Spontaneous Rupture of Adenocarcinoma of Meckel’s Diverticulum- A Rare Entity
Jayabal Pandiaraja1
1 Senior Resident, Department of General Surgery, Govt. Stanley Medical College and Hospital, Chennai, Tamilnadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jayabal Pandiaraja, 26/1, Kaveri Street, Rajaji Nagar, Villivakkam, Chennai- 600 049, Tamilnadu, India. E-mai : dr.pandiaraja@gmail.com
Meckel’s diverticulum is a true diverticulum from remnant of vitelline duct. It is most common congenital anomaly of intestine. It is associated with intestinal atresia and anorectal anomalies. It contains heterotrophic epithelium. Most common heterotrophic mucosa is gastric followed by pancreatic tissue. Adenocarcinoma arising from Meckel’s diverticulum is very rare. Spontaneous perforation of adenocarcinoma rarely reported. Most of perforation reported in Meckel’s diverticulum diagnosed during intraoperative period. This is a case report of spontaneous rupture of adenocarcinoma of Meckel’s diverticulum, which was managed with primary resection and ileostomy.
Benign disease, Vitelline duct, Ileostomy
Case Report
A 55-year-old male patient reported to the general surgery department with complaints of abdominal pain for 10 days and vomiting for 5 days. Patient also complained of constipation for 3 days duration. There was a history of loss of appetite and lose of weight. Abdominal examination showed distended abdomen with guarding and rigidity. On auscultation bowel sound was absent. Investigations showed anemia with leucocytosis. Erect abdominal X-ray showed dilated small bowel with gas under diaphragm. CT abdomen showed dilated small bowel with free fluid [Table/Fig-1].
CT abdomen showed dilated small bowel with free fluid

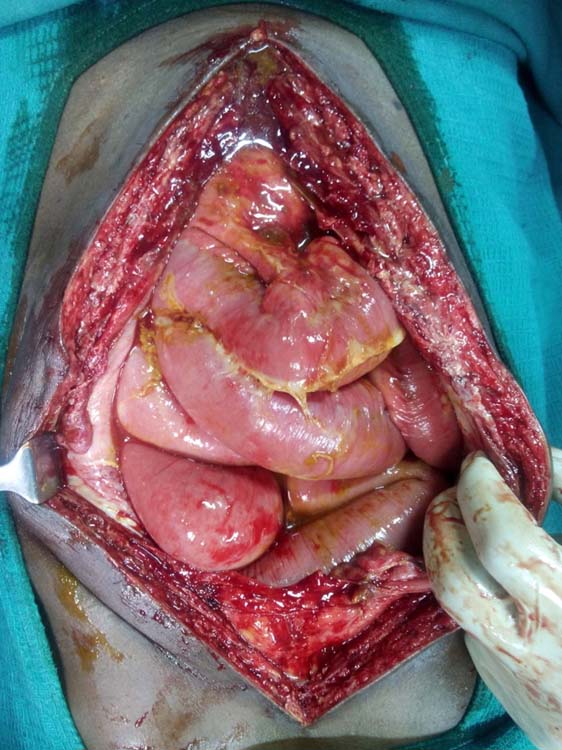
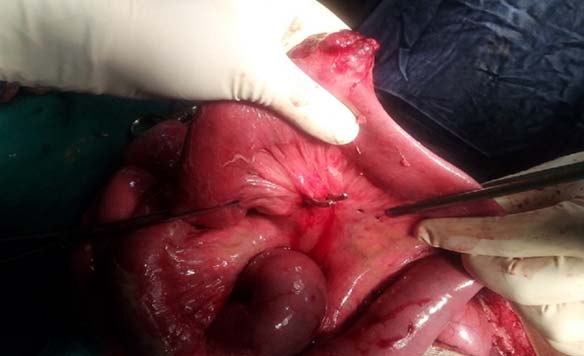
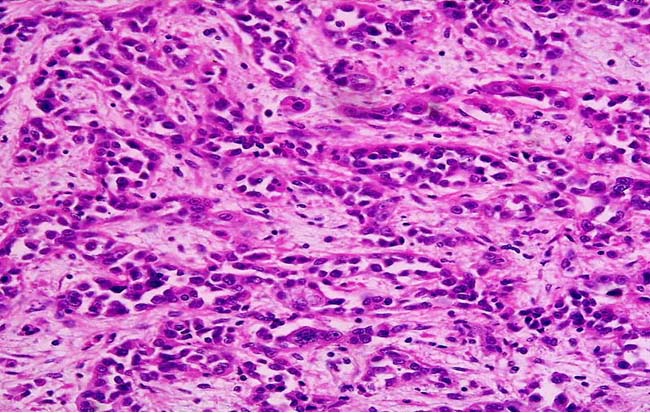
Preoperative diagnosis made as hollow viscus perforation and proceeded with laparotomy. Intraoperative findings were feculent fluid with pus [Table/Fig-2]. Stomach, duodenum and pancreas were normal. An ulceroproliferative growth was present in distal ileum along the antimesentric border which was hard in consistency [Table/Fig-3]. A single perforation was noted in the ulceroproliferative growth which measured about 0.5x0.5cm. Rest of the organs was found to be normal. Primary resection and ileostomy was done, because peritoneal cavity was highly contaminated. Peritoneal cavity was irrigated with normal saline. Abdomen closed in layers with drain tube. Postoperative recovery was uneventful. Histopathological examination showed adenocarcinoma arising from the ectopic gastric mucosa with negative resected margin [Table/Fig-4].
Intraoperative findings were feculent fluid and flakes with dilated small bowel loops
An ulceroproliferative growth was present in distal ileum along the antimesentric border with single perforation was noted in the ulceroproliferative growth which measured about 0.5x0.5cm
Glands show marked architectural distortion with crowding. The epithelial cells show cytological evidence of malignancy with variation in nuclear size and shape, hyperchromasia, increased and abnormal mitoses (H&E stain with 400X)
Discussion
Most of the Meckel’s diverticulum (MD) is asymptomatic. It is only symptomatic when it is associated with complications. Most common presentation in children is gastrointestinal bleeding; whereas in adult is intestinal obstruction [1]. The main complications associated with Meckel’s diverticulum is gastrointestinal bleeding, intestinal obstruction, ulceration, perforation, intussusceptions and malignant transformation. The incidence of malignant transformation of Meckel’s diverticulum ranges from 1-5% [2]. Both benign as well as malignant tumours can occur in Meckel’s diverticulum. Most common malignant tumour arising from Meckel’s diverticulum is carcinoid tumour. Adenocarcinoma arising from Meckel’s diverticulum is extremely rare and it carries poor prognosis [3].
Age of presentation of adenocarcinoma and carcinoid in MD varies. Adenocarcinoma present earlier than malignant Carcinoid tumour. Most of the adenocarcinoma arising from MD either mucinous or signet cell [4]. It usually present as acute abdomen or intestinal obstruction. Most of the adenocarcinoma of MD will have either metastasis or adjacent organ infiltration due to delay in the presentation [5]. There is no specific investigation for the diagnosis. Few case reports showed elevation of CEA level but not diagnostic. It is usually diagnosed during intraoperative period or following histopathology report [6].
Perforation of Meckel’s diverticulum occurs in both benign as well as in malignant disease. Benign disease includes presence of ectopic gastric mucosa [7], perforation following blunt and penetrating injury abdomen [8], ingestion of foreign body like fish bone or chicken bone [9] and formation of stone in Meckel’s diverticulum [10]. Malignant disease includes gastrointestinal stromal tumour [11–13], adenocarcinoma of Meckel’s diverticulum and Carcinoid tumour.
Most of the Meckel’s diverticular perforation misdiagnosed as appendicular perforation or hollow viscus perforation. Most of the time imaging system failed to identify perforated Meckel’s diverticulum. Perforated Meckel’s diverticulum diagnosed while doing laparoscopy or open procedure for other differential diagnosis for perforation.
As we know MD associated with age less than 50 years, male sex, and diverticulum more than 2 cm and persistence of abnormal tissue needs diverticulectomy in asymptomatic MD. But few studies and case report shows even presence of asymptomatic MD advised for diverticulectomy because of morbidity following surgery is negligible compared to the complication and associated malignant transformation [14]. Presence of gross abnormal mucosa in MD needs segmental resection rather than diverticulectomy because positive margin and surgical morbidity following reresection is high [6]. Most of the adenocarcinoma arising from MD need either segment resection or palliative resection along with adjuvant therapy [15].
Conclusion
Most of the Meckel’s diverticulum is asymptomatic, but it can present with wide range of complication. Most of the Meckel’s diverticular perforation misdiagnosed as appendicular perforation or hollow viscus perforation. Malignant transformation of Meckel’s diverticulum associated with poor prognosis. Adenocarcinoma of Meckel’s diverticulum carries poor prognosis compared to malignant Carcinoid. Incidental finding of Meckel’s diverticulum need diverticulectomy because surgical morbidity was less compared to complication. Presence of gross abnormal tissue in Meckel’s diverticulum need segmental resection rather than diverticulectomy because positive margin and surgical morbidity associated with reresection is very high.
[1]. Caracappa D, Gullà N, Lombardo F, Burini G, Castellani E, Boselli C, Incidental finding of carcinoid tumour on Meckel’s diverticulum: case report and literature review, should prophylactic resection be recommended?World J Surg Oncol 2014 12:144 [Google Scholar]
[2]. Carpenter SS, Grillis ME, Meckel’s diverticulitis secondary to carcinoid tumour: an unusual presentation of the acute abdomen in an adultCurr Surg 2003 60(3):301-03. [Google Scholar]
[3]. Lee JK, Kwag SJ, Oh ST, Kim JG, Kang WK, Adenocarcinoma arising from Meckel’s diverticulum in the ileum with malrotation of the midgutJ Korean Surg Soc 2013 84(6):367-70. [Google Scholar]
[4]. Ramírez-González LR, Leonher-Ruezga KL, Plascencia-Posadas FJ, Jiménez-Gómez JA, López-Zamudio J, Fuentes-Orozco C, Adenocarcinoma mucoproductor in Meckel’s diverticulum. Case report and reviewCir Cir 2014 82(2):200-05. [Google Scholar]
[5]. Sakpal SV, Babel N, Pulinthanathu R, Denehy TR, Chamberlain RS, Krukenberg tumour: metastasis of Meckel’s diverticular adenocarcinoma to ovariesJ Nippon Med Sch Nippon Ika Daigaku Zasshi 2009 76(2):96-102. [Google Scholar]
[6]. Lesquereux-Martínez L, Macías-García F, Beiras-Sarasquete C, Martínez-Castro JJ, Paulos-Gómez AM, Beiras-Torrado A, Adenocarcinoma arising in Meckel’s diverticulum: a case report and literature reviewGastroenterol Hepatol 2011 34(3):137-40. [Google Scholar]
[7]. Grasso E, Politi A, Progno V, Guastella T, Spontaneous perforation of Meckel’s diverticulum: case report and review of literatureAnn Ital Chir 2013 84:piiS2239253X13020902 [Google Scholar]
[8]. Ekwunife CN, Mbadugha TN, Ogbue UN, Isolated Meckel’s diverticulum perforation as a sequel to blunt abdominal trauma: a case reportJ Med Case Reports 2014 8:111 [Google Scholar]
[9]. Chan KW, Perforation of Meckel’s diverticulum caused by a chicken bone: a case reportJ Med Case Reports 2009 3:48 [Google Scholar]
[10]. Thiyagarajan UM, Ponnuswamy A, Bagul A, Ponnuswamy P, Perforated Meckel’s Diverticulum Lithiasis: An Unusual Cause of PeritonitisCase Reports in Surgery 2013 2013:8256283 pages,. doi:10.1155/2013/825628 [Google Scholar]
[11]. López-Tomassetti Fernández EM, Hernández Hernández JR, Nuñez Jorge V, Perforated gastrointestinal stromal tumour in Meckel’s diverticulum treated laparoscopicallyAsian J Endosc Surg 2013 6(2):126-29. [Google Scholar]
[12]. Mitura K, Blicharz P, Romanczuk M, Perforated gist of Meckel’s diverticulumPol Przegl Chir 2012 84(5):258-61. [Google Scholar]
[13]. Chou YH, Tu CC, Huang CC, Hsieh MS, A clinically-occult gastrointestinal stromal tumour in a Meckel’s diverticulum presenting as hollow organ perforationChang Gung Med J 2011 34(6 Suppl):56-61. [Google Scholar]
[14]. Thirunavukarasu P, Sathaiah M, Sukumar S, Bartels CJ, Zeh H, Lee KKW, Meckel’s diverticulum—a high-risk region for malignancy in the ileum. Insights from a population-based epidemiological study and implications in surgical managementAnn Surg 2011 253(2):223-30. [Google Scholar]
[15]. Parente F, Anderloni A, Zerbi P, Lazzaroni M, Sampietro G, Danelli P, Intermittent small-bowel obstruction caused by gastric adenocarcinoma in a Meckel’s diverticulumGastrointest Endosc 2005 61(1):180-83. [Google Scholar]