in Immunocompetent Individual
Malay Mehta1, Gopikrishnan Anjaneyan2, Kirti Rathod3, Rita V Vora4
1 Resident, Department of Skin and VD, Pramukhswami Medical College, Karamsad, Gujarat, India.
2 Former Assistant Professor, Department of Skin and VD, Pramukhswami Medical College, Karamsad, Gujarat, India.
3 Associate Professor, Department of Pathology, Pramukhswami Medical College, Karamsad, Gujarat, India.
4 Professor and Head, Department of Skin and VD, Pramukhswami Medical College, Karamsad, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rita Vora, Shree Krishna Hospital, Pramukhswami Medical College, Gokal Nagar, Karamsad- 388325, Anand, Gujarat, India.
E-mail: ritavv@charutarhealth.org
Most common form of cutaneous tuberculosis (TB) is lupus vulgaris, which usually occurs in previously sensitized individuals who have a high degree of tuberculin sensitivity. Various forms including plaque, ulcerative, hypertrophic, vegetative, papular, and nodular forms have been described. We are reporting a case of a young female, who presented with 6 well defined erythematous scaly plaques involving both arms and a puckered scar on right forearm and right breast. Clinically, it was looking like lupus vulgaris with cold abscess, few lesions mimicking scrofuloderma, but skin biopsy from both the types of lesions revealed lupus vulgaris. Patient improved with Anti Tuberculous Therapy and surgical drainage of underlying cold abscess.
Anti Tuberculous Therapy, Cold abscess, Lupus vulgaris, Scrofuloderma
Case Report
A 20-year-old female presented with non tender, fluctuant, soft swelling of left elbow, inability to flex elbows fully, plaques over both arms. On examination, there were 6 well defined erythematous scaly plaques, around 4-6 cm in diameter, involving both the arms. A single ulcer with purulent crust present over extensor aspect of left forearm. Atrophic scars were present over right elbow and right breast. Hyperpigmented puckered scar with multiple discharging sinuses were present over right forearm. There was no lymphadenopathy. On diascopy, "apple jelly" nodules were appreciated in form of yellowish discolouration after applying pressure with slide over the lesion. A fluctuant swelling of 8×11 cm size was present over extensor aspect of left arm along with swollen right elbow, due to which she was not able to flex her elbow completely [Table/Fig-1]. Range of motion was 40 and 50 degree flexion at left and right elbow respectively. All lesions appeared in the span of 3 years. No past history of pulmonary TB. There was no history of trauma. She was vaccinated with BCG vaccine with a vaccine scar over her left deltoid. Her height was 137cm and weighed 42kg with significant undernourishment. She lives in overcrowded slum with poor hygienic conditions. Her aunt was suffering from pulmonary tuberculosis. Lupus vulgaris and scrofuloderma were suspected in the same case as erythematous plaques and puckered scar with sinus formation were there.
Psoriasiform erythematous scaly plaques over the right arm with a puckered scar near medial side of right elbow whereas, left elbow is swollen and shows crusting with discharging sinuses

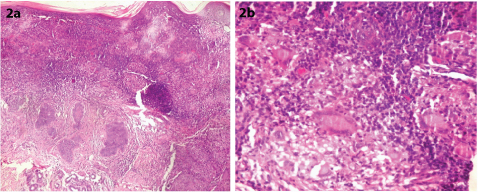
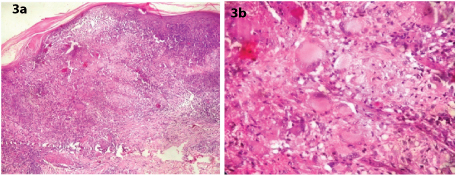
Mantoux test was positive (>15mm induration and 22mm horizontal extension). Pus discharge from the ulcer was negative for grams and AFB stain didn’t show any growth on routine culture. ELISA for HIV was nonreactive. Biopsy was taken from the erythematous plaque as well as puckered scar which showed mild hyperplasia of epidermis with multiple granulomas in dermis containing Langhans giant cells, epitheloid cells, lymphocytes and plasma cells suggestive of lupus vulgaris at both the sites. Reticular dermis was normal. No caseation necrosis was seen in both biopsies [Table/Fig-2,3]. ZN stain was done, which did not show any acid fast bacilli. PAS staining was done for fungal infection, which was negative. Chest and bilateral upper limb X-ray were normal. Ultrasonographic finding of left arm was suggesting 8×10.2×12.1cm size fluctuant abscess over extensor aspect. Patient was kept on Anti Tuberculosis Therapy under Revised National Tuberculosis Control Programme (RNTCP) category 2. Tab Isoniazid (600mg); Tab Pyrazinamide (1500mg); Tab Ethambutol (1200mg); Tab Rifampicin (450mg); Streptomycin (750mg) for 2 months 3 times a week; followed by Tab Isoniazid (600mg); Tab Pyrazinamide (1500mg); Tab Ethambutol (1200mg); Tab Rifampicin (450mg) for three times a week for 1 month; followed by Tab Isoniazid (600mg); Tab Ethambutol (1200mg); Tab Rifampicin (450mg) with Pyridoxine 100 mg 3 times a week for 5 months. The duration of treatment was total 8 months and underlying cold abscess of left arm was drained surgically. Response to therapy was noted by marked subjective and clinical improvement noticed in the form of increased range of motion, upto 110 degree at both elbow joint after 3 months of Anti Tuberculosis Therapy.
Biopsy from the erythematous plaque showing: (a) mild hyperplasia of epidermis and dermal infiltration of lymphocytes with multiple granulomas (100x view, H&E stain); (b) Langhans giant cells in dermis (400x view, H&E stain)
Biopsy from puckered scar showing: (a) epidermal hyperplasia with upper dermal granulomas (100x view, H&E stain); (b) Langhans giant cells within granulomas in dermis (400x view, H&E stain)
Discussion
Tuberculosis is one of the commonest chronic granulomatous infections caused by Mycobacterium tuberculosis. The incidence of cutaneous TB is around 5.9 per 1000 population. It comprises only a small proportion (<1%-2%) of all cases of TB [1]. Lupus vulgaris is the most common form of cutaneous TB in India [2]. Erasmus Wilson, for the first time described lupus vulgaris, compared the lesions to ravages of a wolf and used the word ‘lupus’ (Lupus=Wolf). The disease is also called as Tuberculosis Luposa Cutis or Tuberculosis Luposa [3].
Cutaneous TB is classified into TB due to exogenous source, due to endogenous source and Tuberculids. Tuberculous chancre, Warty tuberculosis occurs due to exogenous infection. Scrofuloderma, orificial tuberculosis, military tuberculosis, tuberculous gumma occur due to endogenous infection. Tuberculids include Lichen scrofulosorum, papular or papulonecrotic tuberculide, erythema nodosum and erythema induratum of Bazin. Lupus vulgaris can occur due to both exogenous and endogenous source of infection [4].
Lupus vulgaris is a chronic progressive form of tuberculosis occurring in patients with moderate to high degree of immunity, originating from an underlying tuberculosis focus or through exogenous inoculation or following BCG vaccination [5]. The typical forms of lupus vulgaris are plaque form, ulcerative/ mutilating, vegetative, tumour-like and the papular/ nodular form. In India, lower extremities, especially buttocks are most frequently affected, while the face is the most commonly affected site in western countries with a frequent affliction of the nose and cheeks [3]. In India, relatively low frequency of facial lesions when compared to western world can be attributed to higher temperatures prevailing in most parts of India [3].
Scrofuloderma (SCF) is a type of secondary TB which occurs by contiguous spread from tuberculosis lymph nodes, bones, or joints. These cases presented with discharging sinuses overlying caseating tuberculosis lymph nodes [6].
In our case, Lupus vulgaris (erythematous scaly plaque) as well as scrofuloderma (puckered scar) were suspected considering morphology of the lesions but both the biopsies revealed lupus vulgaris with upper dermal granuloma composed of lymphocytes, plasma cells, epitheloid cells and typical langhans type of giant cell. This shows that histopathological and clinical findings are still very important in diagnosis of cutaneous tuberculosis. Histopathological differentials of tuberculous granulomas can be lupus miliaris disseminatus faciei, lichen scrofulosorum, sporotrichosis, foreign body granuloma, acne rosacea and recidivans type of leishmaniasis but considering clinical scenario and good response with ATT confirmed our diagnosis.
Demonstration of AFB by smear or culture though the gold standard for diagnosis of any patient with tuberculosis, is not feasible in lupus vulgaris as it is a paucibacillary form of cutaneous tuberculosis [7]. Hence latest techniques of molecular diagnosis like PCR should be employed whenever appropriate, so that a definite diagnosis can be made [8]. Delays in initiating therapy in undiagnosed, long-standing cases result in considerable morbidity including squamous cell carcinoma and disfiguring scars [9].
Conclusion
We report this case considering rarity of different morphologies in a same patient as well as numerous lesions and sites involved were not the same as one would expect in Indian subcontinent. It is known fact that tuberculosis can affect an individual from head to toe and from skin to bone. So in developing country like India where tuberculosis is rampant, it should be of prime importance to keep cutaneous tuberculosis as a differential in chronic skin condition with varied presentation.
[1]. Caminero J, Guia de la tuberculosis para medicose specialistas. Paris: International Union againstTuberculosis and Respiratory Diseases 2003 :35-37. [Google Scholar]
[2]. Kumar B, Rai R, Kaur I, Sahoo B, Muralidhar S, Radotra BD, Childhood cutaneous tuberculosis: a study over 25 years from northern IndiaInt J Dermatol 2001 40:26-32. [Google Scholar]
[3]. Padmavathy L, Rao L, Ethirajan N, Krishnaswamy BK, Ulcerative Lupus Vulgaris Of Face: An Uncommon Presentation In IndiaIndian J Tuberc 2007 54:52-54. [Google Scholar]
[4]. Singh G, Kaur V, Singh S, Bacterial infections. In: Valia RG, Valia AR, editorsIADVL Textbook of Dermatology 2008 3rd edBhalani Publishing House:223-51. [Google Scholar]
[5]. Yates VM, Mycobacterial infectionsIn Rook’s Textbook Of Dermatology 2010 318th edWiley-Blackwell:10-29.Tony B, Stephen B, Neil C, Christopher G [Google Scholar]
[6]. Padmavathy L, Rao L, Ethirajan N, Manohar U, Krishnaswamy BK, Scrofuloderma: A clinicopathological and epidemiological studyIndian J Dermatol Venereol Leprol 2008 74:700 [Google Scholar]
[7]. Lucas S, Bacterial diseases. In: Elder DE, Elenitsas R, Johnson BL, Murphy GF, editorsLever’s histopathology of the skin 2005 9th edPhiladelphiaLippincott Williams and Wilkins:551-90. [Google Scholar]
[8]. Chakravarti A, Dhawan R, Shashidhar TB, Sahni JK, Lupus vulgaris of external noseIndian J Tuberc 2006 53:220-22. [Google Scholar]
[9]. Kiedrowicz M, Królicki A, Stanislawa B, Maleszka R, Squamous cell carcinoma arising from radiation-treated lupus vulgaris scarIndian J Dermatol Venereol Leprol 2011 77:253 [Google Scholar]