The human spinal column is composed of a series of vertebrae alternating with intervertebral discs that extend from the cranium to the coccyx. This resilient cylindrical column essentially protects the spinal cord and plays an important role in posture and locomotion. Although their basic structure is similar, vertebrae vary in size and exhibit regional characteristics. The 7 cervical, 12 thoracic and 5 lumbar vertebrae are termed free while the 5 sacral and 4 coccygeal vertebrae are fixed. Out of the 33 vertebrae, the cervical vertebrae are easily recognizable by the presence of foramina transversaria in their transverse processes. Regardless of the fact that the cervical vertebrae are the smallest, they exhibit the greatest range and variety of movements that makes them prone to a diverse array of traumatic and degenerative conditions. For better management of diseases and mechanical processes, countless researchers have investigated the diverse aspects of human cervical spine, foremost being the anatomy, kinematics and mechanical properties of cervical vertebrae as well as intervertebral discs [1]. As spinal ailments are frequently managed by arthrodesis which involves surgical fusion of adjacent degenerated vertebrae with plates and screws, accurate placement of screws is of paramount importance to circumvent damage to the vertebral artery, spinal medulla or nerve roots [2]. The commonest form of arthrodesis is anterior cervical plate fixation. In cases where there is restricted accessibility from anterior aspect of bone mass, another technique known as posterior lateral mass screw fixation is employed. A further superior approach of arthrodesis is trans-pedicular screw fixation wherein pedicles of adjacent vertebrae are held together with screws [1].
Differences exist in cervical spine morphometric values across different study populations [3]. So far, out of the studies available, few determine the morphometry of sub-axial cervical vertebrae, especially in the Indian population. The present study quantifies morphometric charteristics of the typical cervical vertebrae (C3-C6) which are mandatory for safe screw placement during surgical instrumentation of the cervical spine.
Materials and Methods
The present study included 203 typical cervical vertebrae which were part of the osteological collection of the Department of Anatomy. Vertebrae that were damaged or those with bony spurs/deformities, which may influence linear measurements, were excluded from the study and only intact vertebrae in good condition were studied and photographed. All linear measurements were ascertained using digital Vernier calliper with 0.01mm precision while angular measurements were recorded with software Image J.
Mean and standard deviations of the following dimensional and angular parameters were calculated:
Linear Parameters
Body
Antero-posterior diameter, measured as the midline antero-posterior distance between the anterior and posterior borders of superior surface of the vertebral body [Table/Fig-1].
Typical cervical vertebra; Superior view, (B1)- Antero-posterior diameter of vertebral body; (B2)-Transverse diameter of vertebral body; (P1)-Length of pedicle; (P2)- Width of pedicle, (S1)- Length of superior articular process; (S2)-Width of superior articular process; (Sp)- Length of spinal process; (A)-Pedicle transverse angle
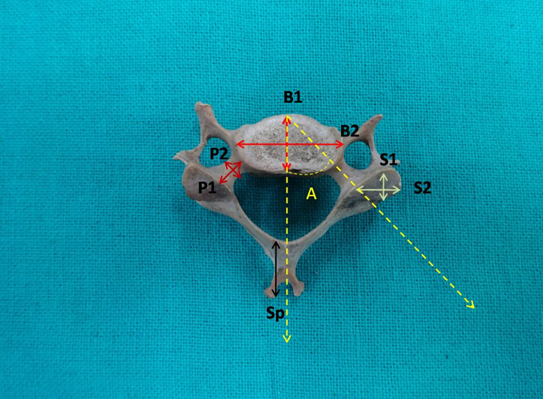
Transverse diameter: The maximum transverse distance of superior surface of the vertebral body [Table/Fig-1].
Height: The midline vertical distance between superior and inferior border of the anterior surface of the vertebral body [Table/Fig-2].
Typical cervical vertebra, Anterior view: (B3)-Height of vertebral body

Pedicle
Length: The distance between the anterior margin of superior articular facet and posterior margin of vertebral body [Table/Fig-1].
Width: Distance between the medial and lateral border of pedicle [Table/Fig-1].
Laminae
Height: Midline distance between superior and inferior border of laminae [Table/Fig-3].
Typical cervical vertebra, Posterior view: (L1)- Transverse length of lamina, (L2)-Height of lamina
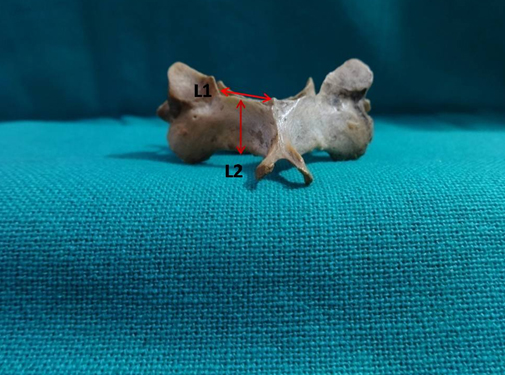
Transverse length: The distance between spine and lateral border of superior articular facet along superior border of lamina [Table/Fig-3].
Spine
Length: The distance from anterior end of the spine to the longest tip of the bifurcated spine [Table/Fig-1].
Superior articular process
Length: The maximum distance between superior and inferior border of the superior articular process [Table/Fig-1].
Width: Maximum transverse diameter of superior articular process [Table/Fig-1].
Inferior articular process
Length: Maximum distance between superior and inferior border of the inferior articular process [Table/Fig-4].
Typical cervical vertebra; Inferior view: (i1)-Length of inferior articular process, (i2)- Width of inferior articular process
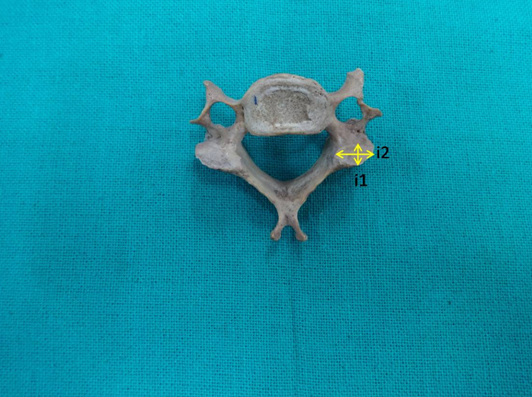
Width: Maximum transverse diameter of inferior articular process [Table/Fig-4].
Angular parameter
Pedicle transverse angle (PTA): The angle between pedicle axis and the sagittal plane [Table/Fig-1].
Statistical Analysis
The mean and standard deviations of the linear and angular parameters were calculated. The comparison of morphometric dimensions of the right and left sides was performed using Student’s t-test and p-value was calculated.
Results
A total of 203 typical cervical vertebrae from C3-C6 were examined in the present study. The vertebrae were analysed for the above mentioned parameters.
Linear parameters: Mean antero-posterior and transverse diameters of the vertebral body were 14.84 ± 1.44 mm and 22.18 ± 2.52 mm respectively, while mean height obtained was 11.39 ± 1.08 mm.
The mean length of the pedicle was noted to be more on the right side when compared to the left and same held good for the pedicle width though these differences were not statistically significant.
Mean height and length of the lamina were 10.82 ± 1.18 mm and 14.53 ± 1.57 mm, respectively. There was no statistical difference between the right and left sides.
Mean length of the spinous processes was 16.61 ± 2.50 mm with no statistically significant difference between the two sides.
The mean length and width of the superior articular process was found to be more on the left side and a highly significant difference (p-value= 0.002) existed for the width.
Similarly, when the mean length (9.15 ± 1.03 mm) and width (11.89 ± 0.64 mm) of the inferior articular process was obtained, a highly significant difference existed for the width.
Angular parameters: The mean pedicle transverse angle from C3 to C6 was 44.470 ± 2.81mm. There was no significant statistical difference between PTA of the right and left pedicles.
([Table/Fig-5] summarizes mean and standard deviation of each measurement.)
Morphometric measurements of typical cervical vertebrae (C3-C6)
| Morphometric measurements | Right | Left | mean value | p value |
|---|
| Antero-posterior diameter of vertebral body | | | 14.84 ± 1.44 mm | _ |
| Transverse diameter of vertebral body | | | 22.18 ± 2.52 mm | _ |
| Height of vertebral body | | | 11.39 ± 1.08 mm | _ |
| Length of pedicle | 4.55 ± 0.82 mm | 4.47 ± 0.68 mm | 4.51 ± 0.66 mm | 0.592 |
| Width of pedicle | 4.64 ± 0.53 mm | 4.47 ± 0.54 mm | 4.56 ± 0.43 mm | 0.268 |
| Length of superior articular process | 10.08 ± 1.19 mm | 10.72 ± 1.31 mm | 10.4 ± 1.14 mm | 0.014 |
| Width of superior articular process | 11.18 ± 1.06 mm | 10.69 ± 1.17 mm | 10.93 ± 1.07 mm | 0.002 |
| Length of inferior articular process | 9.38 ± 1.39 mm | 8.92 ± 1.08 mm | 9.15 ± 1.03 mm | 0.14 |
| Width of inferior articular process | 12.52 ± 0.96 mm | 11.26 ± 1.14 mm | 11.89 ± 0.64 mm | 0.002 |
| Length of spinous process | 16.71 ± 2.53 mm | 16.51 ± 2.66 mm | 16.61 ± 2.50 mm | 0.507 |
| Height of lamina | 10.81 ± 1.21 mm | 10.82 ± 1.24 mm | 10.82 ± 1.18 mm | 0.913 |
| Transverse length of lamina | 14.51 ± 1.74 mm | 14.54 ± 1.55 mm | 14.53 ± 1.57 mm | 0.88 |
| Pedicle transverse angle | 44.410 ± 3.32 | 44.530 ± 2.73 | 44.470 ± 2.81 | 0.809 |
Discussion
Instrumentation involving cervical spine necessitates detailed anatomical knowledge which is useful in designing spinal implants and to avoid damage to regional vital structures, but variability in vertebral dimensions exist amongst different races and prevents the standardization of measurements [3]. This has led many researchers to describe the morphological characteristics of the vertebral column and study its dimensions via direct measurement and by CT scans of bony specimens. In the present study we have endeavoured to analyse cervical vertebrae morphometry and provide a reference database for designing customized spinal implants and screws for Indian population. Such data also allows for comparison with other study populations and enables identification of osteological remains, especially of Indian population.
Body: The typical cervical vertebrae possess transversely elongated bodies. The superior surface has elevated posterior and lateral margins along with a depressed anterior margin, giving the vertebral bodies a somewhat seat like appearance. Such a sculpted superior surface enables free flexion and extension but limits lateral flexion and rotation. During anterior cervical reconstructions, surgeons require the antero-posterior diameter of the vertebral bodies to fix the bicortical screws [3]. Bazaldua CJJ et al., studied cervical vertebrae in Mexicans and reported a mean antero-posterior diameter slightly larger (16.08 mm) than that reported by Tan SH et al., (14.1 mm) in Singaporean population and as per the present study in Indians (14.84 mm) [3,4]. The mean transverse diameter of the vertebral body reported by Bazaldua CJJ et al., (21.31 mm) and Tan SH et al., (14.8mm) was less than what we found in the Indian population (22.18 mm). The anterior vertebral body height was 10.2 mm as reported by Tan SH et al., which was less in comparison to present study [Table/Fig-6]. Thus, the vertebral bodies are transversely longer in Indian populations. Such variations emphasize the need to take into account the racial differences during surgical procedures [3].
Morphometry of vertebral body C3-C6 (mm)
| Present study | Bazaldua (2011) | Tan (2004) |
|---|
| Mean Antero-posterior diameter | 14.84 | 16.08 | 14.1 |
| Mean Transverse diameter | 22.18 | 21.31 | 14.8 |
| Mean Height | 11.39 | _ | 10.2 |
Pedicles: The pedicles are short cylindrical processes projecting backwards from the body that meet the laminae posteriorly. The vertebral notching observed on the superior and inferior aspects of the pedicle, helps to form the intervertebral foramina for the passage of spinal nerves. Thus pedicle length and width are essential parameters for screw size selection during trans-pedicular fixation surgery. Though technically challenging, the maximum stability of the cervical spine is offered by trans-pedicular screw fixation but it risks damage to the adjacent neurovascular structures. Such potential complications may be avoided if the detailed cervical pedicle anatomy is obtained beforehand as well as the appropriate surgical techniques and implant designs are decided upon. In our present study, pedicle measurements in Indian population were comparable to that reported by Bazaldua CJJ et al.,, Vergas-Mena R et al., in Mexican population and Tan SH et al., in Singaporean population [2–4]. Other populations: Thai (Chanplakorn P et al.,), Egyptian (Eldin MMM), British (Hacker AG et al.,), Turkish (Kayalioglu G et al.,), (Bozbuga M et al.,), (Ugur HC et al.,), American (Rao RD et al.,), (Ludwig SC et al.,) (Ebraheim NA et al.,) Stanescu S et al.,) presented higher values than ours [5–14] [Table/Fig-7]. From the surgical perspective, minute divergence in cervical pedicle dimensions is a constant feature, but in Indian population it may play a decisive role as the size of the pedicle is relatively smaller than other populations. In cases of disparity between pedicle and screw length, the pedicle wall may be breached along with infringement of the vertebral canal space [5].
Comparison of pedicle dimensions with previous studies
| Author (Year) | Mean Length (mm) | Mean Width (mm) | Mean pedicle transverse Angle (degree) |
|---|
| Present study | 4.51 | 4.56 | 44.47 |
| Chanplakorn (2014) | - | 5.16 | 43.18 |
| Eldin (2014) | 7.06 | 5.18 | 42.5 |
| Bazaldua (2011) | 4.53 | 4.81 | - |
| Vergas Mena (2011) | - | 4.76 | 43.61 |
| Rao RD (2008) | 5.46 | 5.66 | 45.83 |
| Hacker (2008) | - | 5.43 | 48.93 |
| Kayalioglu (2007) | 5.83 | 4.72 | - |
| Bozbuga (2004) | 5.75 | 4.65 | 46.9 |
| Tan (2004) | - | 4.76 | 41.28 |
| Ugur (2000) | - | 5.28 | 44 |
| Ludwig (1999) | 15.8 | 5.91 | 41.64 |
| Ebraheim (1997) | 6.1 (C6) | 4.85 | - |
| Stanescu (1994) | 4.9 (C5-C6) | 5.75 | 50 (C5) |
The ideal entry point and trajectory for cervical pedicle screw insertion is established by pedicle transverse angle (PTA). We found the mean pedicle transverse angle in Indians to be 44.470 ± 2.81. A great disparity of the PTA was noted in different populations: Eldin MMM, Tan SH et al., Chanplakorn P et al., and Ludwig SC et al., reported lower value than ours while Hacker AG et al., Bozbuga M et al., Rao et al., and Stanescu S et al., observed higher values of pedicle transverse angle [4,5,7,9–12,14]. As there is no space for the pedicle screws to diverge, preoperative Multi-Detector Computerized Tomography (MD-CT) scans are necessary to individually evaluate, the entry point and trajectories for cervical pedicle screw insertion [5].
Laminae: The flat laminae are a pair of broad bony plates that unite in the midline and complete the vertebral foramen posteriorly. The laminae are critical in maintaining the cervical spine stability [15]. Recently, cervical laminoplasty is being used for spondylotic myelopathy, resection of spinal tumours and ossified posterior longitudinal ligament [16,17]. The laminae also present a consistent intraoperative guide to the contra-lateral pedicle transverse angle during sub-axial cervical pedicle instrumentation [14]. Though, not extensively studied by other researchers, the dimensions of the laminae obtained by us were lesser in comparison to Bazaldua CJJ et al., lesser dimensions of the lamina found in the Indian population may offer a restricted surgical field during cervical laminoplasty.
Spinous Process: The spinous processes show racial variability, being short and bifid in Whites when compared to African races [18]. Screws can invariably be placed in the spinous processes and length of the spinous process assumes importance during screw placement in traumatic or degenerative lesions. As per our study, the mean length of spinous process in Indians was lesser than values reported by Bazaldua CJJ et al., and does not appear favourable for screw placement, as shorter spinous process may splinter.
Superior and inferior articular processes: The bony connection between the superior and inferior articular processes lying between the vertebral canal and the transverse foramen is referred to as the lateral mass. It serves as a dependable site for screw insertion where the integrity of the laminae, pedicle, or spinous process is not required, as in cervical wiring, laminar screws or pedicular screws major. Lateral mass screw fixation has emerged as the technique of choice in stabilizing sub-axial cervical spine as it maintains rotational stability, the facets are not pierced, it is more secure than trans-pedicular screws and does not require intra-operative imaging. The complications of lateral mass screw fixation include: injury to adjacent neurovascular structures or facet joints, weak screw grip due to less cortical bone in the lateral mass and a smaller area left for bony fusion after plate insertion [19]. These drawbacks may be overcome by changing the entry point and trajectory of screws. The dimensions of superior and inferior articular process form the basis for lateral mass screw insertion. We found the mean length and width of the superior articular processes (10.4 ± 1.14 mm and 10.93 ± 1.07 mm respectively) were comparable to the findings of Bazaldua CJJ et al.,. Stemper BD et al., in Americans and Mohamed E et al., in Egyptian populations reported larger lateral mass width than the present study. This may have resulted due to the fact that these researchers took into account the total length and width of the articular processes, rather than just the articular facet size [19,20].
Limitation
Though at the commencement of our study, we had envisaged the inclusion of a range of parameters, the dimensions eventually studied were limited. This was chiefly due to the meticulous nature of manual measurements of 203 vertebrae by digital callipers, which required time and accurate positioning. Further studies are required on the linear and angular parameters of pedicles, facets, laminae, foramen transversaria and spinal canal to complete the morphometric database of sub-axial cervical vertebrae.
Conclusion
The considerable technical challenge encountered during stabilization of the cervical spine is intimidating for surgeons, who require an extensive knowledge of the surgical anatomy of cervical vertebrae. The present comprehensive study yielded the characteristics of the Indian cervical vertebrae. We found the dimensions of the vertebrae to be lesser in Indians when compared to other populations. Such data suggests that procedures like trans-pedicular screw fixation may be hazardous owing to smaller vertebral pedicles. The vast range of the pedicle transverse angle (range: 39.73°- 54.14°) necessitates the need to individualize the entry point and trajectories for pedicle screw insertion according to the patients. Smaller dimensions of the laminae restrict the surgical field while shorter spinous processes are unfavourable for screw placement. We anticipate that our study will be able to provide a reference database for designing implants and for planning the appropriate surgical approach in the cervical vertebrae.