Cystic Lymhangioma of the Lesser Sac in Adult Presenting with Features of Gastric Outlet Obstruction - A Case Report
Sathasivam Suresh Kumar1, Sri Aurobindo Prasad Das2, Vikram Kate3
1 Assistant Professor, Department of Surgery, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry, India.
2 Senior Resident, Department of Surgery, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry, India.
3 Professor, Department of Surgery, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vikram Kate, Professor, Department of Surgery, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry-605006, India.
E-mail: drvikramkate@gmail.com
Cystic lymphangioma is a paediatric benign tumour, occurs commonly in head and neck region. Adult intraabdominal lymphangiomas are uncommon and only few cases of lesser sac cystic lymphangioma are reported in the literature. We present a case of lesser sac cystic lymphangioma in a 26-year-old lady who presented with features of gastric outlet obstruction. Clinical examination revealed a 10x10 cm firm, non tender, mobile intraabdominal lump in the epigastrium. An upper gastrointestinal endoscopy showed possible external compression at the body of the stomach. Ultrasound demonstrated a multicystic lesion, with internal echoes in one locule. CECT showed a large multiloculated cystic lesion with hyper-dense content in the lesser sac extending up to the left lobe of the liver and indenting the stomach, lesser sac, and upper border of pancreas. On surgical exploration, a 10X8 cm multi cystic lesion with clear fluid was found in the lesser sac very close to the lesser curvature of stomach. Histopathological examination of the excised lesion showed features of cystic lymphangioma. Though very rare, intraabdominal cystic lymphangiomas should be considered in all atypical cases of gastric outlet obstruction. A reasonable knowledge about these benign lesions will aid in establishing the diagnosis and surgical management.
Intraabdominal cystic tumour, Lymphatic cyst, Omental bursa
Case Report
A 26-year-old lady presented to surgical outpatient department with complaints of early satiety, vomiting few hours after food intake and vague fullness of upper abdomen. She also had features of dyspepsia for the past one year. She had developed pain and had a feeling of a mobile lump in the upper abdomen for the past one month. There was no pancreatitis episode before. General physical examination was unremarkable. Clinical examination of the abdomen revealed 10x10 cm lump in the epigastrium which was firm in consistency. The lump was non tender, freely mobile and intra-abdominal. The haemogram and biochemical profiles were within normal limits. An upper gastrointestinal endoscopy was done which showed normal mucosa of stomach with possible external compression at the body of the stomach. Ultrasound of abdomen was suggestive of a multicystic lesion measuring 10X8 cm, with internal echoes in one locule, present superior to pancreas adjacent to the left lobe of the liver. Rest of abdomen was unremarkable.
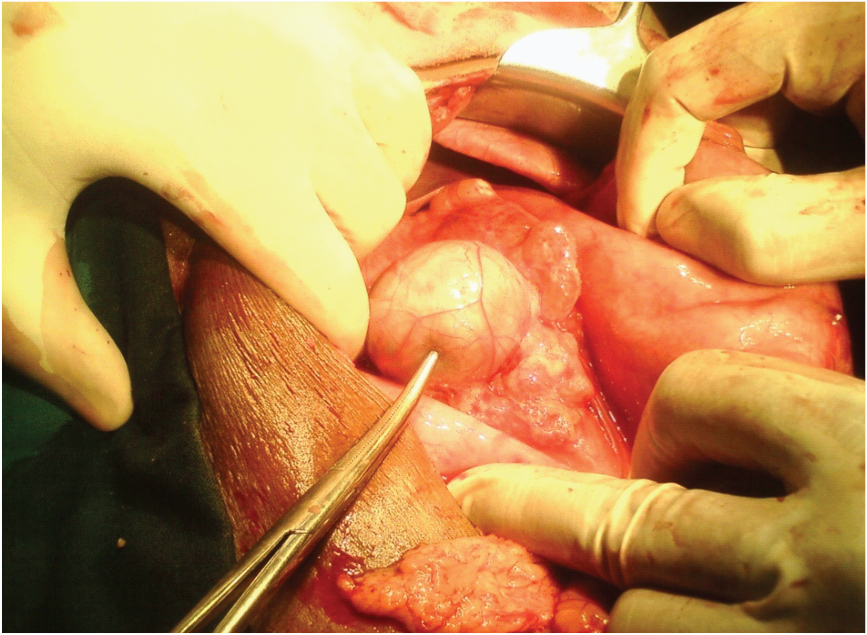
Contrast enhanced computed tomography of the abdomen showed a large multiloculated cystic lesion measuring 10.2X8 cm with hyper dense content in some loculi in the lesser sac extending up to the left lobe of the liver and indenting the stomach, lesser sac, and upper border of pancreas with a few branches of left gastric vessels coursing through it [Table/Fig-1]. Correlating the clinical, USG and CECT abdomen findings a diagnosis of possible lymphangioma or cystic mesothelioma was made and the patient was planned for exploratory laparotomy as the symptoms were persisting. On surgical exploration, a 10X8 cm multi cystic lesion with clear fluid was found in the lesser sac very close to the lesser curvature of stomach [Table/Fig-2]. The descending branches of left gastric which were found coursing through the cyst were ligated and the cyst was excised in Toto [Table/Fig-3]. A drain was placed in lesser sac and abdomen was closed in layers.
Contrast enhanced computed tomography showing large multiloculated cystic lesion with hyper dense content in the lesser sac extending up to the left lobe of the liver

Intraoperative image showing multi cystic lesion in the lesser sac very close to the lesser curvature of stomach
Excised specimen of cystic lymphangioma

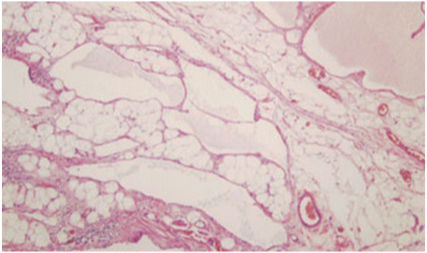
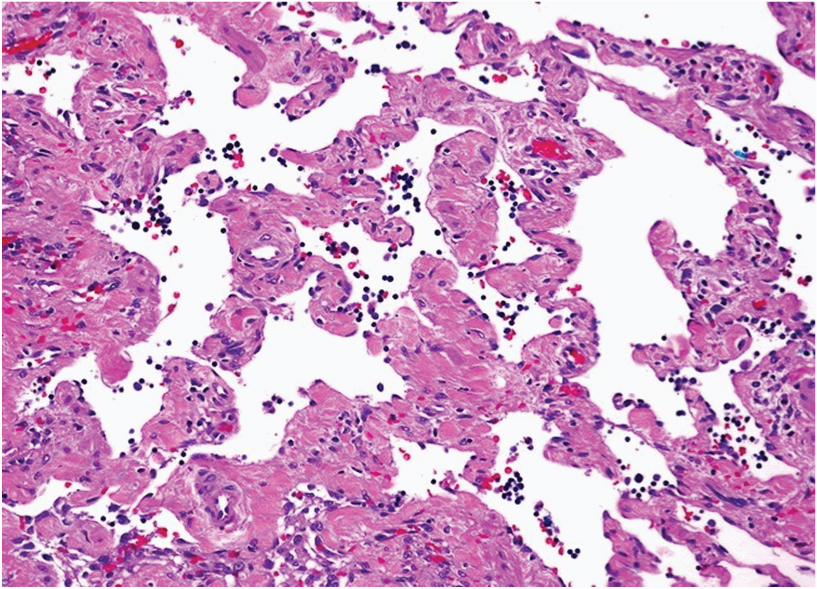
Postoperative course was uneventful. The drain was removed on the 3rd postoperative day and the patient was discharged on seventh postoperative day. Histopathological examination of the excised lesion showed features of cystic lymphangioma showing dilated lymphatic vessels with fibro-fatty tissue ingrained in the endothelial lining [Table/Fig-4]. High power view demonstrated anatomising lymphatic spaces along with a few red blood cells and numerous lymphocytes in the lymphatic channels [Table/Fig-5].
Histopathological examination showing dilated lymphatic vessels with fibro-fatty tissue ingrained in the endothelial lining
High power histopathological view demonstrating anastomosing lymphatic spaces along with a few red blood cells and numerous lymphocytes in the lymphatic channels
Patient was followed up at one month, six months, one year and two year after surgery. On each visit, clinical examination and USG was done which showed no evidence of recurrence. The lady is presently on regular follow up for past 2 years with no evidence recurrence till date.
Discussion
Ninety percent of the lymphagiomas manifest itself within the first two years of life and symptomatic presentation in adults is very rare [1]. Though intraabdominal lymphangioma accounts for <1% it is of particular importance because of the atypical presentation, difficulty in differentiating from other causes and relatively little knowledge about this uncommon entity among the treating surgeons. Reported sites of intraabdominal lymphangioma include small bowel mesentery, omentum, broad ligament, hepaticoduodenal ligament, and retroperitoneum [2–4]. Very few cases of lesser sac lymphangiomas have been reported with varied symptomatology [3,4]. We had a case of cystic lymphangioma in the lesser sac which is very rare. Primary cystic lymphangioma are believed to be originating from malformed or malpositioned lymphatic channels. Secondary lymphangioma may also occur following surgical procedure, abdominal trauma or post-radiotherapy lymphatic obstruction [1–4]. The indexed patient did not have any of the secondary inciting factors. The cause probably was congenital which had manifested late in life.
Commonly known to present in childhood, lymphagiomas sometimes remain asymptomatic until late adulthood, and are discovered during evaluation of vague and chronic nonspecific symptoms like anorexia, nausea, vomiting, fatigue, and weight loss, which are secondary to mass effect [4]. This was seen in our patient who had early satiety and vomiting after food intake probably due to mass effect and had a vague feeling of mass in the abdomen. Other ways of presentation such as acute abdomen, mimicking acute appendicitis has also been reported [3].
Contrast CT done in our patient revealed multicystic lesion measuring 10.2X8 cm, present superior to pancreas, in the lesser sac adjacent to the left lobe of the liver. Characteristic feature of cystic lymphangioma in ultrasound include multiloculated cysts of varied sizes separated by thin septa. Majority of the cysts shows anechoic clear fluid and rarely echogenic debris inside the cyst. Contrast enhanced CT typically show cyst wall enhancement with or without calcification [4,5]. Image features at times difficult to differentiate from enteric duplication cyst, non- pancreatic pseudocyst or pseudomyxoma peritonei particularly in the presence of altered fluid attenuation in CT due to infection in the cyst [5].
Cystic mesothelioma that typically occurs in reproductive age group female is often impossible to differentiate from cystic lymphangioma preoperatively due to the non specific symptoms and similar imaging characteristics of both entities [6]. Other differential diagnosis includes cystic lesions of enteric or urogenital origin. Pancreatic pseudocysts from trauma, dermoid cysts or teratomas and cystic degeneration of solid tumours are also to be considered before making this rare diagnosis [5,6].
Management of intra-abdominal cystic tumours depends on the size of the cyst, clinical symptoms and the degree of suspicion for malignancy. Imaging generally provides valuable information for the treatment planning. Complete removal of the tumour offers an excellent prognosis and laparoscopic removal of lymphangioma also shown feasible in few reports [7]. We therefore decided to perform a laparotomy and complete excision of the cyst was done. Recurrence rate is reported to be 10% mainly with patients in whom primary resection was incomplete [8]. If the feeding lymphatics are not completely ligated, chylous ascites may also occur.
Conclusion
Though intra-abdominal cystic lymphangiomas are very rare, it should be considered in cases of gastric or biliary obstruction where the cause could not be recognized clearly. Complete surgical excision offers the best chance for cure and should be attempted in all the cases to avoid recurrence.
Consent
Written informed consent was obtained from the patient for publication of this Case report and any accompanying images.
[1]. Hanagiri T, Baba M, Shimabukuro T, Hashimoto M, Takemoto H, Inoue A, Lymphangioma in the small intestine: Report of a case and review of the Japanese literatureSurgery Today 1992 22:363-67. [Google Scholar]
[2]. Roisman I, Manny J, Fields S, Shiloni E, Intra-abdominal lymphangiomaBr J Surg 1989 76:485-89. [Google Scholar]
[3]. Tan BH, Lim T, Cystic lymphangioma of the lesser sac presenting as acute appendicitis: A case reportCases J 2008 1(1):147 [Google Scholar]
[4]. El Barni R, Lahkim M, Fihri JF, Mejdane A, Bouchama R, Achour A, Cystic lymphangioma of the lesser sacPan Afr Med J 2014 17:48 [Google Scholar]
[5]. Arraiza M, Metser U, Vajpeyi R, Khalili K, Hanbidge A, Kennedy E, Primary cystic peritoneal masses and mimickers: spectrum of diseases with pathologic correlationAbdom Imaging 2015 40(4):875-906. [Google Scholar]
[6]. Eire PF, Bouzas MXL, Rey JAO, Villaraviz MH, Arias MP, Benign cystic mesothelioma in a boy: An uncommon case mimicking a lymphangiomaJ Paediatr Child Health 2015 51(8):841-42. [Google Scholar]
[7]. Makni A, Chebbi F, Fetirich F, Ksantini R, Bedioui H, Jouini M, Surgical management of intra-abdominal cystic lymphangioma. Report of 20 casesWorld J Surg 2012 36(5):1037-43. [Google Scholar]
[8]. Steyaert H, Guitard J, Moscovici J, Juricic M, Vaysse P, Juskiewenski S, Abdominal cystic lymphangioma in children: benign lesions that can have a proliferative courseJ Pediatr Surg 1996 31:677-80. [Google Scholar]