Vanishing Mandible: A Rare Case Report with Accent to Recent Concepts on Aetio-pathogenesis
Durairaj Duraisamy1, Jai Santhosh Manikandan Veerasamy2, Davidson Rajiah3, Bharathi Mani4
1 Professor, Department of Oral and Maxillofacial Surgery, Tamil Nadu Government Dental College and Hospital, Chennai, India.
2 Post Graduate Student, Department of Oral and Maxillofacial Pathology, Tamil Nadu Government Dental College and Hospital, Chennai, India.
3 Assistant Professor, Department of Oral and Maxillofacial Surgery, Tamil Nadu Government Dental College and Hospital, Chennai, India.
4 Post Graduate Student, Department of Oral and Maxillofacial Surgery, Tamil Nadu Government Dental College and Hospital, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jai Santhosh Manikandan Veerasamy, No. 2, Mosses Street, Eswaran Nagar, Pammal, Chennai – 600075, India.
E-mail: jaisanthoshmanikandan@gmail.com
Massive osteolysis is a rare idiopathic bone disease resulting in progressive destruction of bone. Considering the rarity of encountering this fascinating bone disease, it is often misinterpreted as some other osteolytic disease. Hence, we present a well-documented case of massive osteolysis in a 29-year-old female patient with complete clinical, radiographic, macroscopic and microscopic features along with surgical photographs, which has been effectively managed at our hospital.
Angiomatosis of bone, Disappearing bone disease, Gorham-Stout syndrome, Massive osteolysis, Phantom bone disease
Case Report
A 29-year-old female patient, reported to the out patient department of the hospital with a chief complaint of progressive decrease in mouth opening for the past 2 months. Patient has undergone surgery on the right side of her lower jaw 12 years ago for which she does not have any medical record. Patient had no history of deleterious habits and her family history was unremarkable. On extra oral examination, facial asymmetries with slight depression over both the right and left lower border of mandible were noted [Table/Fig-1].
Patient showing facial asymmetries with slight depression (arrows) over both the right and left lower border of mandible

No symptoms of paraesthesia were present. Tenderness over the left temporomandibular joint and ramus of mandible could be elicited. Patient had restricted mouth opening [Table/Fig-2].
Patient showing restricted mouth opening

Minimal bilateral condylar movements were palpated. There was no associated sinus opening or pus discharge on examination. Intraoral examination revealed missing teeth (namely 41, 42 and 48) with generalized spacing but no carious tooth was present. Blood investigations were within normal limits. Orthopantomograph revealed decreased vertical height of right and left body of mandible and bone resorption involving the ramus and condylar articular surface of left tempero-mandibular joint [Table/Fig-3].
Orthopantomograph reveals decreased vertical height of both left and right body of mandible (orange arrows) as well as bone resorption involving ramus and condylar articular surface of left tempero-mandibular joint (yellow arrow)

CT scan revealed bone resorption involving the ramus and condylar head of left mandible [Table/Fig-4]. The above findings were supported by 3D Computed Tomography [Table/Fig-5].
CT scan reveals bone resorption (arrows) involving the ramus and condylar head of left mandible
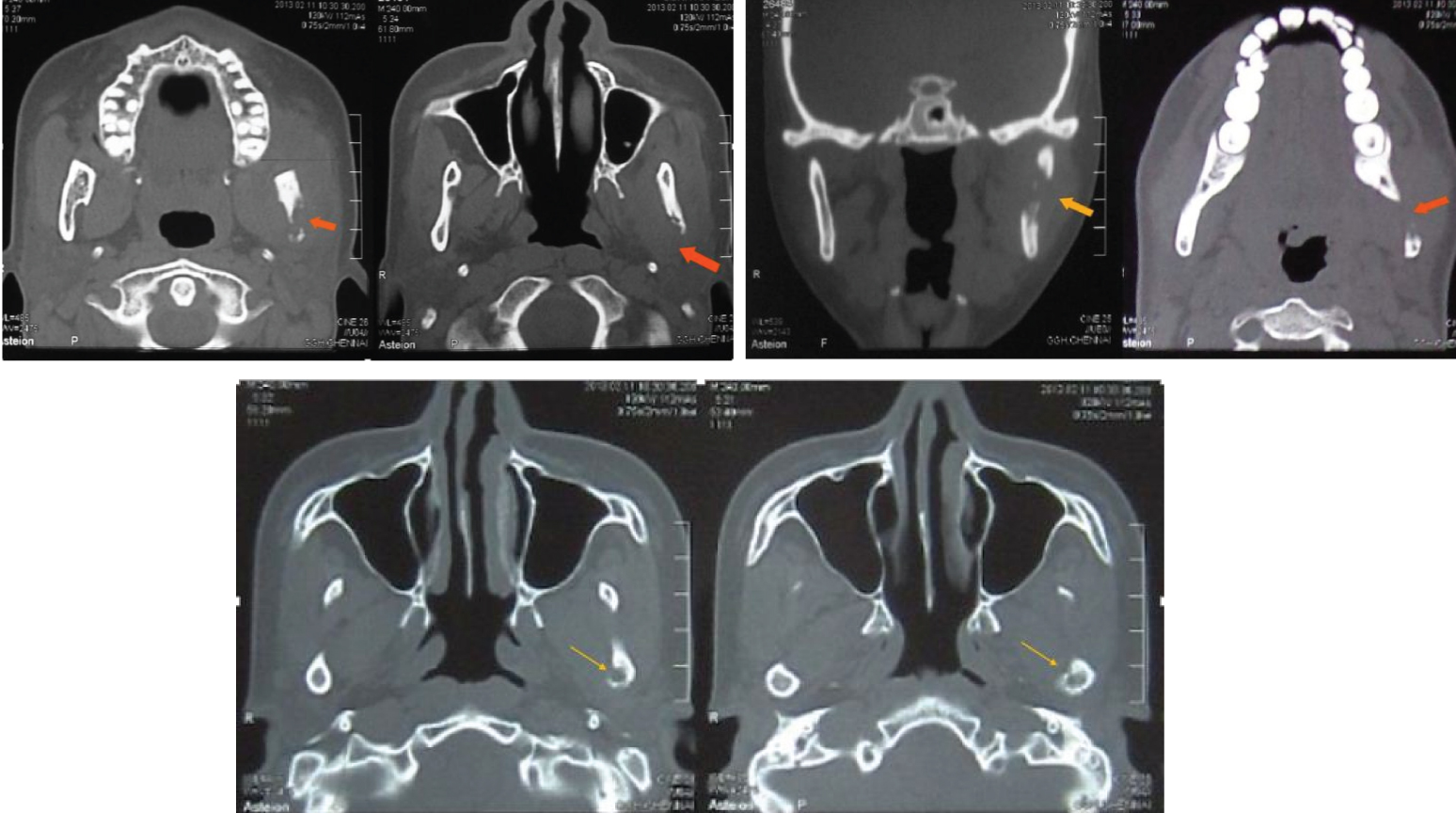
3D construction image reveals bone resorption (arrows) involving the inferior border of right mandible as well as inferior border, ramus and condylar head of left mandible

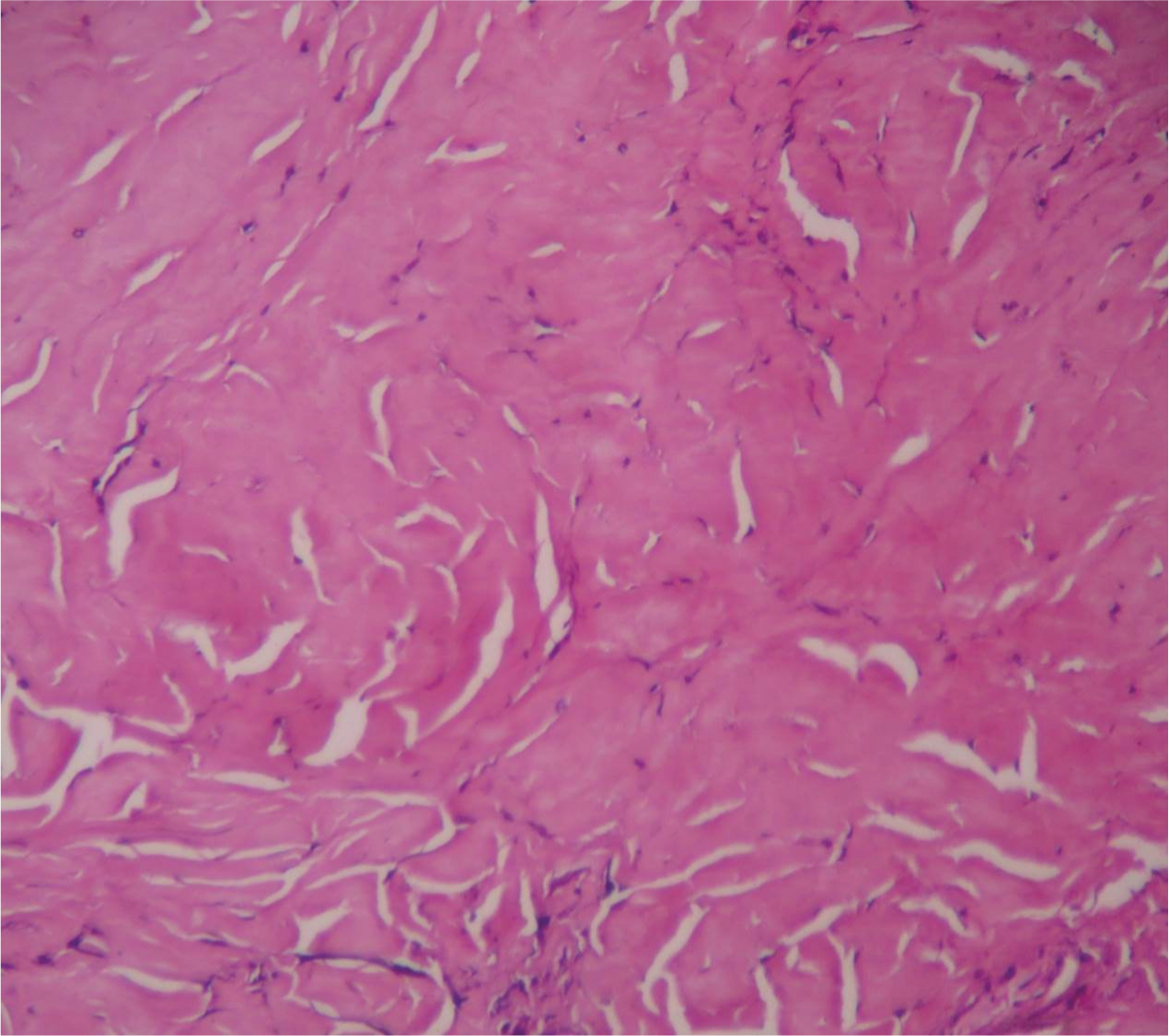
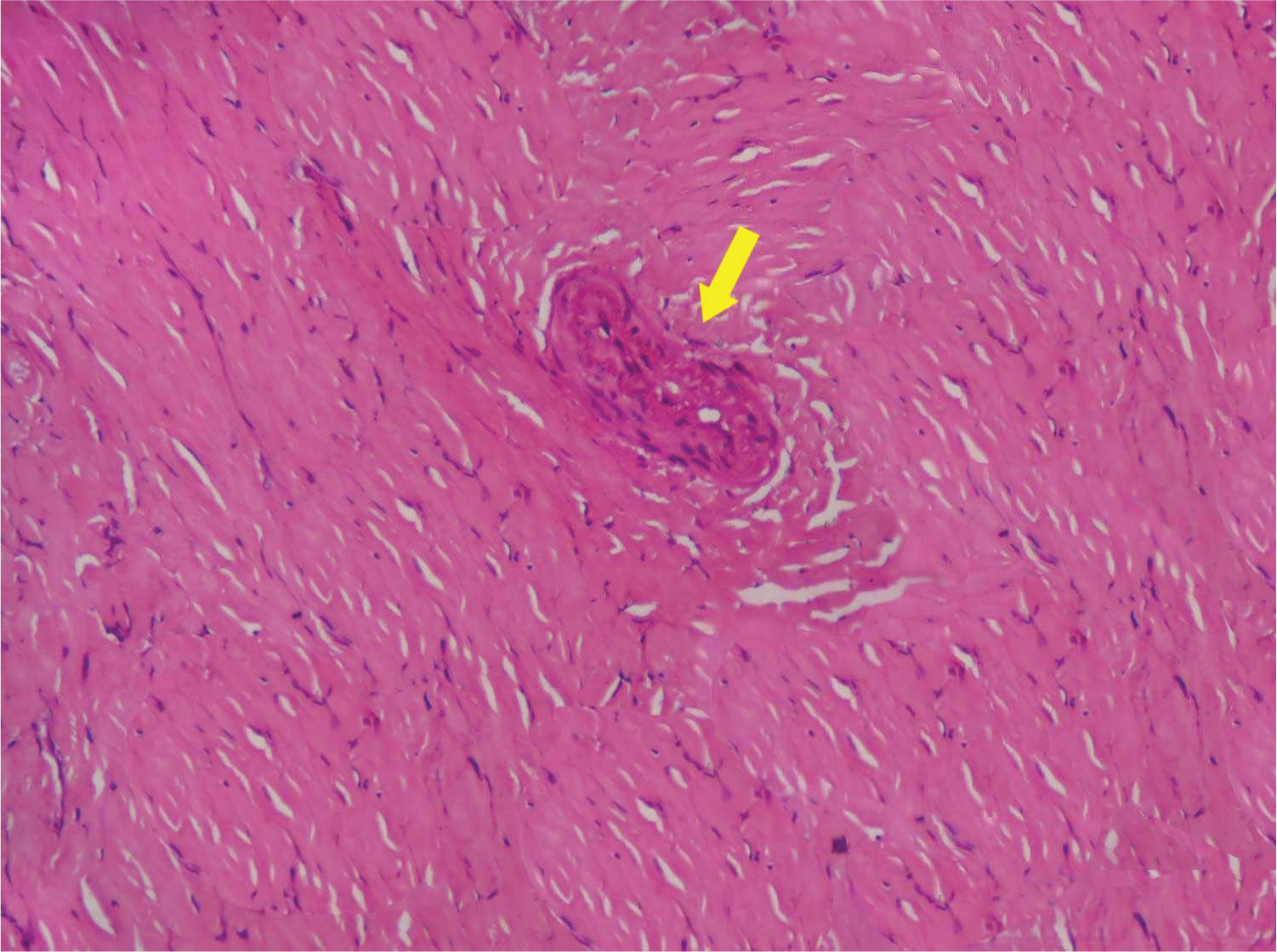
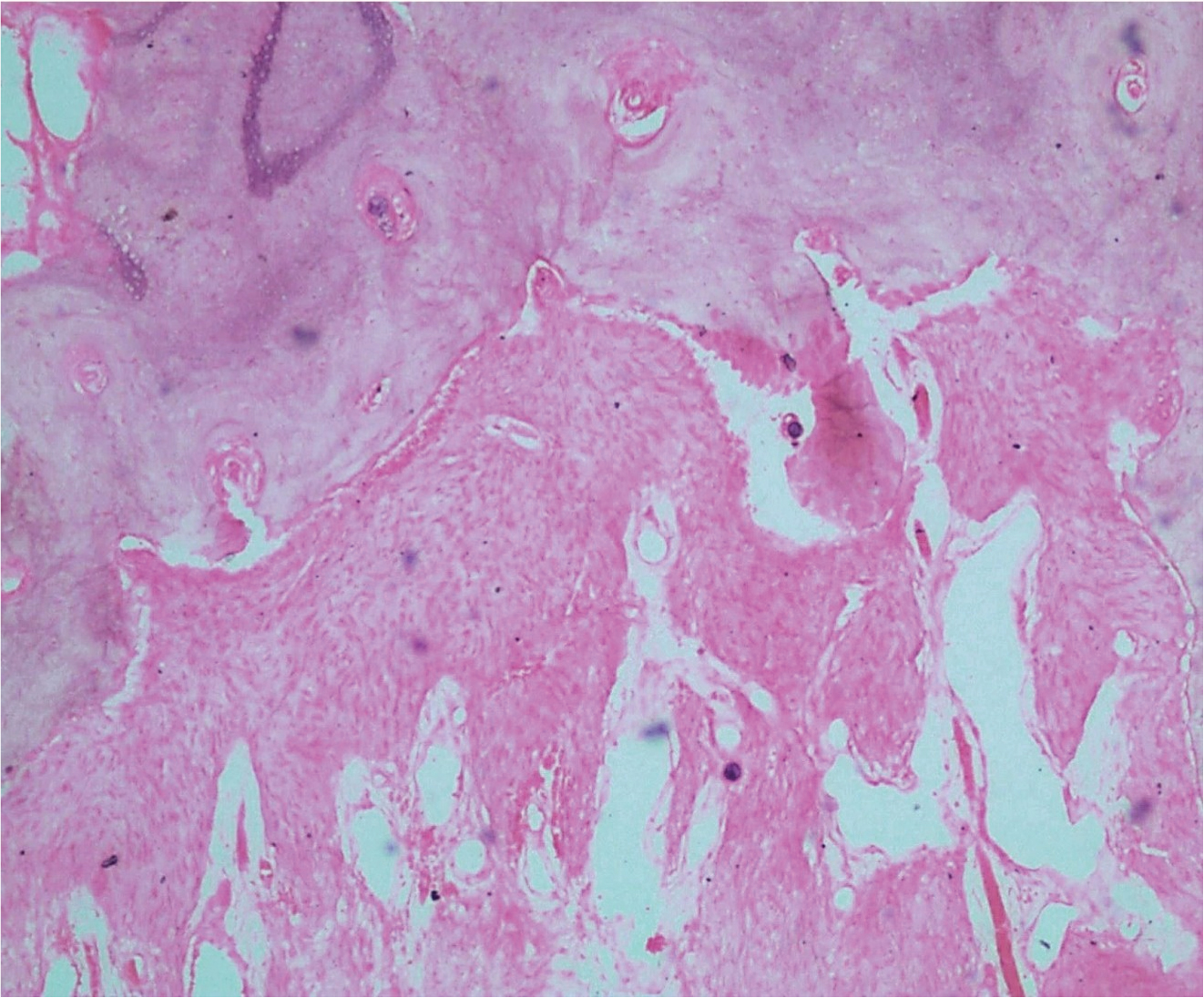
Provisional diagnosis of osteomyelitis of the mandible was made. Patient was given counselling and was provided with various treatment options. An incisional biopsy was performed after obtaining informed consent. On histological examination non-inflammed, densely collagenized and pauci-cellular fibrous tissue [Table/Fig-6] with entrapped blood vessels [Table/Fig-7] was seen in contrast to the features of osteomyelitis. Hence a diagnosis of massive osteolysis was then made correlating with the clinical, radiographic and histolopathological findings.
Histological examination showing densely collagenized and pauci-cellular fibrous tissue (haematoxylin and eosin stain, 10X Magnification)
Histological examination showing entrapped blood vessel (arrow) (haematoxylin and eosin stain, 10X Magnification)
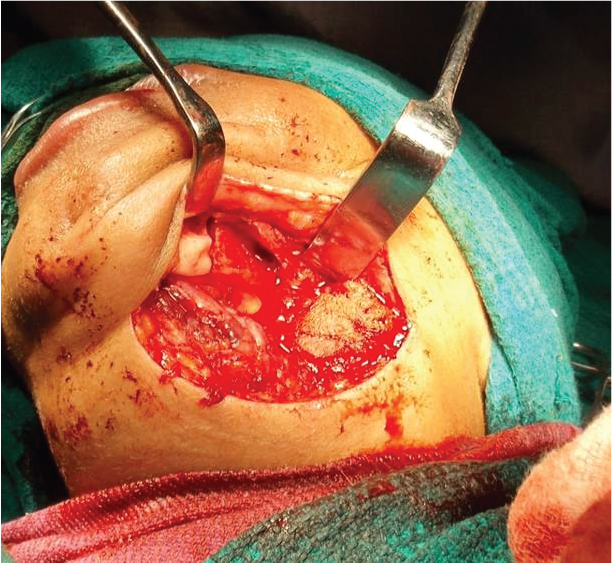
Two months later, after obtaining an informed consent, the patient was taken up for surgery under general anaesthesia. Through left sub mandibular incision access to left mandibular body and ramus was gained. Because of fibrous nature of the tissue it was very difficult to identify fascial planes. After adequate bone exposure, the bone appeared relatively soft and pliable in contrast to the normal bone [Table/Fig-8].
Left sub mandibular incision access to left mandibular body exposing the diseased bone
Hence resection of entire left body and ramus of mandible up to the condyle was accomplished. Gross specimen consisting of resected part of mandible with bone resorption areas [Table/Fig-9], along with fibrous tissue mass [Table/Fig-10] was submitted for histopathological study.
Gross specimen showing buccal and lingual surface of resected mandible with bone resorption (arrows)

Gross specimen showing firm, fibrous mass (along with cut-section) retrieved for histopathology study

On histological examination, non-inflammed, densely collagenous pauci cellular fibrous tissue entrapped with numerous blood vessels was found, confirming the preoperative diagnosis of Massive Osteolysis [Table/Fig-11,12,13]. Review of the patient at the end of 6 month follow up showed adequate mouth opening [Table/Fig-14] and no evidence of any new lesion. Patient referred to prosthodontics department for fabrication of guiding flange. Further management with autogenous bone grafting at a later stage is to be planned.
Histological examination showing non-inflammed, densely collagenized and pauci-cellular fibrous tissue with entrapped blood vessels (arrows). (Haematoxylin and eosin stain, 4X Magnification)

Histological examination showing entrapped blood vessel (arrow). (Haematoxylin and eosin stain, 10X magnification)

Histological examination showing borders of bone at the periphery of the fibrous tissue. (Haematoxylin and eosin stain, 10X Magnification)
Postoperative photograph showing improved mouth opening

Discussion
Massive osteolysis is known by several names such as Vanishing bone disease, Gorham – Stout disease, Morbus Gorham-Stout syndrome, Idiopathic massive osteolysis, Phantom bone disease [1]. Literatures suggest that only a handful of cases (i.e approximately 200 cases) have been reported and out of which only 51 cases involved the face [2], with our case adding to that number. Although two decades have passed, the exact pathology of this disease is poorly understood [2]. There is no evidence of genetic inheritance or associated metabolic or endocrine abnormalities [3]. The lesion in its initial stage, has these unusually wide capillary-like vessels with a sluggish flow that results in a local hypoxic effect and a decreased pH which favours the activity of various hydrolytic enzymes causing bone resorption [2]. Trauma favours bone resorption in this disease through activation of previously silent hamartoma [4] or due to defect in normal neovascularisation of blood clot formed between fractured bone fragments after trauma [5].
It is found recently that cells of monocyte-macrophage lineage (that fasten osteoclastogenesis and angiogenesis) as well as signaling pathway of the PDGFR-b (receptor of the lymphangiogenic growth factor Platelet Derived Growth Factor BB) plays a key role in pathogenesis of massive osteolysis. In the future, research must be directed towards lymphangiogenic pathways, to un-tie many hidden secrets regarding this fascinating disease [6]. Massive osteolysis has a predilection for children and young adults and mostly preceded by history of trauma [7]. But in our case there is no history of trauma except that patient had undergone surgery on the right side of mandible at a younger age. The disease has an insidious onset without pain and advances rapidly until the involved bone is replaced by a thin layer of fibrous tissue [7]. It is predominantly monocentric [4], with spontaneous fracture being the first sign in most cases [2]. Even in this scenario, patient had concern only when there was a progressive restriction for mouth opening since there was no evidence of pain or any other discomfort.
The most commonly affected bones are pelvis, shoulder, scapula, and clavicle [5]. Only in 30% of the patients, maxillo-facial region is affected [2]. In the maxillo-facial region, the mandible is the most frequently affected [4] and mainly involves the mandibular basal and alveolar region [8] and very rarely temporomandibular joint [9]. However in our case along with mandibular basal bone, ramus and articular surface of left condyle were also affected which is quite rare. Generally, the results of laboratory investigation in these patients are completely within normal limits [3], which were documented in our case as well. Radiographic features play a major role in the diagnosis of massive osteolysis. During the initial stages, the lesion is seen as radiolucent foci restricted within the intramedullary or subcortical regions. These radiolucent foci coalesce and eventually involve the cortex at later stages. Computed tomography plays an important role in evaluating the involvement of facial bones and the skull, and can determine any extension into the base of the skull. Radio isotopic scan often demonstrates increased vascularity during initial stages [9].
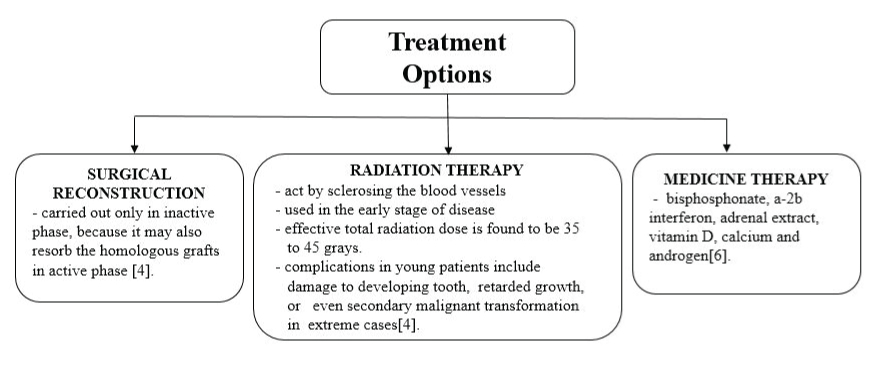
On histopathological examination, lesion in the early stage shows areas of bone resorption characterized by vascular proliferation made up of thin-walled channels that may be capillary or cavernous in nature intermixed with fibrous connective and few chronic inflammatory infiltrates. In the later stages, the areas of bone loss become more collagenized. Our case corresponds to the later stage of the disease as it predominantly shows densely collagenous pauci cellular fibrous tissue entrapped with few blood vessel [3]. Sparcity of osteoclasts, no evidence of repair by new bone formation [3] and absence of areas of active resorption [7] are some of the peculiar features of the disease which correlated with the histopathological findings in our case. Finally to sum up, our case holds good for most of the eight criteria put forth by Heffez et al., [10] for definitive diagnosis of massive osteolysis. The clinical course of massive osteolysis is generally unpredictable, as in some patient it may get arrested and in some patients it may progress to complete disappearance of bone [6]. Treatment modalities illustrated in flow chart below [Table/Fig-15].
Flow chart to demonstrate treatment options
Diagnosis of such poorly understood disease is in itself is very challenging for a clinician since the patient may complain of a vague pain or progressing weakness. In this particular case features of insidious onset of restricted mouth opening, absence of infectious or malignant component, reduced vertical height of mandibular ramus, radiolucent areas involving cortex of mandible and a normal blood investigation gave a high index of suspicion of Gorham’s disease [2], but contrasting features of female predilection, negative history of trauma, sole involvement of mandible, bone loss extending upto the condyle, made the diagnosis of this case little tricky and necessitated a histopathological confirmation. Surgical management of this case has yielded positive response so far, with no evidence for any newer lesions at the end of 6 months follow up.
Conclusion
It is unfortunate that with so many advances in the medical field, there is no effective treatment regime for massive osteolysis. Hence it is prudent for every oral pathologist to scrutinize all the information obtained from patients before arriving at final diagnosis to prevent misdiagnose of this destructive bone disease, which is actually not rare as we perceive. Even though clinical and radiological finding helps in diagnosis, considering the rarity of the disease, a histopathological diagnosis is a mandatory, to proceed towards a more definitive management.
[1]. Dipak V, Gorham’s dieases or massive osteolysisClin Med Res 2005 3:65-74. [Google Scholar]
[2]. Saify FY, Gosavi SR, Gorham’s disease: A diagnostic challengeJOMFP 2014 18(3):411-14. [Google Scholar]
[3]. Nevile BW, Bouquot JE, Damm DD, Allen CM, Oral and maxillofacial pathology 2009 3rd edPhiladelphiaW.B. SaundersChapter 14, Bone pathology; Pp.613-677 [Google Scholar]
[4]. Nagaveni NB, Radhika NB, Umashankara KV, Satisha TS, Vanishing (Disappearing) bone disease in children-A reviewJ Clin Exp Dent 2011 3(4):1-8. [Google Scholar]
[5]. Jackson JBS, A boneless armBoston Med Surg J 2000 18:368-69. [Google Scholar]
[6]. Nikolaou VS, Chytas D, Korres D, Efstathopoulos N, Vanishing bone disease (Gorham-Stout syndrome): A review of a rare entityWorld J Orthop 2014 5(5):694-98. [Google Scholar]
[7]. Rajendran R, Sivapathasundharam B, Shafer’s Textbook of oral pathology 2012 7th edNew DelhiElsevierChapter 17, Disease of bone and joints; Pp.685-760 [Google Scholar]
[8]. Kiran DN, Anupama A, Vanishing bone disease: A reviewJ Oral Maxillofac Surg 2011 69:199-203. [Google Scholar]
[9]. Raghuveer HP, Jayalekshmy R, Gorham’s massive osteolysis of the mandible-a progressive radiographic presentationDentomaxillofac Radiol 2009 38:292-95. [Google Scholar]
[10]. Heffez L, Doku HC, Carter BL, Feeney JE, Perspectives on massive osteolysis. Report of a case and review of the literatureOral Surg 1983 55:331-43. [Google Scholar]