Unusual Presentation of Hepatocellular Carcinoma into Right iliac fossa: A Rare Entity
Murali Uthamalingam1, Karthikumaran Periyasamy2
1 Associate Professor, Department of Surgery, International Medical School, MSU, Malaysia.
2 Senior Resident, Department of Surgery, Ramakrishna Hospital, Coimbatore, Tamilnadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Murali Uthamalingam, Associate Professor, Department of Surgery, Management & Science University, University Drive, Off Persiaran Olahraga, Section 13, 40100 Shah Alam, Selangor Darul Ehsan, Malaysia. E-mail : srimuralihospital2012@gmail.com
Hepatocellular carcinoma (HCC) is the most common primary malignant hepatic tumour. Hepatocellular carcinoma presenting itself or extending into the right iliac fossa (RIF) is a very rare entity. We report on a rare case of hepatocellular carcinoma in a 60-year-old lady, presented with a mobile mass in the lower abdomen without cirrhosis, with normal α-feto protein levels (AFP) or any known risk factors for liver disease. HCC in this case was unusual in its presentation both in the patient as well as a disease.
Cirrhosis, Extra hepatic growth, Malignant hepatic tumour
Case Report
A 60-year-old woman presented with 3 months history of mass in lower abdomen and occasional abdominal discomfort in the right lower flank. There was no past history of vomiting, jaundice, abdominal distension or evidence of chronic liver disease. There was no significant loss of weight or appetite. Personal history was not significant. She was a known hypertensive patient and was on regular treatment. She underwent abdominal hysterectomy 15 years back. On clinical examination she was moderately built and nourished with anaemic appearance and was not jaundiced. Her vitals were stable with non-distended abdomen. Examination of abdomen was non-tender with hepatomegaly and a separate mass of size 10x8 cm occupying the right iliac fossa (RIF) with mobility up to midline as shown in [Table/Fig-1]. It was hard in consistency and separated from liver by a groove. Dullness over the mass was continuous with the liver dullness and moved with respiration. No other masses were palpable. All other examination was normal.

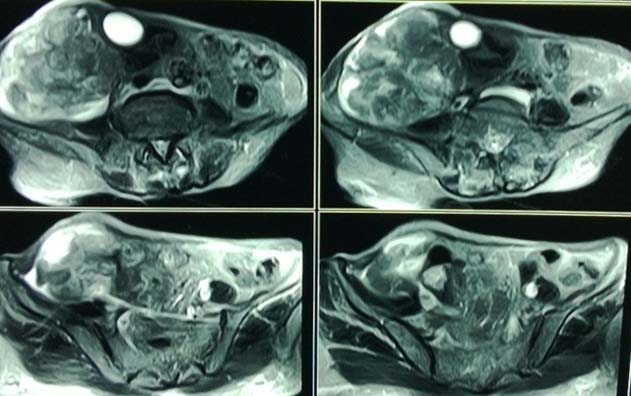
Clinical diagnosis could not be made and differential diagnosis was opted: 1) Pedunculated mass from liver; 2) Right ovarian tumour; 3) Caecal mass; or 4) Distal ileal mass. The patient was investigated with liver function test (LFT), αfeto protein (AFP), chest X-ray which but showed no positive findings. Ultrasound abdomen was done [Table/Fig-2] initially and reported inconclusively as –Metastasis within the liver with another similar lesion in right iliac fossa (RIF) showing a nodal invasion as well. As ultrasound report was inconclusive, fine needle aspiration cytology (FNAC) /core biopsy from liver and RIF mass was done which showed features of well differentiated HCC – trabecular pattern, clear cell type. She was further evaluated by Magnetic resonance imaging (MRI) of the abdomen [Table/Fig-3]. MRI scan revealed hepatomegaly with Iso to Hyperintense lesions of varying size with exophytic mass extending to right iliac fossa with minimal ascites.

With the report of core biopsy & MRI in mind and also considering the rarity of the case, to confirm the diagnosis and to know the extent of the mass the patient was subjected to diagnostic laparascopy. Laparoscopy showed multiple nodular lesions in lobes of the liver, with hard mass of size 9x7cm, arising from the right lobe of the liver and extending into right iliac fossa displacing the bowels. A small groove was noted in between the enlarged liver and RIF mass together with enlarged periportal lymph nodes. On trying to touch or move the lesion, it showed a tendency to bleed. Postoperative period was uneventful.
As the tumour was unresectable and keeping in mind the age of the patient no mutilating surgeries were advised. The patient was neither willing to undergo chemo or radiotherapy. Symptomatic treatments were given. Patient expired 3 months later.
Discussion
One of the world’s most common cancers is primary cancer of the liver (Hepatocellular carcinoma - HCC) [1]. The gross appearance of HCC had been classified into: nodular, massive or diffuse. Other classification was according to the growth pattern or spread includes expanding, spreading, multifocal or indeterminate [2]. The mechanism for its growth pattern remains unknown. Exophytic growth or pedunculation is not a rare finding of HCCs. Studies have shown that exophytic HCCs constitute 0.2 – 4.2% of all HCCs [3].
HCC is a potential complication of alcoholic cirrhosis. The many aetiologies of cirrhosis make patient prone to developing hepatocellular carcinoma. It is not necessary all patient prone to develop HCC [4]. Increasing age and male sex are independent risk factors for HCC [5]. Men have a higher prevalence of hepatocellular carcinoma than women. The ratio of affected men to affected women varies between 2:1 and 4:1, depending on the geographic region [6]. Presented is a case of an old lady without cirrhosis or any known risk factors for liver disease. This unusual presentation is a rare occurrence.
HCC has a more indolent course with more constitutional symptoms and long history of chronic liver disease. Non-cirrhotic patients with HCC typically present in a different manner [7]. Their tumours are often allowed to grow with much less restriction. Symptoms including malaise, anorexia, wasting, right upper quadrant abdominal pain and distension are often related to long-standing malignancy and tumour [7]. The clinical course of present patient also had most of the similar symptoms.
Another interesting feature in presented case was unusual presentation of HCC as a mass of size 10 x 8 cm in the right iliac fossa and mobile within the abdomen. Usually they present as an abdominal mass or hepatomegaly with hard and irregular borders that may demonstrate a vascular bruit [8]. The differential diagnosis is occasionally difficult in cases of such type of presentation of HCC extending caudally from right lobe of the liver. It is a diagnostic challenge to identify the exophytic growth of the tumour when lying beyond the confines of the liver. This is due to the uncertainty of its origin and that it mimics other abdominal tumours [9]. Two rare cases reported so far are –a case of giant pedunculated HCC combined with haemangioma, in the right iliac fossa, which presented with clinical features of intestinal obstruction by Karatzas et al., from Athens, Greece [10] and second, CT diagnosed retroperitoneal extension of HCC, thus mimicking a right adrenal tumour by Kim KW et al., from Korea [9].
Elevated serum liver enzymes levels, total bilirubin, gamma globulin, and lowered serum albumin levels are nonspecific markers of liver pathology. There is no specific pattern of LFT for diagnosing HCC [11]. The biochemical evaluation tests were within normal limits in the present case. Further on, serum alpha fetoprotein levels were also unusual in this case. A well-established tumour marker for diagnosing HCC is AFP, with sensitivity of 70-80% [12]. However, because of its less specificity, determination of the AFP level is of limited value for the diagnosis of HCC and is often elevated in chronic liver diseases, such as chronic hepatitis and liver cirrhosis [13]. Further, raised AFP levels are more suggestive of advanced stage of HCC. So, in the presented patient, normal AFP levels with such a presentation are certainly unusual.
Liver biopsy offers a safe and effective means to confirm suspicious lesions for HCC. The samples can be obtained by percutaneous fine-needle aspiration cytology (FNAC) and needle core biopsy under Ultrasound (USG) or Computerised scan (CT) guidance. Studies conducted by Sidhaling reddy et al., yielded a diagnostic value of 92.7% for USG and 100% for CT guidance [14]. Liver biopsy can be useful in the patient whose suspicious lesion does not necessarily meet the characteristic radiographic or laboratory features of HCC as in present case.
Imaging plays a key role in the diagnosis of HCC. As the extrahepatic growth, Alpha fetoprotein, Imaging of a hepatic tumour is rare, the abdominal mass between the liver, kidney and colon should be differentiated from exophytic or pedunculated hepatic tumour. The first imaging modality in many of these cases is Ultrasound as in presented case [15]. But because of the exophytic nature of the lesions, defining tissue of origin was very difficult. Multiphase contrast-enhanced MDCT or MRI is the imaging of choice in these cases [15]. The same was applicable to our case.
Laparoscopy yields additional information about extent of disease in the liver, and extrahepatic disease [4]. The yield of laparoscopy is dictated by the extent of disease and is only selectively employed as we carried out in presented case. Most of the patients diagnosed with HCC will not be amenable to surgical resection because of the advanced stage of the cancer or the severity of the underlying liver disease [1]. In the presented case even though there was no underlying liver pathology the exophytic growth was huge with multiple lesions, periportal spread and had a tendency to bleed. So surgery was deferred and moreover the patient was not willing to undergo any further treatment. Most studies show that tumour size plays a role in the prognosis and significantly affects survival [16]. In the presented case too, patient later after 3 months succumbed to death.
Conclusion
Unusual presentation of HCC is reported here. This case illustrates that HCC can present as right iliac fossa mass in an old lady with no cirrhosis, no risk factors, no viral markers and normal AFP levels. The possibility of HCC should be kept in mind in any differential diagnosis of large intraperitoneal mass even if it is not related to liver by clinical study.
[1]. Rahul S K, Sanjeev K, Brian R Davidson, The Liver. In: Williams NS, Bulstrode CJK and Ronan O’Connell P(Ed)Bailey and Love’s Short Practice of Surgery 2013 26th editionBoca Raton, LondonCRC Press:1085-86. [Google Scholar]
[2]. Zimmerman A., Tumours of the liver-pathologic aspect. In: L.H. Blumgart, Jacques Belhati, William R. Jarnagin, Ronald P. Deatteo, William C. Chapman, Markus W. Bbucheler, Lucy E Hhann, Michael Dangelica (Ed)Surgery of the liver, biliary tract, and pancreas 2007 Philadelphia, USASaunders:1085-130. [Google Scholar]
[3]. Yeh CN, Lee WC, Jeng LB, Chen MF, Pedunculated hepatocellular carcinoma: Clinicopathologic study of 18 surgically resected casesWorld J Surg 2002 26:1133-38. [Google Scholar]
[4]. Michael D’Angelica, The Liver. In: Townsend CM, Beauchamp RD, Evers BM, Mattox KL (Ed)Sabiston textbook of surgery, the biological basis of modern surgical practice: Abdomen 2008 18editionPhiladelphia, USASaunders, Elsevier:1333-47. [Google Scholar]
[5]. Zaman SN, Melia WM, Johnson RD, Portmann BC, Johnson PJ, Williams R, Risk factors in development of hepatocellular carcinoma in cirrhosis: Prospective study of 613 patientsLancet 1985 1:1357-60. [Google Scholar]
[6]. Wands J, Hepatocellular carcinoma and sexN Engl J Med 2007 357:74 [Google Scholar]
[7]. Schafer DF, Sorrell MF, Hepatocellular carcinomaLancet 1999 353:1253-57. [Google Scholar]
[8]. Di Bisceglie AM, Epidemiology and clinical presentation of hepatocellular carcinomaJ Vase Interv Radiol 2002 13(9):169-71. [Google Scholar]
[9]. Kim KW, Auh YH, Chi HS, Lee SI, CT of retroperitoneal extension of hepatoma mimicking adrenal tumourJ Comput Assist Tomogr 1993 17(4):599-02. [Google Scholar]
[10]. Karatzas T, Smirnis A, Dimitroulis D, Giant pedunculated hepatocellular carcinoma with haemangioma mimicking intestinal obstructionBMC Gastroenterology 2011 11:99 [Google Scholar]
[11]. Okonkwo UC, Nwosu MN, Nnadozie OJ, Is liver function test of any diagnostic relevance in patients presenting with hepatocellular carcinoma?Orient J Med 2011 23:1-4. [Google Scholar]
[12]. Szklaruk J, Silverman PM, Charnsangavej C, Imaging in the diagnosis, staging, treatment, and surveillance of hepatocellular carcinomaAm J Roentgenol 2003 180:441-54. [Google Scholar]
[13]. Moriwaki K, Miyoshi E, Fucosylation and gastrointestinal cancerWorld J Hepatol 2010 2:151-61. [Google Scholar]
[14]. Sidhaling R, Sainath KA, Fine needle aspiration cytology of Intra-abdominal lesionsJCDR 2011 5(3):551-58. [Google Scholar]
[15]. Kumar S, Kumar B, Sundarayan RN, Malal AM, Imaging clues for exophytic liver lesionsWest Afr J Radiol 2013 20(1):41-44. [Google Scholar]
[16]. Horie Y, Shigoku A, Tanaka H, Tomie Y, Maeda N, Hoshiro U, Prognosis for pedunculated hepatocellular carcinomaOncology 1999 57:23-28. [Google Scholar]