Pregnancy Associated Breast Cancer: Awareness is the Key to Diagnosis -A Case Report
Namrata Nargotra1, Dipti Kalita2
1 Senior Specialist and Head, Department of Pathology, Hindu Rao Hospital and, North DMC Medical College, Delhi, India.
2 Specialist, Department of Pathology, Hindu Rao Hospital and North DMC Medical College, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Dipti Kalita, House no. 15, 2nd Floor, Uday Park, New Delhi-49, India.
E-mail: diptikalita@yahoo.co.in
Pregnancy-associated breast cancer (PABC) is defined as breast cancer that occurs during pregnancy or within one year of delivery. PABCs are typically found at advanced stage and are reported to have higher recurrence and mortality rates as compared to non PABC. Although it is said to be rare its incidence is increasing. Very little data is available on PABC among Indian women. Delay in diagnosis is one of the major causes of aggressive presentation of PABC. This is due to the fact that most of the lesions presenting during this period are benign and lactational changes hamper the detection of mass clinically as well as by various investigative methods. Paget’s disease of breast, usually reported in elderly woman, when occurs in lactating breast may mimic benign eczematous lesion. Increased awareness among patients as well as clinicians is required to detect this highly aggressive form of breast cancer at an early and treatable stage. Treatment is by multidisciplinary approach and depends upon the gestational stage. Here we report a case of PABC in a lactating woman presenting with Paget’s disease because such case may be under diagnosed as breast feeding related lesion leading to delayed diagnosis.
Lactational change, Paget’s disease
Case Report
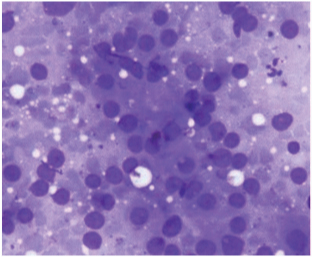
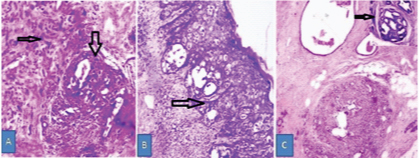
A 32-year-old woman presented with ulceration and retraction of nipple of the left breast and a slowly growing breast lump on the same side since delivery of her baby 1 year back. There was history of blood mixed white discharge from the left nipple on few occasions. She did not have family history of breast cancer. These symptoms were initially considered as lactation related and hence were ignored. On examination, a lump of 1.5cm x1.5cm size was felt in the left lower quadrant, firm in consistency, not fixed to underlying tissue or overlying skin. Mammography revealed asymmetrical increased density in the left breast with skin and subcutaneous thickening. Fine needle aspiration cytology (FNAC) from the lump revealed highly cellular smear with loosely cohesive groups of acinar cells showing moderate anisokaryosis, nucleomegaly with prominent nucleoli in a lipoproteinaceous background [Table/Fig-1]. On Magnetic resonance imaging (MRI) a nodular lesion was seen, suspicious of malignancy without obvious infiltration or destruction. Core needle biopsy from the breast lump showed features of infiltrating carcinoma. The patient underwent modified radical mastectomy and gross examination of the specimen measuring 20cmx13cmx5cm revealed ulceration in the nipple [Table/Fig-2a] and a tumour mass measuring 4cmx4cm extending from nipple [Table/Fig-2b]. Microscopic examination revealed infiltrating duct carcinoma, grade 3, with high grade ductal carcinoma in situ (DCIS) and Paget’s disease of nipple [Table/Fig-3a] with negative resected margins. Intraepidermal malignant cells were seen throughout the nipple involving lactiferous ducts and focally infiltrating into underlying tissue [Table/Fig-3b]. The adjacent breast tissue showed wide spread fibrocystic change, lobular hyperplasia and lactational change [Table/Fig-3c]. Eleven axillary lymph nodes revealed metastatic deposits. Hormonal status (ER, PR) was negative. She received six cycles of standard dose of adjuvant chemotherapy and radiotherapy was planned. She, however, developed liver metastasis and died of advanced disease within one year of diagnosis.
FNAC smear showing cells in loose cohesive groups and microacinar pattern in a vacuolated background. Moderate anisokaryosis, uniform nuclear chromatin and in few cells prominent nucleoli are seen. MGG stain, x400
Mastectomy specimen showing: a) nipple with ulceration; and b) gross appearance of the tumour

Microscopic pictures showing: a) DCIS (thick arrow) and infiltrating duct carcinoma(thin arrow) H&E stain, x100; b) Intraepidermal malignant cells in the nipple- Paget’s disease (arrow) H&E stain, x100; c) Lobular hyperplasia, cystic change, fibrosis and lactational change (inset, arrow), H&E stain, x40
Discussion
Pregnancy-associated breast cancer (PABC) is defined as breast cancer that occurs during pregnancy or within one year of delivery. PABCs are typically found at advanced stage, have a higher incidence of lymph node metastases and are poorly differentiated [1]. Data on outcome of PABC are conflicting, however it is said to have unfavourable prognosis as compared to non PABC [2]. Delay in diagnosis is the major cause of advanced presentation of PABC. Basaran et al., observed that there was a diagnostic delay between occurrence of the presenting symptoms and the initiation of breast mass workup in 40% of PABC cases included in their study [3]. In another study it was found that there was diagnostic delay in 60% PABC cases and in 40% cases it was due to physician’s reassurance [4]. A more aggressive growth pattern of the tumour, caused by the biological effects of pregnancy, is also associated with a poor prognosis in PABC. Compared with the non-PABCs, PABCs have twice more frequent HER2 over-expression and hormone receptor (ER, PR) negative status which adds to their unfavourable prognosis of PABC [5].
Breast cancer is one of the most common cancers diagnosed during pregnancy. Although it is said to be a rare event, its incidence is on rising with increasing age of first pregnancy. It accounts for 7% to 14.5% of all breast cancer cases as reported in studies from western countries [5,6]. The reported age of occurrence ranged from late 2nd decade to 4th decade [6,7].
There is little available data on PABC in Indian women. In an institutional study incidence has been reported to be 0.7% which is much less than that of western countries [8]. Majority of cases presented to clinician after delivery. Median duration of disease for all the cases was 11.5 months with 50% survival rate at 3 years. Low incidence may reflect under diagnosis and under reporting of cases due to lack of awareness. Large systematic multi-institutional study is required to know actual incidence and characteristics of a PABC in Indian women.
Majority of breast masses occurring during pregnancy and lactational period are benign, among which common are fibroadenoma, lactational adenoma, mastitis, abscess formation, galactocele and breast tissue with lactational change [9]. A sore or inflamed or eczematous nipple is also a common finding in lactational period, although the incidence is unknown. One must suspect Paget’s disease if “eczema” is unilateral or persists for more than 3weeks [10].
The physiologic changes associated with pregnancy and lactation makes detection and evaluation of breast masses difficult, both by clinical examination and radiologically. During the lactational period, breast parenchymal density is further increased leading to more difficulty in diagnosing a tumour in mammography [9]. In such cases, ultrasonography is a more suitable diagnostic procedure than mammography. In a study by Bo Young Ahn, et al., mammographic sensitivity was 86.7%, while sonographic sensitivity was 100% [11]. The sonographic appearance of PABC is somewhat different from that in non pregnant breast cancer, because of the associated physiological changes. Sometimes complex features such as cystic change, high vascularity, spontaneous infarction etc may arouse suspicion of malignancy even in a benign lesion like fibroadenoma on radiological assessment [10]. Breast MRI has emerged as the most sensitive modality for evaluation of the breast, especially in detecting mammography negative carcinoma in dense breast; however, it is limited by low specificity [12].
Any breast lump clinically or radiologically showing atypical or suspicious features must undergo cytological and histological evaluation. FNAC can be easily and safely done in both pregnant and lactating women. Both false positivity and false negativity have been issues in cytological diagnosis of lactating breast. Few publications are available in literature addressing the issue of over diagnosing malignancy in cytology [13,14]. False positivity is because of atypical features like high cellularity, nucleomegaly, and anisonucleosis etc. which are commonly seen in lactational breast and lactational adenoma. Core needle biopsy should be done which will determine the nature of the lesion.
A few studies are available regarding the importance of histopathology of PABC, and it has been reported as similar to that in non pregnant patients. Shousha S, reported few distinctive histomorphological features like cancerization of lobule and foci of mucinous change in PABC [15].
Paget’s disease most often occurs in postmenopausal women, accounts for 1% to 4% of all cases of female breast carcinoma and presents as a chronic eczematous change of the nipple often with an underlying lump. Eczema of the nipple and areola frequently develops in the breastfeeding women and is associated with sore, burning, and painful sensations. There is always a risk to ignore the nipple changes in a lactating woman as benign on casual examination by inexperienced observer. Nipple scrape cytology or imprint cytology can be easily done whenever there is slightest suspicion, however, the material may not be sufficient for a specific diagnosis. Such patient should be extensively evaluated to exclude malignancy.
Treatment of PABC is multidisciplinary and depends on gestational age. Surgery can be performed at any time during pregnancy and post partum period. Radiotherapy and endocrine therapy are contraindicated during pregnancy but chemotherapy can be administered from second trimester onwards. Data on outcome of PABC is controversial, but recent studies suggest that PABC patients had a higher risk of both death and recurrence as compared to age and stage matched control [2].
Conclusion
This case presented a classical picture of PABC with delayed diagnosis in advanced stage where clinical picture mimicked that of benign breast lesion with nipple changes. Cytological features were not confirmatory and mammography failed to detect the underlying lesion. In order to detect PABC in early stage index of suspicion should be high and such case should be thoroughly investigated keeping in mind the pit falls of various diagnostic modalities and aggressiveness of the disease. There is a need to increase awareness about PABC among primary care physicians and pregnant and lactating women to ensure its early detection and prompt treatment.
[1]. Middleton LP, Amin M, Gwyn K, Theriault R, Sahin A, Breast carcinoma in pregnant women: assessment of clinicopathologic and immunohistochemical featuresCancer 2003 98:1055-60. [Google Scholar]
[2]. Ali SA, Gupta S, Sehgal R, Vogel V, Survival outcomes in pregnancy associated breast cancer: A retrospective case control studyBreast J 2012 18:139-44. [Google Scholar]
[3]. Basaran D, Turgal M, Beksac K, Ozyuncu O, Aran O, Beksac MS, Pregnancy-associated breast cancer: clinicopathological characteristics of 20 cases with a focus on identifiable causes of diagnostic delayBreast Care (Basel) 2014 9:355-59. [Google Scholar]
[4]. Al-Amri AM, Clinical presentation and causes of the delayed diagnosis of breast cancer in patients with pregnancy associated breast cancerJ Family Community Med 2015 22:96-100. [Google Scholar]
[5]. Genin AS, Lesieur B, Gligorov J, Antoine M, Selleret L, Rouzier R, Pregnancy-associated breast cancers: do they differ from other breast cancers in young women?Breast 2012 21:550-55. [Google Scholar]
[6]. Langer A, Mohallem M, Stevens D, Rouzier R, Lerebours F, Chérel P, A single-institution study of 117 pregnancy-associated breast cancers (PABC): Presentation, imaging, clinicopathological data and outcomeDiagn Interv Imaging 2014 95:435-41. [Google Scholar]
[7]. Bodner-Adler B, Bodner K, Zeisler H, Breast cancer diagnosed during pregnancyAnticancer Res 2007 27:1705-07. [Google Scholar]
[8]. Gogia A, Deo S, Shukla NK, Mohanti BK, Raina V, Pregnancy associated breast cancer: An institutional experienceIndian J Cancer 2014 51:167-69. [Google Scholar]
[9]. Yu JH, Kim MJ, Cho H, Liu HJ, Han SJ, Ahn TG, Breast diseases during pregnancy and lactationObstet Gynecol Sci 2013 56:143-59. [Google Scholar]
[10]. Barankin B, Gross MS, Nipple and areolar eczema in the breastfeeding womanJ Cutan Med Surg 2004 8:126-30. [Google Scholar]
[11]. Ahn BY, Kim HH, Moon WK, Pisano ED, Kim HS, Cha ES, Pregnancy- and lactation-associated breast cancer: mammographic and sonographic findingsJ Ultrasound Med 2003 22:491-97. [Google Scholar]
[12]. Saslow D, Boetes C, Burke W, Harms S, Leach MO, Lehman CD, American Cancer Society Breast Cancer Advisory Group. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammographyCA Cancer J Clin 2007 57:75-89. [Google Scholar]
[13]. O’Neil S, Castelli M, Gattuso P, Kluskens L, Madsen K, Aranha G, Fine-needle aspiration of 697 palpable breast lesions with histopathologic correlationSurgery 1997 122:824-28. [Google Scholar]
[14]. Stanley MW, Sidawy MK, Sanchez MA, Stahl RE, Goldfischer M, Current issues in breast cytopathologyAm J Clin Pathol 2000 113:S49-75. [Google Scholar]
[15]. Shousha S, Breast carcinoma presenting during or shortly after pregnancy and lactationArch Pathol Lab Med 2000 124:1053-56. [Google Scholar]