Quality of life is the degree in which a human can enjoy the important opportunities of life. In the other words Quality of life (QOL) is the general well-being of individuals and societies [1]. Successful aging is depended on preserving a good quality of life which in turn is related to different aspects of health [2]. Oral health is an integrated part of general health. The world health organization has introduced oral diseases as a public health problem due to its high prevalence and incidence worldwide [3]. Oral health related quality of life (OHR-QoL) is defined as a multidimensional assessment of effects of oral functions on patient well-being [4–7]. Dental and oral problems can impact on nutrition intake. Due to systemic problems, any infectious source in oral cavity can compromise general health. Some malignancies are more prevalent in this age group which can in turn affect patient survival. These disorders must be diagnosed and managed appropriately by dentists to treat disease, restore function, and improve the quality of a person’s life.
This study was conducted to evaluate OHR-QoL in a group of elderly patients referred to Mashhad dental school (MDS) for oral and dental problems and to compare them with a group of normal population by using Persian version of OIDP. Also, this study was planned to show if patients with oral and maxillofacial diseases (dental, periodontal or oral diseases, jaw problems, salivary pathologies, etc) had worse OHL-QoL than patients with isolated dental and periodontal diseases.
Materials and Methods
There are two groups in this study: 1) case group which consists of elderly patients referred for different oral, dental and maxillofacial complaints to Mashhad Dental School (MDS); and 2) control population which consists of a group of normal elderly people with no oral, dental and maxillofacial complaints made them seek care.
Sample size was calculated due to mean difference in two groups upon a pilot survey, (α=0.05, β=0.2) by 20 cases in each group. Based on pilot study, 119 cases assigned to be included in each group. Considering outflow, a total of 300 elderly patients (150 for each group) were invited in this cross-sectional study from February 2009 to February 2011 by face-to-face contact. The sampling method was purposive in both groups. The participants were informed about the interview and assured of the confidentiality of the collected information and only those who gave consent were included in the research. Inclusion criteria: 1) being elderly (>60 years old); 2) seeking care in MDS (for case group); 3) coming for visiting holy shrine of Imam Reza (for control group); 4)being resident of Mashhad; 5) Verbal consent to participate in this study. Exclusion criteria 1) loss of orientation or recall (e.g. memory deficit, mental problems); 2) having any oral, dental or maxillofacial compliant in control group (due to dental or oral problems or deleterious oral habits: smoking, alcohol...).
Sixty four subjects were excluded due to disagreement for participation in the survey (N=50) and loss of exact demographic data (N=14). Twenty three patients had incomplete items in OIDP forms so they were excluded from the survey. Two hundred and thirteen elderly patients (>60-year-old) were eligible for this study. A total of 99 elderly patients referred to MDS for different dental and oromaxillofacial complaints were chosen. One hundred and fourteen (114) elderly people who came to visit the holy shrine of Imam Reza were chosen as control group. We used this group as control because visitors of holy shrine in Mashhad are relatively a true sample of elderly people (excluding non residents of Mashhad).(1) They were chosen because they had no oral and maxillofacial compliant. This statement was asked verbally from the control sample (OIDP measures self-reported oral health status not the real status).
Data were collected through face to face interview performed by a trained dentist by using Persian version of OIDP questionnaire [1,12]. During the interview the examiner registered demographic data and the OIDP index was calculated for each patient. It consistes of six questions which assess severity and frequency of impairment in 11 common daily functions. Dorri et al., evaluated the validity and reliability of Persian version of the OIDP index in a sample of 285 Iranian population, and concluded that the index is valid and reliable for use in this population [1]. The interviewee answered all the questions. The items addressed various aspects of a typical daily routine, including eating, speaking, denture or tooth cleaning, light activities (performing normal daily activities like walking), going out, sleeping, smiling, emotional stability, enjoying social contacts, and performing occupational tasks. Frequency and severity of impairment of daily activity (qualitative data) and the assigned value (quantitative data) were recorded. Interviewees linked each of the recorded data with one or more oral conditions. This data were used for analysis of special conditions.
Performance score for each function was calculated as follows:
Performance score = Severity score × Frequency score
Total performance score =Σ Performance score/ (11×35)
The total performance score was calculated by dividing the Performance score by the maximum possible score.
Statistical Analysis
The items, addressed various data from case and control groups, were compared. Data were entered to SPSS 11.5 soft ware for windows (SPSS, Chicago IL), classified and converted into SPSS file format for analysis. Statistical analysis was performed using the Chi-square test, analysis of variance (ANOVA), and t-test. When distribution of data was not normal Mann-Whitney test was used. A p-value less than 0.05 were considered significant.
Results
A total of 213 patients were enrolled in this study (case group=99, control group=114). Mean age of patients was 67.82±6.47 (case=67.13±6.39; control=68.58±6.50). Mean Performance score (MPS) was 6.27±10.47. MPS was 7.96±11.95 in case group and 4.80±8.77 in control group. The difference in MPS between case and control groups was significant (95%CI= -5.96 to-0.35, p=0.015). No significant difference between males and females, in total sample or in each study group was found (p=0.41).
The age was not significantly different between two groups (p=0.12). [Table/Fig-1] shows gender distribution of patients in two groups. [Table/Fig-2] shows occupation of patients which was similar in two groups. Occupation was not related with OIDP score. Most patients were from rural areas (N=203, 96%).
Distribution of patients in two study groups due to gender
| Gender | Normal group | MDS group | Total | p-value=0.41 |
|---|
| Male | 59(52%) | 61(62%) | 120(56.33%) | 0.68 |
| Female | 55(48%) | 38(38%) | 93(43.66%) |
| Total | 114(100%) | 99(100%) | 213(100%) |
Carrier of patients in two study groups
| Occupation | Normal group | MDS group | Total | p-value |
|---|
| Unemployed or housewives | 73(64%) | 81(82%) | 154(73.31%) | 0.02 |
| employee | 41(36%) | 18(18%) | 59(27.69%) |
| Total | 114(100%) | 99(100%) | 213(100%) |
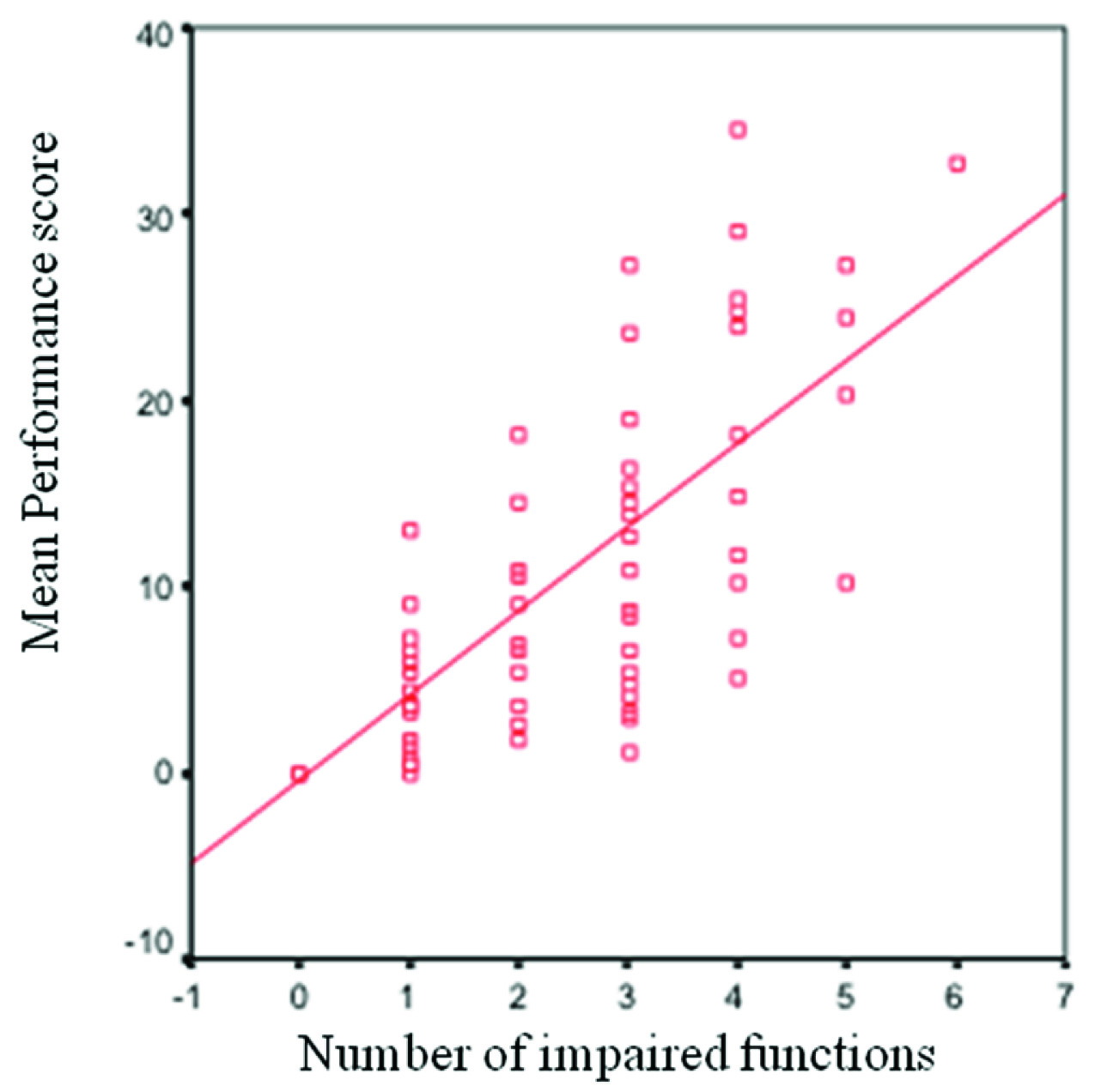
With increasing age, MPS decreased which shows better OHR-QoL. It can be inferred that age is conversely correlated with MPS (r= -0.0125, p=0.24) and older elderly people can cope better with their oromaxillofacial complications although this correlation was not significant. [Table/Fig-3] shows correlation between number of impaired functions and MPS. With increased in number of impaired functions, MPS was increased which shows decrease in quality of life. In other word MPS was directly correlated with number of impaired functions (r=0.92, p<0.001). Another interesting finding is that with increase in age, the number of impaired function is decreased. So age was indirectly correlated with number of impaired functions (r=-0.134, p=0.21) but this correlation is not statistically significant.
Correlation between the number of impaired functions and MPS: mean performance score (MPS) in the vertical axis is directly correlated with number of impaired functions in the horizontal axis.
Of those who had impaired functions, 31.9% had one impaired function. [Table/Fig-4] shows number of impaired functions in case group and [Table/Fig-5] demonstrates impaired daily functions in two study groups. Function “Eating” was impaired by different situations. Among these situations: ill-fit denture (31/213=14.55%), oral ulcers (24/213=11.26%) and pain (21/213=9.85%) were main responsible for impaired eating. “Speaking” was impaired mainly by tooth mobility (11/213=5.16%) and ill-fit dentures (2/213=4.22%). “Cleaning teeth” was impaired in four patients by toothache (2/213=0.93%). “Going out” was impaired by halitosis (6/213=2.81%), ill-fit dentures (4/213=1.87%). “Sleeping” was impaired by pain (7/213=3.28%), ill-fit dentures and ulcers (each one 1.40%). “Relaxing” was impaired by pain (6/213=2.81%), ill-fit dentures and ulcers and tooth mobility and caries (each one 1.40%). “Smiling” was impaired by tooth discolouration (3/213=2.81%), tooth malposition and discolouration and tooth mobility (2/213=0.93%). “Emotional status” was negatively affected by ill-fit dentures, pain and halitosis (each one 3/213=1.40%). “Social contacts” was impaired mainly by halitosis (6/213=2.81%) and ill-fit dentures and tooth discolouration (each one 4/213=1.87%).
Number of impaired functions in study population
| The number of impaired functions | Percentage of involved patients |
|---|
| 1 | 32% |
| 2 | 6.6% |
| 3 | 9.8% |
| 4 | 6.6% |
| 5 | 3% |
Impaired daily functions in two study groups
| Study Groups | Normal group | MDS group | Total | Total study population | p-value |
|---|
| Impaired functions | Yes | No | Yes | No | Yes | No |
|---|
| Eating | 52 | 162 | 38 | 61 | 90 | 123 | 213 | 0.28 |
| Speaking | 98 | 16 | 73 | 26 | 17 1 | 43 | 213 | 0.02* |
| Cleaning teeth | 114 | 0 | 94 | 5 | 208 | 5 | 213 | 0.02* |
| Physical activities | 114 | 0 | 95 | 4 | 209 | 4 | 213 | 0.02* |
| Going out | 105 | 9 | 92 | 7 | 197 | 16 | 213 | 0.08 |
| Sleeping | 105 | 9 | 91 | 8 | 196 | 17 | 213 | 0.09 |
| Relaxing | 105 | 9 | 93 | 6 | 198 | 15 | 213 | 0.60 |
| Smiling | 108 | 6 | 88 | 11 | 196 | 17 | 213 | 0.11 |
| Emotional status | 109 | 5 | 83 | 16 | 192 | 21 | 213 | 0.00* |
| Social contacts | 110 | 4 | 83 | 16 | 193 | 20 | 213 | 0.00* |
| Working | 113 | 1 | 96 | 3 | 209 | 4 | 213 | 0.34 |
*Significant difference between MDS and Normal group
Frequency of patients with oral diseases (oral immunologic ulcers, atypical facial pain, burning mouth syndrome, etc.) was significantly higher in case group (p<0.001). We could not show any significant difference in MPS of patients with oral diseases in case group compared to other patients with dental and periodontal problems.
Discussion
As we anticipated, OHR-QoL of patients with oromaxillofacial complaints was impaired more than normal group. Impaired speaking, emotional status, cleaning teeth, physical activity and social contacts were experienced more among case group. Different situations could impair daily functions. Ill-fit dentures were responsible in most impaired functions (9 of 11 daily functions were impaired by ill-fit dentures). Gender was not an important determinant in our study because no significant difference was found in either whole study sample or each group. Similarly, Fuentes-Garcíain a comparison of OHR-QoL in three cities of Brazil reported that sex was not an important determinant in GOHAI scores [8]. They indicated that socio-economic inequalities affected oral health status and OHR-QoL. In our study occupation of the patients was not related to OHR-Qol. Other factors affecting socio-economic inequalities were not assessed in our study since we had focused on oral and maxillofacial problems rather than socio-economic factors. Wang found that self-rated oral health, number of missing teeth, satisfaction with oral health and satisfaction with life were major factors in OHR-QoL [13]. Number of missing teeth was not a major determinant in our study, but ill-fit dentures, pain and halitosis were most influencing factors in our study.
Ikebe showed that gender and age are not significantly related in OHR-QoL but oral health impact profile (OHIP-14) scores were related with lower self-assessed general health, fewer residual teeth, and subjective oral dryness and dissatisfied with financial status [14]. In another study Ikebe found masticatory performance as a related function [15]. With increase in age some controversial issues are evident in our survey. For example with increasing age, MPS was decreased and older elderly people can couple better with their oromaxillofacial complaints. Similarly, Laraway et al., showed that older patients with head and neck cancer adjusted and coupled better than younger patients, when physical and socio-economic domain was assessed [16]. Other studies have not showed such correlation. We found that with increase in age, the number of impaired functions was decreased which in turn can improve OHR-QoL.
Ill-fit dentures were responsible situation in most impaired daily functions (9 out of 11 daily functions). Dissatisfaction with denture can be an important factor in OHL-QoL. Albaker showed that patients with both jaws denture have worse OHR-QoL than patients with single complete denture [17]. Locker found that main oral problems that can impair OHR-QoL are missing teeth, dry mouth and Limitation in chewing capacity but our study can not confirm such findings [18]. Yu in a survey on impact of oral health status on OHR-QoL in Chinese hospitalized geriatric patients. Found that decayed teeth, lack of occluded teeth, coated tongue, excessive tartar, dry and rough red oral tissue and diseased gum were the main problems affecting OHL-QoL [19]. Such findings were not showed in our study perhaps because of different setting of study (hospital vs clinic). In another study in Brazilian elderly by Silva the major impacts were related to feeling conscious of psychological discomfort (28.1%) and difficulty eating (24.4%) due to teeth, mouth or dentures. Some parts of this result can be confirmed by our study, especially with ill-fit dentures as a major determinant. Higher scores were related to non-White individuals, those with depressive symptoms, tobacco users, non-denture wearers, those with a perceived need for dental treatment and those with poor or very poor self-rated oral health and Lower scores were found among individuals aged 80 years or older and those with higher income [20]. We showed that the more the age of patient, the better he/she can compatible with dental, oral and maxillofacial problems. Our results are in agreement with Silva which considered age as a reverse affecting issue. We didn’t comprise income because we did not ask the income of cases due to cultural issues. Yashioka suggested that “subjective masticatory ability” might be a good landmark for quality of life of elderly people in addition to the number of remaining teeth [21]. Subjective masticatory ability was not assessed in OIDP forms. We found, in oromaxillofacial functions, ill-fit dentures, oral ulcers, pain and tooth mobility were major determinants of OHR-QoL whereas in social functions such as smiling, emotional status, going out and social contacts, halitosis, tooth malposition and tooth discoloration are major issues. This difference can be due to variable complaints or cultural differences. Although frequency of oral diseases (other than dental and periodontal problems) was higher in case group than control group, no significant correlation was found between oral diseases and OHR-QoL.
Limitations
This study has some limitations: 1) two study groups are not matched considering employment; 2) the primary oral needs of patients are not exactly indicated –this was not our goal - which could be useful for organizing health policies and insurances; 3) We had a considerable outflow so further studies must be planned with a greater sample size so that more reliable results can be obtained.
Conclusion
Since some daily functions were impaired in patients referred to MDS in comparison with control group, more attention must be paid to oral and maxillofacial diseases to improve quality of life in elderly patients. Speaking, emotional status, cleaning tooth, physical activity and social contacts were impaired more than other daily functions. Ill-fitting denture was responsible for this impairment in most cases. Results of this study could not be generalized to all elderly people unless more research is performed.
*Significant difference between MDS and Normal group