Pneumonia is one of the leading infectious causes of mortality and morbidity worldwide. While Streptococcus pneumoniae still remains the most common cause of Community acquired pneumonia, atypical respiratory pathogens account for 30 – 40% of these infections [1]. The three most important atypical pathogens are Mycoplasma pneumoniae, Chlamydophila pneumoniae and Legionella pneumophila. As infections due to atypical pathogens do not present with classical signs and symptoms of pneumonia they are often underdiagnosed. Patient may develop associated complications like acute respiratory distress syndrome and respiratory failure. The literature regarding the frequency and prevalence of atypical pneumonia, particularly in the developing countries like India is not very vast. Mycoplasma pneumonia and Chlamydophila pneumonia are also implicated in the pathogenesis of Bronchial Asthma and they often cause secondary infections in individuals with Chronic Obstructive Pulmonary Diseases [2]. Apart from respiratory infections Chlamydophila pneumoniae is also thought play a role in Atherosclerosis and multiple sclerosis [3]. From patient point of view treatment failure frequently happens as these pathogens do not generally responds to beta lactam antibiotics which are the mainstay for empirical treatment [3]. With this background in mind the study was undertaken to find out the prevalence of atypical pathogens causing lung parenchymal infections.
Materials and Methods
A cross-sectional period study was done in the Department of Microbiology, Sri Ramachandra University, Chennai, India from March 2013 to September 2014, after obtaining Institutional Ethics Committee approval for patients consent and conduction of study (Ref:CSP-MED/13/OCT/09/94). A total of 107 patients with clinical suspicion of atypical pneumonia during the study period were enrolled. Patients on ventilator and having classical signs and symptoms of pneumonia were excluded from the study.
The presence of atypical pathogens Mycoplasma pneumoniae, Chlamydophila pneumoniae and Legionella pneumophila were screened from the patient’s sample. Respiratory samples in the form of sputum, broncheoalveolar lavage (BAL) and non- Broncheoalveolar lavage (Non-BAL) were used cultivation of Mycoplasma pneumoniae and Legionella pneumophilia. Urine specimen was used for the detection of Legionella antigen. Serum samples were used for the detection of Mycoplasma pneumoniae IgM and Chlamydophila pneumoniae IgM antibodies.
Mycoplasma pneumoniae
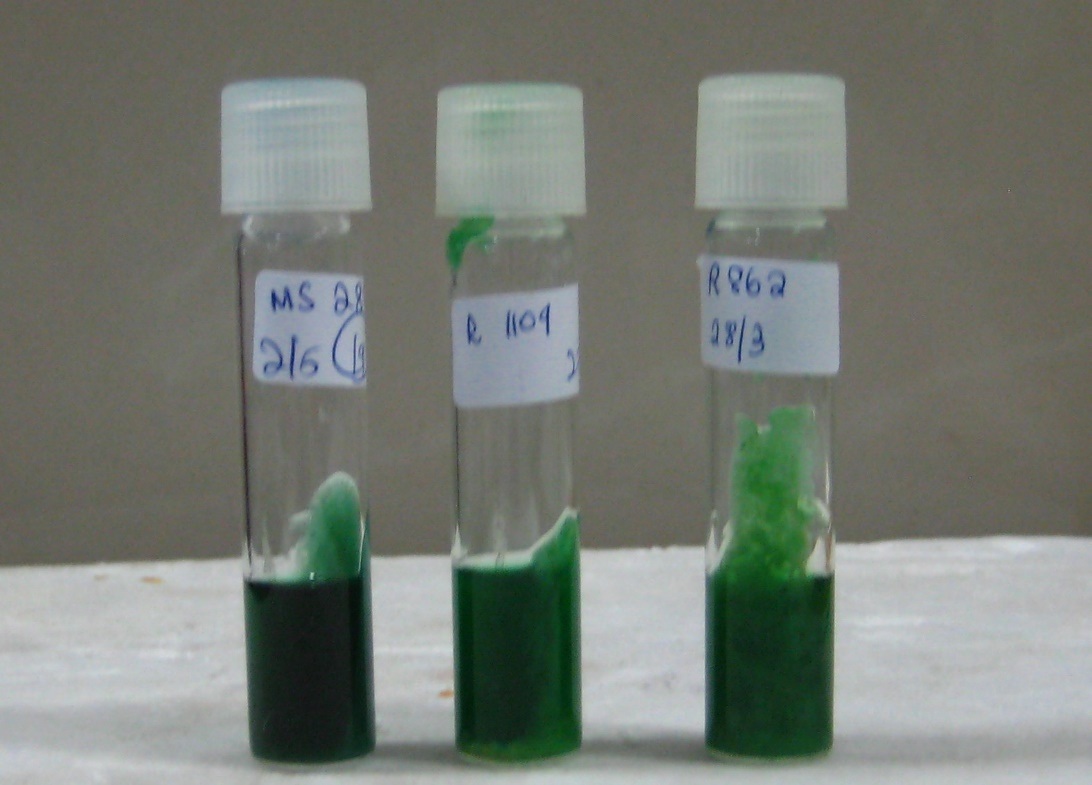
Culture: Respiratory samples were decontaminated before inoculation into the screening medium, Methylene Blue Glucose Biphasic medium [Table/Fig-1], incubated at 37°C under 5% CO2 and reading was taken at regular intervals. The tubes not showing any color change after seven days were sub-cultured for the isolation of Mycoplasma pneumoniae into pleuro pneumoniae like Organism medium (PPLO) (obtained from Hi Media, Mumbai, India), and incubated for two weeks .
Methylene Blue Glucose Biphasic Agar
Serology: The presence of IgM antibody was detected from the serum by ELISA. (EUROIMMUN, Medizinesche Labordiagnostika AG)
Legionella Pneumophilia
Culture: Respiratory samples were inoculated into 5% sheep blood agar and Buffered Charcoal Yeast Extract (BYCE) Agar (obtained from Hi Media, Mumbai, India), incubated at 37°C under 5% CO2 for 7 days.
Serology: Presence of Legionella antigen in the urine was detected by ELISA using kit procured from DRG Instruments GmbH, Germany.
Chlamydophila pneumoniae
Serum samples were used for the detection of IgM antibodies against Chlamydophila pneumoniae by ELISA kit procured from (EUROIMMUN)
Results
A total of 107 patients were enrolled in this study. The study group included 41 women and 66 men. The mean age was 44.42 years. The patient’s demographic data is shown in [Table/Fig-2]. All patients were adults. Among the 107 samples screened, 13 (12.1%) were positive for antibodies against atypical pathogens. Out of which 7 (6.5%) had IgM antibodies against Mycoplasma pneumoniae and the rest 6 (5.6%) had Chlamydophila pneumoniae IgM antibodies. All the samples were culture negative for Mycoplasma pneumoniae and Legionella pneumophila. Urinary antigen detection for Legionella pneumophila was also negative in patients. The results of the study are tabulated in [Table/Fig-3].
| Age in years | Male | Female |
|---|
| 18 - 25 | 6 | 6 |
| 26 - 35 | 15 | 13 |
| 36 - 50 | 22 | 6 |
| 50 - 65 | 13 | 13 |
| >65 | 10 | 3 |
Culture and Serology results
| Atypical Pathogen | IgM Antibody | Antigen | Culture |
|---|
| Positive | Negative | Positive | Negative | Growth | No Growth |
|---|
| Mycoplasma pneumoniae | 7(6.5%) | 100(93.5%) | - | - | 0 | 107(100%) |
| Chlamydophila pneumonia | 6(5.6%) | 101(94.4%) | - | - | 0 | 107(100%) |
| Legionella pneumophila | - | - | 0 | 107 | 0 | 107(100%) |
Discussion
Globally the incidence of atypical pathogens in the community acquired pneumonia is 22% and in Asia it is 20% [4]. The incidence of atypical pneumonia in various study is tabulated in the [Table/Fig-4]. meta-analysis by Bartlett J G [4] has also shown that in outpatients mainly Mycoplasma was seen as the common atypical pathogens whereas in the patients who were in need of admission and intensive care was mainly due to Chlamydia pneumoniae. Atypical pneumonia because of the unusual clinical presentation often go undiagnosed, and a high index of suspicion is necessary to clinch the diagnosis. We evaluated the etiology of clinically diagnosed atypical community acquired pneumonia in adults. Our study showed 12.1% of patients positive for atypical pathogens, whereas, an Asian study by Ngeow Y F et al., [5] and his colleagues reported 21.2 % atypical pathogens. Lui G et al., [6] in his study among the hospitalized patients reported 11.2% (n=1193) of atypical pathogens, which correlates well with the study by Sohan J W et al., [7] from Korea. However, both have selected all the patients with pneumonia whereas we only included patients who were clinically diagnosed to have atypical pneumonia. Even though culture remains the gold standard for the diagnosis of Mycoplasma pneumoniae, our study and Oguz F et al., [8], had nil culture positive cases but serology was positive for IgM and IgG by ELISA. Culture negativity could possibly due to fastidious nature of organisms, loss of viability during transit, previous exposure to antibiotics, influence of normal flora hindering the growth and need for prolonged incubation. Oguz F has further confirmed his findings by PCR and has reported false negativity in culture. Ngeow Y et al., [5] has reported 9.4% of Mycoplasma pneumoniae in his Asian study. A meta-analysis and systematic review by Zahang L et al., [9] has also revealed serology as a better tool for the diagnosis of Mycoplasma pneumoniae. Hence ELISA can be adopted as method for diagnosing where facilities are not available and the results are also available immediately in contrast with culture taking 2-3 weeks for its growth. Global and Asia incidence of Legionella pneumophila is 5 and 6% respectively [4]. In our study the presence of Legionella pneumophila was screened by using BCYE agar for culture and legionella urinary antigen for serology. Both the method had neither culture nor serology positive. Prapphal N et al., [10] in his study on community acquired pneumonia, in adult patients had one positive case out of 47. Ngeow Y et al., [5] in his Asian study had 6.2 % of Legionella pneumophila positive cases. Chlamydia was reported in 5.6% of cases in our study. Other studies like Prapphal N et al., [10], Ngeow Y F et al., [5] and Ruiz M et al., [11] has reported 3.4%, 7% and 4.7% of Chlamydia pneumoniae correlating with our findings.
Incidence of Atypical pneumonia in various studies
| Author | Year of study | Study population | Mycoplasma pneumoniae | Chlamydophila pneumoniae | Legionella pneumophila |
|---|
| Oguz F [8] | 2002 | 1-14 years with Atypical pneumonia | 34.5% | - | - |
| Ngeow [5] | 2004 | > 2years with CAP | 12.2% | 4.7% | 6.6% |
| Prapphal N [10] | 2006 | > 2 years with CAP | 14% | 3.4% | 0.4% |
| Barlett JG [4] | 2008 | Asia and /or Africa | 12% | 5% | 6% |
| This study | 2013-2014 | >18 years of age with atypical pneumonia | 6.5% | 5.6% | 0% |
Limitation
The limitation in our study was the failure in confirmation of the serological positive cases by molecular method
Conclusion
Atypical pathogens should also be considered routinely as a cause of lower respiratory tract infections, especially Chlamydia pneumoniae and Mycoplasma pneumoniae in our country. Serological diagnosis by ELISA can be adopted for determining the infections by atypical pathogens as culture requires special media and prolonged incubation. This may not be feasible for many laboratories. Early diagnosis and treatment will reduce the complications.