The large intestine and Anal canal are sites for broad array of non- neoplastic and neoplastic diseases, which at times, can lead to serious complications. They can be sites for infections, vascular disorders, ulcers, various inflammatory conditions and neoplasms [1]. Epithelial tumours are major cause of morbidity & mortality. Colorectal cancer is the fourth ranking cancer worldwide, accounting for approximately 9% of all cancers [2]. Adenocarcinomas are the commonest malignancies arising in the colorectal region, other being carcinoid, anal zone carcinoma & melanoma. Non neoplastic polyps are classified as hyperplastic, hamartomatous, juvenile & Peutz jeghers polyp, inflammatory & lymphoid polyp. Other benign conditions are adenoma, lipoma, neuroma, angioma, etc.
Hirschsprung disease, enterocolitis & various ulcers like amoebic and inflammatory bowel disease (IBD), can cause septicaemia, perforation peritonitis & electrolyte imbalance. Inflammatory bowel diseases like Crohn’s disease & Ulcerative colitis are premalignant conditions, hence their early diagnosis is necessary to avoid further consequences & for proper treatment. Bowel infarction is a grave disorder that imposes 50-70% death rate. If not detected early patient may progress to shock & vascular collapse.
Both macroscopic and microscopic appearance when correlated with clinical data helps in a definitive diagnosis of the lesion, which helps in early treatment and better outcome of the patient.
The present study was conducted to study the large intestinal lesions including Anal canal, correlate them with clinical data and to compare the findings with other studies.
Materials and Methods
This three years retrospective and two years prospective (5 years) study included 124 large intestinal & 64 Anal canal lesions. For retrospective study, requisition forms, blocks and slides were retrieved from the archives. Clinical details were obtained and maintained according to the proforma. The blocks were restained with H&E and also for special stains whenever required for re-establishing the diagnosis. The study was approved and permitted by ethics committee of the institution.
All biopsies and resected specimen received were immediately fixed in 10% formalin for 24 hours. Gross features of specimen were noted and multiple sections were taken. Routine tissue processing was done. Special stains like Periodic Acid Schiff (PAS) and Reticulin were done whenever necessary along with immunohistochemistry (IHC).
After detailed study of the sections under the light microscope the final diagnosis was given. Then, data was analysed and results were obtained.
Results
For the ease of interpretation, the results were divided in to Lesions of large intestine and Anal canal. Out of 188 cases, 124 were from large intestine and 64 from Anal canal.
Lesions of Large intestine
Among large intestinal lesions, neoplastic lesions (77 cases) were found to be common. Nine cases, which were suspected cases of malignancies of the colon and rectum, were included in the study and were classified as biopsy specimen inadequate for accurate interpretation. Among the non neoplastic lesions, maximum cases were of Acute self limiting colitis (14 cases). Infectious colitis included one case each of Amoebic and strongyloid stercoralis induced colitis. Amongst the neoplastic lesions, malignant lesions (68 cases) constituted the maximum number of cases. In benign neoplastic lesions, maximum were of juvenile polyp (06 cases) and adenocarcinoma (61 cases) outnumbered all malignant lesions [Table/Fig-1].
Distribution of lesions of large intestine
| Sr.no | Lesion | No. of cases | Percentage |
|---|
| 1 | Non – neoplastic | 38 | 30.65 |
| Hirschsprung’s disease | 03 | 7.89 |
| Acute self limiting colitis | 14 | 36.84 |
| Infectious colitis | 02 | 5.26 |
| Ulcerative colitis | 03 | 7.89 |
| Tuberculosis | 02 | 5.26 |
| Ischemic colitis | 12 | 31.58 |
| Pseudomembranous colitis | 02 | 5.26 |
| 2 | Neoplastic | 77 | 62.09 |
| Benign | 09 | 11.69 |
| Juvenile polyp | 06 | 66.67 |
| Adenomatous polyp | 02 | 22.22 |
| Hyperplastic polyp | 01 | 11.11 |
| Malignant | 68 | 88.31 |
| Adenocarcinoma | 61 | 89.71 |
| Squamous cell carcinoma | 01 | 1.47 |
| Lymphoma | 02 | 2.94 |
| Malignant melanoma | 01 | 1.47 |
| Vascular Leiomyosarcoma | 01 | 1.47 |
| Metastasis to large bowel | 02 | 5.88 |
| 3 | Inadequate biopsy | 09 | 7.26 |
| Total | 124 | 100 |
The non-neoplastic lesions were common in 3rd to 6th decade with male preponderance and male to female ratio of 2.4:1.
Among neoplastic lesions, equal sex incidence was found in malignant cases, while in benign lesions M:F was 2:1. Benign neoplastic lesions were common in 1st decade and malignant were found to be common in 4th to 7th decade.
Among Adenocarcinomas the most common histologic type was moderately differentiated adenocarcinoma (35 cases) [Table/Fig-2].
Distribution of histological types of Adenocarcinoma
| Histological type | No. | Percentage |
|---|
| Well differentiated adenocarcinoma | 11 | 18.03 |
| Mod- differentiated adenocarcinoma | 35 | 57.37 |
| Poorly- differentiated adenocarcinoma | 01 | 1.64 |
| Mucin secreting adenocarcinoma | 11 | 18.02 |
| Signet ring cell adenocarcinoma | 03 | 4.92 |
| Total | 61 | 100 |
Lesions of Anal canal: Among Anal canal lesions, Non-neoplastic lesions (55 cases) were found to be common. In the present study all the nine neoplastic cases were malignant [Table/Fig-3].
Distribution of lesions of Anal canal
| Sr.no | Lesion | No. of cases | Percentage |
|---|
| 1 | Non – neoplastic | 55 | 85.94 |
| Fistula in ano | 33 | 60.00 |
| Hemorrhoides | 19 | 34.55 |
| Hypertrophied anal papillae | 03 | 5.45 |
| 2 | Neoplastic | 09 | 14.06 |
| Squamous cell carcinoma | 05 | 55.56 |
| Adenocarcinoma | 03 | 33.33 |
| Malignant melanoma | 01 | 11.11 |
| Total | 64 | 100 | |
Among Non-neoplastic lesions Fistula in ano (33 cases) was commonest and in malignant neoplastic lesions squamous cell carcinoma (05 cases) was found to be common.
In anal canal lesions, the most common age group affected was 4th-7th decade.
Male preponderance was seen in non neoplastic lesions with M:F ratio of 4.2:1, while in neoplastic lesions nearly equal sex incidence was observed.
Bleeding per rectum (131 cases) was found to be the most common symptom among patients of large intestinal lesions followed by constipation (101 cases), pain abdomen (81 cases) and weakness (52 cases) [Table/Fig-4].
Distribution of the large intestinal lesions with respect to symptoms (including anal canal)
| Symptoms | Number of cases | Percentage |
|---|
| Bleeding per rectum | 131 | 69.68 |
| Constipation | 101 | 53.72 |
| Pain abdomen | 81 | 43.09 |
| Weakness | 52 | 27.66 |
| Diarrhoea | 46 | 24.47 |
| Mass per abdomen | 35 | 18.62 |
With the available data and proforma collected, in the present study we observed that among malignant lesions of the large intestine including anal canal, 71.43% were non vegetarians.
Discussion
Lesions Of Large Intestine: In the present study there were 38 cases of non-neoplastic lesions, 77 neoplastic lesions and 9 were inadequate biopsies.
Non Neoplastic Lesions
1) Hirschsprung Disease : Three cases (7.89%) of Hirschsprung disease were noted. One was a two days old neonate and others, 11 years male and 5 years female. USG abdomen of them showed dilated bowel loops.
Cecilia & Rescorla et al., stated that 80% cases of Hirschsprung disease are male with 80% of cases diagnosed during first year of life & 10% first present in adults. Most of them present with severe constipation [3,4].
Zaid F et al., in their study found that the age range of Hirschsprung disease patient was from 1 day to 13 yrs with peak during the neonatal period [5]. Most of the patients presented with constipation and the remaining (6%) presented with other congenital anomalies.
On histology, in Hirschsprung disease, the transitional area in the affected bowel shows abnormally small ganglion cells.
2) Acute self limiting colitis: In the present study 14 cases (36.84%) of acute self limiting colitis were noted. Most of the patients presented with pain in abdomen, diarrhoea and per rectal bleeding. The stool cultures of most of the cases were bacteriologically negative.
Mandal BK et al., and Haboubi et al., found that patients who presented with diarrhea, had features of acute self limiting colitis with wide age range and male preponderance. Our findings were similar to above studies [6,7].
3) Infectious colitis: Two cases (5.26%) of infectious colitis were seen. One was amoebic and the other was colitis due to Strongyloid stercoralis.
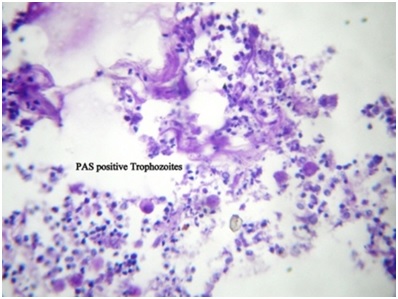
a) The patient of amoebic colitis was a 30 years male presented with bleeding per rectum, intermittent diarrhoea and constipation along with acute pain in abdomen. Histopathology shows denudation of the surface epithelium with dense and diffuse infiltration by mixed inflammatory cells along with oedema of the mucosa. These trophozoites were PAS positive [Table/Fig-5].
Photomicrograph showing PAS positive Trophozoites of Entamoeba Histolytica (PAS; 10x X 10x).
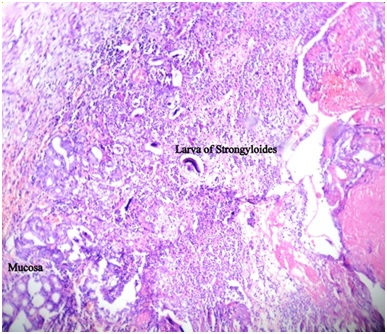
Cecilia stated that amoebiasis can affect individuals of all ages [8]. b) The patient with infestation of the colon by Strongyloid stercoralis was a 40 years male presented with pain in abdomen and diarrhoea with signs of intestinal obstruction.
On histopathologic examination many larval forms of the helminth were seen in the submucosa with ooedema and diffuse and dense infiltration by mixed inflammatory cells [Table/Fig-6].
Photomicrograph showing numerous Strongyloidal larva in mucosa and submucosa of the large intestine with mixed inflammatory infiltrate (H&E; 10x X 10x)
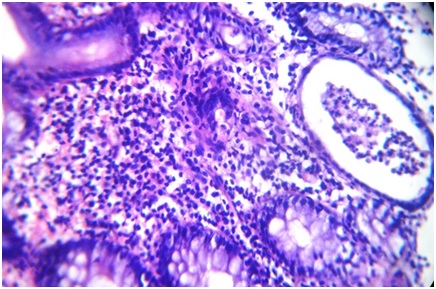
4) Ulcerative colitis: In our study three cases, two females & one male of ulcerative colitis were seen. They presented with pain in abdomen, diarrhoea and per rectal bleeding. Histology showed loss of tubules with cryptitis and crypt abscesses [Table/Fig-7].
Photomicrograph of Ulcerative Colitis of large intestine showing Crypt abscess (H&E; 40x X 10x)
Price AB et al., stated that ulcerative colitis is a disease confined to the large intestine with a peak incidence in the 3rd decade [9].
Kirsner JB et al., stated that both Ulcerative Colitis and Crohn’s disease are rare in developing countries [10].
Sood A et al., in their study in Punjab found that the mean age of presentation of ulcerative colitis was 35.32 years with the commonest symptoms being pain in abdomen and per rectal bleeding [11]. Our findings match with the above studies.
5) Ischemic colitis: In the present study 12 cases of ischaemic colitis were noted. The most common symptom was pain in abdomen followed by constipation & bleeding per rectum. The age range was 25–75 years with M:F :: 7:5. Histology of all showed transmural haemorrhagic necrosis.
Kontagianni A et al., also found transmural ischaemic necrosis in whole of the population [12].
Antolovic D et al., stated that the clinical spectrum ranges from moderate self limiting to severe forms with full thickness necrosis requiring urgent surgical treatment [13].
Benign Neoplastic Lesions of Large Intestine
In our study out of 77 cases of neoplastic lesions, nine cases were of benign nature. The 9 cases included 6 of juvenile polyps, 2 of adenomatous polyps and a case of hyperplastic polyp.
a) Juvenile polyp: In the present study of 6 cases of juvenile polyps, the most common symptom was per rectal bleeding. All the polyps were found in rectum.
Roth SI et al., and Dajani YF et al., found rectum as the most common site for Juvenile polyps [Table/Fig-8] [14,15].
Comparison of clinicopathological features in Juvenile polyp.
| Roth SI et al., (1963) | Dajani YF et al., (1984) | Tony J & Harish K et al., (2007) | Present study (2010) |
|---|
| Age range (years) | 11 mnts-61 yrs | 7 mnts - 33yrs | 4 – 28 yrs | 4 – 62 yrs |
| M : F ratio | 2.9 : 1 | 2 : 1 | 1.4:1 | 1 : 1 |
| Rectal bleeding | 80 % | - | - | 100% |
| Site – rectum | 76% | 96.5 % | 66.67% | 100% |
Histological study showed cystically dilated glands, few of which show mucous in their lumen. Stroma was oedematous and showed infiltration by mononuclear cells. The glands were devoid of atypical features.
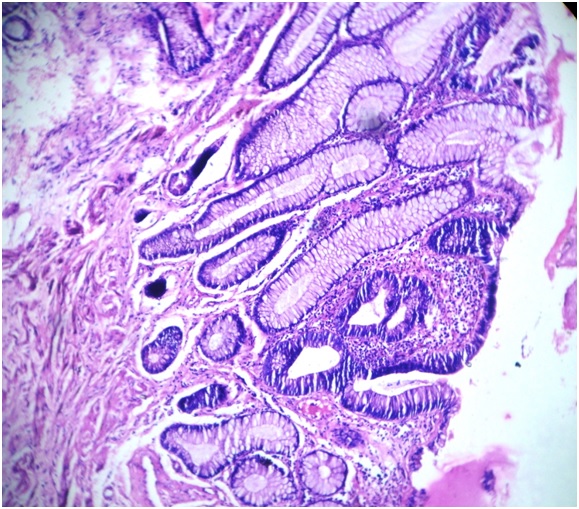
b) Adenomatous polyp: In the present study 2 cases of adenomatous polyp in sigmoid colon were observed. Both were males less than 30-year-old, presented with per rectal bleeding and diarrhoea. On histology one showed tubular adenoma with dysplasia while the other showed tubulo – villous pattern [Table/Fig-9].
Photomicrograph showing Adenomatous polyp with dysplasia (10x X 40x)
Konishi F et al., in their study of colorectal adenomas found that 81 % were tubular adenomas while only 3% were villous of the villous type [16]. An 88% of tubular adenomas showed mild dysplasia while only 4% showed severe dysplasia.
Tony J and Harish K et al., found that in Southern India adenomatous polyps were the most common polyps (79.8%) in the age group of 23-82 years with M:F ratio of 2.5:1 [17]. They also found severe dysplasia in 12% of tubular adenomas and 43% of villous adenomas.
c) Hyperplastic (Metaplastic) polyp: Only one case of hyperplastic polyp in rectum of 60 year male patient was noted in our study.
William’s GJ et al., in their study on metaplastic polyps found that they commonly presented in the age group of 19-85 years [18].
Tony J and Harish K et al., found that hyperplastic polyp constituted 8.8% of all the colorectal polyps [17].
On histology the hyperplastic polyp showed elongated colonic crypts with upper half of crypt showing intraluminal papillary in folding giving rise to saw toothed appearance.
Malignant Neoplastic Lesions of Large Intestine
In the present study 68 cases (88.31%) of malignant lesions were seen. The most common symptom was bleeding per rectum (63.83%) followed by constipation, pain in abdomen and diarrhoea. The most common age group affected was from 4th to 7th decade with equal sex incidence. Adenocarcinoma constituted the maximum number of cases i.e. 61 cases (89.71%). Followed by two cases (2.94%) of lymphoma and one case (1.47%) each of squamous cell carcinoma, malignant melanoma and vascular leiomyosarcoma. Two cases (5.88%) of metastasis to large bowel were also noted.
Adenocarcinoma: Caliskan C et al., in their study found moderately differentiated adenocarcinoma as the most common type [19] [Table/Fig-10].
Comparison of Histological types of Adenocarcinoma
| Histologic types | Caliskan C et al.,(2010) (n = 448) | Present study(2010) (n = 61) |
|---|
| Well differentiated | 13.16% | 18.03% |
| Moderately differentiated | 56.02% | 57.37% |
| Poorly differentiated | 11.16% | 1.64% |
| Mucinous | 14.06% | 18.64% |
| Signet ring | 2.23% | 4.92% |
Shah A et al., in their study of 107 cases of colorectal carcinoma found that 72% of the cases were of well differentiated type while mucinous carcinoma constituted 20% of the cases [20].
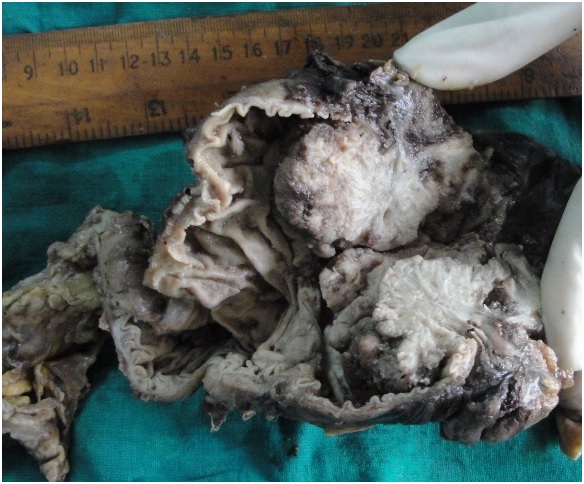
On gross well differentiated adenocarcinoma show constrictive ring [Table/Fig-11] and histology shows well formed glands lined by neoplastic cells and infiltrating the muscularis propria.
Gross specimen of large intestine showing constrictive growth

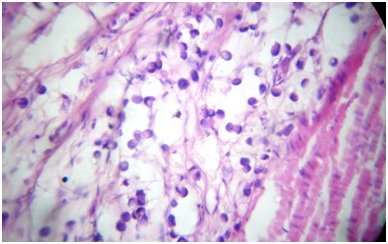
On gross mucinous carcinoma shows fungating mass [Table/Fig-12] and on histology shows tumour cells floating in mucinous pools [Table/Fig-13].
Gross specimen of rectum showing fungating mass with gelatinous cut surface
Photomicrograph of mucinous adenocarcinoma showing tumour cells floating in mucinous pools (H&E; 10x X 40x)
Rasool A et al., and Caliskan C et al., observed that colorectal adenocarcinoma most commonly affects the persons in the age group of 41-70 years [19,21].
Lymphoma: In the present study two cases (2.94%) of lymphomas of colon were observed.
One case was of 19-year-old male and the other case was of a 10-year-old female. Clinically there was generalised lymphadenopathy and marrow showed infiltration. Hence the patients were diagnosed to have a secondary malignant lymphoma of colon.
In both the cases, histology showed diffuse large cell type of Non Hodgkin’s lymphoma.
Nirmala V et al., in their study found that primary malignant lymphomas are rare in colon [22].
Malignant melanoma: In the present study one case (1.47%) of malignant melanoma in 58-year-old female was seen.
Nicholson AG et al., in their study found that primary malignant melanomas of rectum are rare [23].
In the present study, among malignant neoplasms of large intestine, 71.43% were non vegetarians indicating that non vegetarians are more prone for colon malignancies.
Anwar S et al., in their study found that the dietary factors associated with colorectal carcinoma were low fiber contents of food, high meat, smoked foods, high fat diet, increase in refined tin packed food and juices, inadequate intake of fruits and vegetables and wide spread use of preservatives and pesticides [24].
Lesions of anal Canal
In the present study 64 cases (21.33%) of anal canal were observed. Out of 64 cases, 55 cases (85.94%) were non-neoplastic while nine cases (14.06%) were neoplastic. In the neoplastic lesions all the cases were malignant.
1) Non neoplastic lesions: In the present study 55 cases (85.94%) of non–neoplastic lesions were seen. In non – neoplastic lesions 33 cases (60%) were fistula in ano, 19 cases (34.55%) were haemorrhoids and three cases (5.45%) of hypertrophied anal papillae.
2) Malignant neoplastic lesions of anal canal: In the present study 9 cases (14.06%) of tumours of anal canal were noted. Out of 9 cases, 5 cases (55.56%) were of squamous cell carcinoma, three cases (33.33%) were of adenocarcinoma and one case (11.11%) was of malignant melanoma.
In the present study squamous cell carcinoma constituted upto 55.56%. the age range of anal tumours was 4th –7th decade with F:M ratio of 1.25:1.
Klas et al., in their study found that 74% of anal tumours were squamous cell carcinoma [Table/Fig-14] [25].
Comparison of Histological types of Anal tumours
| Histological types | Klas et al.,(1999) (n=192) | Present study(2010) (n =9) |
|---|
| Squamous cell carcinoma | 74 % | 55.56% |
| Adenocarcinoma | 19% | 33.33% |
| Malignant melanoma | 4% | 11.11% |
Morson BC and Volkastadt H in their study of malignant melanoma of the anal canal found that the average age of presentation of malignant melanoma of the anal canal is 59 years [26]. Ramakrishnan AS et al., in his study of Anorectal melanomas found that the average age of melanoma was 53 years [27]. Histologically the tumour is composed of large polygonal cells having pleomorphic hyperchromatic nuclei with prominent eosinophilic nucleoli and moderate amount of cytoplasm. At places the melanin pigment is seen intracellularly and also extracellularly.
Conclusion
This study concludes that various types of lesions occur in the Large intestine and Anal canal affecting the persons from early childhood to late adulthood. Most of the lesions present vaguely which prevent their early diagnosis and treatment leading to grave complications. So this study emphasises the need for early diagnosis of the disease through histopathology, which when correlated clinically will help the surgeon/clinician to implement the appropriate treatment and improve the survival of the patients.