Preeclampsia, characterized by hypertension and features of multiple organ disease, complicates 2–8% of pregnancies and can result in maternal and neonatal mortality and morbidity, especially in developing countries [1–3]. Improving the outcome for preeclampsia necessitates accurate and early prediction of the disease to identify women at high risk, enabling prophylaxis with antiplatelet agents such as aspirin, as well as early intervention [4–6]. Even patients with severe disease can be asymptomatic and have normal laboratory findings during early pregnancy [1,4]. As such, recent studies on serum markers such as maternal beta-human chorionic gonadotropin (β-hCG) and pregnancy-associated plasma protein-A (PAPP-A) and ultrasound markers such as uterine artery Doppler velocimetry have gained acceptance as potential predictors of preeclampsia in the first trimester of pregnancy [7,8].
Although multiple mechanisms and factors have long been recognized, including increased oxidative stress; abnormal placentation; cardiovascular maladaptation to pregnancy; malfunction in genetic, immunological, nutritional, hormonal, and angiogenic mechanisms; and inflammation the understanding of the exact pathophysiology of preeclampsia has been elusive [2,5,9].
The term “low-grade inflammation” is used to define the conditions characterized by slightly elevated immune cell count and increased acute phase and proinflammatory protein levels in healthy subjects with no evidence of disease [10,11]. Systemic inflammation can be measured by using a variety of biochemical and haematological markers. Recent findings indicate that measuring blood cell subtype ratios, such as the neutrophiltolymphocyte (NLR) and platelet to lymphocyte (PLR) ratios, might provide prognostic and diagnostic clues to diseases related to chronic low-grade inflammation [3,10,11]. Platelet indices, including mean platelet volume (MPV), platelet distributed width (PDW), and platelet crit (PCT), are other examples of noninvasive biomarkers that can be tested easily and at low cost to assess disease status [12].
In the present study, we aimed to investigate haematological changes in early pregnancy, using simple complete blood count (CBC) and blood concentrations of PAPP-A and free β-hCG to determine whether these measures are of any value in the prediction and early diagnosis of preeclampsia.
Materials and Methods
This retrospective observational case–control study was conducted at the Department of Perinatology, Zekai Tahir Burak Women’s Health Education and Research Hospital, a tertiary center in Ankara, Turkey. The Institutional Review Board of the hospital approved the study and the universal principles of the Declaration of Helsinki were applied.
The study group consisted of hospitalized and eventually delivered nulliparous patients with a diagnosis of preeclampsia between October 2012 and November 2014. Healthy pregnant women without any pregnancy complications and who delivered at ≥37 weeks were recruited within the same time interval as the control group.
Consecutive patients between the ages of 18 and 40 years with singleton nulliparous pregnancies who conceived spontaneously were included in the study.
All of the pregnant were examined for infection, routine urine cultures were obtained and body temperature was measured. Patient with any signs and symptoms of active infection (pain, fever, or vaginal discharge), were excluded from the study. In addition, pregnant with any known medical condition or chronic systemic disease (endocrinological, urogenital, cardiovascular, gastrointestinal, immunological, or oncological) or multiple gestations, or complication of pregnancy, such as abortion, intrauterine fetal demise, antenatal bleeding, gestational diabetes mellitus, or spontaneous preterm delivery was not included. Patients with pre-pregnancy obesity (body mass index {BMI} ≥30kg/m2); suspected or known chromosomally or morphologically anomalous fetus were also not included in the study.
The diagnosis of preeclampsia was based on a systolic blood pressure of ≥140 mmHg or diastolic blood pressure ≥90 mmHg, measured twice in four-hour intervals while resting, after the 20th gestational week, as well as 300 mg/dL proteinuria detected in a 24-hour urine sample, or in the absence of proteinuria, hypertension together with evidence of systemic disease, including thrombocytopenia, increased levels of liver transaminases, renal failure, pulmonary oedema, and visual or cerebral disturbances. The diagnosis of severe preeclampsia was based on the presence of any of the following criteria: systolic blood pressure ≥160 mm Hg or diastolic blood pressure ≥110 mmHg on two separate measurements, performed at six-hour intervals at the least, elevated serum creatinine level (>1.1 mg/dL), headache, visual impairment, epigastric pain or pain in the right upper quadrant, elevated hepatic transaminases (≥ 40 IU/ml), thrombocytopenia (PLT<100,000/μL), or pulmonary oedema [13]. The patients were classified as having severe preeclampsia (group 1) or mild (group 2) preeclampsia, as well as the control subjects (group 3).
Gestational age was determined based on the first day of the last menstrual period (LMP) and first trimester ultrasonographic measurement of the crown–rump length (CRL). If ultrasound dating differed from LMP dating by more than seven days, the estimated due date was changed to correspond with the ultrasound dating. If the patient was unsure of her LMP, dating was based on ultrasound estimates by using the earliest CRL measurement during the first trimester [14].
Blood samples for routine CBC and first trimester screen (FTS), which combines PAPP-A and free β-hCG blood concentrations, the thickness of the nuchal translucency by ultrasound, and maternal age, were all taken during the same visit at 11 + 0 to 13 + 6 weeks of gestation.
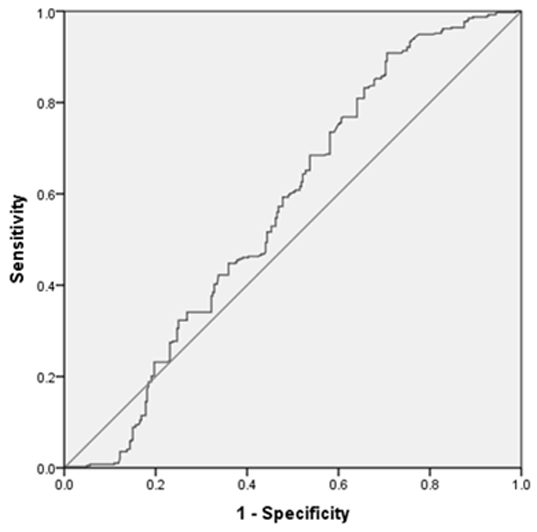
All CBC analyses were conducted in the central haematology laboratory of the hospital within two hours of collecting the blood samples, using a Gen-S automated analyser (Beckman Coulter, High Wycombe, UK). NLR and PLR values were calculated by dividing the absolute neutrophil and platelet counts, respectively, by the absolute lymphocyte counts. The predictive values of first trimester NLR and PLR for preeclampsia and PDW were estimated by Receiver Operating Characteristic (ROC) analysis calculating area under the curve (AUC).
The measured free β-hCG and PAPP-A values were converted to a gestation-specific multiple of the medians (MoM), using Prisca 4.0 software (Typolog, Tornesch, Germany). Because PAPP-A levels are reduced in smokers, separate medians were used for each group. PAPP-A and free β-hCGMoM values were corrected for maternal weight using reciprocal-linear regression [15].
Demographic data, including maternal age, medical clinical status, gestational week, smoking habits, BMI, perinatal outcome, and the laboratory data of the routine CBC and FTS were obtained from the patient records.
Statistical Analysis
The data were analysed using the Statistical Package for the Social Sciences version 15.0 (SPSS Inc., Chicago, IL). Descriptive statistics were expressed as mean and standard deviation for numerical variables. The Kolmogorov–Smirnov test was used to analyse the normal distribution of the variables. Subgroup comparisons were performed using the Mann–Whitney U-test with Bonferroni correction. The best cut-off points of NLR to discriminate patients and control groups each other was evaluated by ROC analysis calculating AUC as giving the maximum sum of sensitivity and specificity for the significant test. Sensitivity, specificity, positive and negative predictive values were also calculated at the best cut-off point for NLR. Statistical significance was set at p<0.05.
Results
During the study period, a total of 28,633 patients delivered infants, 1774 of whom were diagnosed with preeclampsia, for a prevalence rate of 6.1%. Seven hundred sixty five patients with preeclampsia met the inclusion criteria, and 400 healthy patients without any pregnancy complications were recruited as controls. One hundred fifty one patients in the study group and 80 patients in the control group were further excluded due to missing clinical or laboratory files. Twenty-seven of pregnant would be re-dated by using the earliest CRL measurement during the first trimester.
In the end, the data of 614 patients with preeclampsia (288 with mild disease and 326 with severe disease) and 320 healthy pregnant women were evaluated for final analysis.
Maternal age, gravidity, smoking status, CRL at screening, and BMI were comparable among all three groups. The demographic and obstetrical data of the severe preeclampsia (group 1), mild preeclampsia (group 2), and control (group 3) groups are shown in [Table/Fig-1].
Comparison of demographic and clinical characteristics of severe preeclampsia (group 1), mild preeclampsia (Group 2) and the control group (Group 3)
| Group 1 (n=326) | Group 2 (n=288) | Group 3 (n=320) | p-value |
|---|
| p1vs2 | p1vs3 | p2vs3 |
|---|
| Maternal age (years) | 29.3± 14.3 | 27.9± 4.9 | 27.0± 5.0 | 0.124 | 0.211 | 0.99 |
| Gravidity (range) | 2 (0–3) | 2 (1–3) | 1 (0–2) | 0.097 | 0.081 | 0.13 |
| Parity | 0 | 0 | 0 | - | - | - |
| Smoking, n (%) | 16 (5%) | 10 (3.5%) | 12 (3.7%) | 0.44 | 0.69 | 0.89 |
| CRL at screening (mm) (range) | 65.75 (54.5-79) | 61.75 (55-78) | 64.9 (60-76.5) | 0.58 | 0.67 | 0.83 |
| PE occurring week | 32.4 ± 3.5 | 36.5 ± 2.9 | - | <0.001* | - | - |
| Pre-pregnancy BMI, kg/m2 | 23.7± 3.6 | 22.9 ± 3.1 | 22.7 ± 3.6 | 0.175 | 0.068 | 0.09 |
| Gestational age at delivery (weeks) | 33.0± 3.5 | 37.5 ± 2.1 | 40.6 ± 1.6 | <0.001* | <0.001* | <0.001* |
| Neonatal Birthweight (grams) | 2045 ± 597 | 2923 ± 519 | 3417 ± 314 | <0.001* | <0.001* | <0.001* |
Data expressed as number (%), mean ± SD, median (minimum - maximum). * indicates statistical significance
While the mean white blood cell, neutrophil, platelet, MPV, PCT, and free β-hCG values were comparable among the three groups, the mean lymphocyte count was significantly different in each group. The PAPP-A levels were significantly higher in the group 3 compared with the group 1 and group 2 (p< 0.01 and p< 0.01, respectively). The haematological test results of the group 1, group 2, and group 3 are provided in [Table/Fig-2]. The NLR values were significantly higher in the group 1compared with the group 3 (p<0.01). Furthermore, PLR values were found to be significantly higher in the patients with severe preeclampsia compared to the patients with mild preeclampsia (p=0.05).
Although the PDW values were significantly higher in both preeclampsia groups compared with the healthy control group (p<0.01), the difference was not significant between the mild and severe preeclampsia groups. The positive predictive value of NLR for preeclampsia was determined by ROC analysis. At a cutoff level of 4.01, NLR accurately predicted preeclampsia {AUC=0.568 (95% confidence interval 0.524–0.612), p=0.002} with sensitivity and specificity rates of 79.1% and 38.7% and positive and negative predictive values of 73.6% and 72.3%, respectively [Table/Fig-3].
Comparison of the hematological results of severe preeclampsia (group 1), mild preeclampsia (Group 2) and the control group (Group 3)
| Group 1(n=326) | Group 2(n=288) | Group 3(n=320) | p values |
|---|
| p1vs2 | p1vs3 | p2vs3 |
|---|
| PAPP-A (MoM) | 0.77± 0.12 | 0.79± .33 | 1.18± 0.85 | 0.571 | <0.001* | <0.001* |
| Free B-HCG (MoM) | 1.05± 0.49 | 0.99± 0.52 | 1.06± 0.33 | 0.35 | 0.21 | 0.8 |
| WBC count, (x103/mm3) | 9.3± 1400 | 8.8± 1400 | 8.4± 1400 | 0.53 | 0.41 | 0.6 |
| Neutrophil count, (x103/mm3) | 6.8± 2.0 | 6.9± 2.1 | 6.5± 1.6 | 0.085 | 0.561 | 0.218 |
| Lymphocyte count, (x103/mm3) | 1.8± 0.52 | 2.0± 0.56 | 2.3± 0.81 | 0.005* | <0.001* | <0.001* |
| NLR | 4.54± 2.98 | 3.97± 1.34 | 3.23± 1.33 | 0.86 | <0.001* | 0.005* |
| PLT count, (x103/mm3) | 238± 47 | 236± 54 | 239± 63 | 0.085 | 0.650 | 0.14 |
| PLR | 139± 91 | 118± 41 | 121± 52 | 0.009 | 0.007 | 0.876 |
| MPV | 10.0± 1.12 | 10.2± 0.97 | 10.4± 1.2 | 0.146 | 0.326 | 0.259 |
| PCT | 0.248± 0.05 | 0.252± 0.06 | 0.246± 0.05 | 0.777 | 0.007 | 0.112 |
| PDW | 13.4± 2.53 | 12.6± 2.21 | 11.7± 1.93 | 0.09 | <0.001* | <0.001* |
Data expressed as number (%), mean ± SD, median (minimum - maximum). * indicates statistical significance. MPV, Mean Platelet Volume; NLR, Neutrophil/lymphocyte ratio; PDW; platelet distribution width; PLT, Platelet; PLR, Platelet/lymphocyte ratio; MPV; PCT, Plateletcrit. WBC, white blood cell.
BMI, Body mass index; CRL, Crown–Rump Length; PE, Preeclampsia
Area under the receiver operating characteristic curve for NLR measurements for predicting preeclampsia. The area under the curve was 0.568 (95% confidence interval 0.524–0.612)
Discussion
In the present study, NLR was found to be significantly higher in patients with preeclampsia, albeit with low specificity in the ROC analysis, and it was also predictive in discriminating the severe cases from the mild ones. We also confirmed that levels of PAPP-A were lower in patients who developed preeclampsia. To the best of our knowledge, this is the first study to explore the possible relationships among NLR, PLR, PAPP-A and other routine haematologic parameters and preeclampsia in the first trimester.
Despite significant advances in the understanding of the complex pathogenesis of preeclampsia, there is not yet a method that predicts the disease accurately in the first trimester. An ideal predictive method should be fast, simple, inexpensive, valid, noninvasive, reproducible, and reliable [16]. Thus far, no single biomarker has met these criteria [17].
Several recent studies have explored the diagnostic and prognostic value of NLR and PLR in pregnant women with preeclampsia. Although Kurtoglu et al., demonstrated retrospectively that NLR values were significantly higher in preeclamptic patients; the test did not predict the severity of the disease [18]. Likewise, Yavuzcan et al., reported that the NLR values of patients with severe preeclampsia were significantly higher than healthy pregnant women; however, MPV and PLR values were comparable among the groups [19]. Oylumlu et al., also found that NLR, as an independent marker, was predictive of preeclampsia [20].
Abnormalities of haemostasis and coagulation (probably resulting from endothelial damage), including enhanced platelet activity, are implicated in the pathogenesis of preeclampsia [21]. The MPV, PCT, and PDW indices are well-known parameters that reflect platelet activation and alteration in the haemostatic system, including endothelial cell damage [21,22]. In our study, while PLT, MPV, and PCT values were comparable among the groups between 11 and 14 weeks of gestation, PDW values were higher in the pregnant patients who later developed preeclampsia. The combination of PAPP-A and β-hCG measurements, along with several ultrasonography markers, has been used frequently for first trimester screening for chromosomal abnormalities. Altered maternal serum marker levels have also been found to be associated with obstetric complications [23]. Low maternal serum PAPP-A in the first trimester is associated with increased risk of subsequent development of preeclampsia in chromosomally normal pregnancies, but its predictive value as a single screening test alone is poor [24]. Goetzinger et al., investigated the predictive value of a model consisting of first trimester PAPP-A, free-β-HCG, and maternal characteristics, and they found that low PAPP-A levels were related to the development of preeclampsia in the later weeks of pregnancy; however, predictive accuracy of their model was quite low [25]. In the FASTER trial, it was demonstrated that patients with low PAPP-A levels were significantly more likely to experience adverse pregnancy outcomes, including preeclampsia; however, the sensitivity and positive predictive values were relatively low [24].
The associations among inflammation, obesity [26] and preeclampsia are well known [5,9]. In the present study, the possible confounding effects were eliminated, because BMI was similar in the three groups and patients with infectious diseases were excluded. We demonstrated that levels of PAPP-A were lower and NLR values were higher in, patients who developed preeclampsia. Because measuring CBC parameters, particularly NLR and PDW, are fast and easily applicable, they can be used routinely in almost every laboratory setup to predict preeclampsia in early pregnancy.
Limitations
Major limitations of our study were its retrospective design and the inability to calculate population-based rates. Despite our best efforts to adjust for clinically relevant characteristics, the possibility of residual confounding remains. Despite these limitations, our study is the first of its kind to investigate the relationship among preeclampsia, first trimester combined test and simple complete blood count parameters. We believe that large-scale and prospective studies are needed to reproduce our data, and thus, to clarify the upper and lower normal limits, as well as the modulating factors and predictive value of these haematologic parameters.
Conclusion
This study is the first report focusing on the relationship among the first trimester combined test parameters, simple complete blood count parameters and preeclampsia in the literature. On the contrary many other inflammatory markers and bioassays, NLR is a simple, cheap and readily available marker that may be useful to predict preeclampsia in early pregnancy.
Data expressed as number (%), mean ± SD, median (minimum - maximum). * indicates statistical significance
Data expressed as number (%), mean ± SD, median (minimum - maximum). * indicates statistical significance. MPV, Mean Platelet Volume; NLR, Neutrophil/lymphocyte ratio; PDW; platelet distribution width; PLT, Platelet; PLR, Platelet/lymphocyte ratio; MPV; PCT, Plateletcrit. WBC, white blood cell.
BMI, Body mass index; CRL, Crown–Rump Length; PE, Preeclampsia