Extensive Giant Molluscum Contagiosum in a HIV Positive Patient
Rita V. Vora1, Abhishek P. Pilani2, Rahul Krishna Kota3
1 Professor and Head, Department of Dermatology, Shree Krishna Hospital, Pramukh Swami Medical College, Karamsad, Gujarat, India.
2 Ex-Resident, Department of Dermatology, Shree Krishna Hospital, Pramukh Swami Medical College, Karamsad, Gujarat, India.
3 Resident, Department of Dermatology, Shree Krishna Hospital, Pramukh Swami Medical College, Karamsad, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rita V. Vora, Professor and Head, Department of Dermatology, Shree Krishna Hospital, Pramukh Swami Medical College, Karamsad-388325, Gujarat, India.
E-mail: ritavv@charutarhealth.org
Molluscum contagiosum (MC) is a very common benign self-limiting cutaneous viral infection caused by molluscum contagiosum virus. Disease is self-limiting in immunocompetent individuals, while it is severe and prolonged when associated with Human Immunodeficiency Virus (HIV) infection. The widespread and refractory mollusca of HIV disease occur especially on the face. In advanced stages of immunosuppression, giant or verrucous forms of MC may occur. Molluscum contagiosum tends to take a chronic course and is usually not responsive to various treatments in immunocompromised patients. Here, we present a HIV positive male patient with extensive papulonodular lesions over face, neck, bilateral upper limbs since 2 months, diagnosed as giant molluscum contagiosum, treated with cryotherapy with little improvement for few weeks after which patient did not turn up.
Cutaneous viral infection, Immunocompromised patient, Papulonodular lesions
Case Report
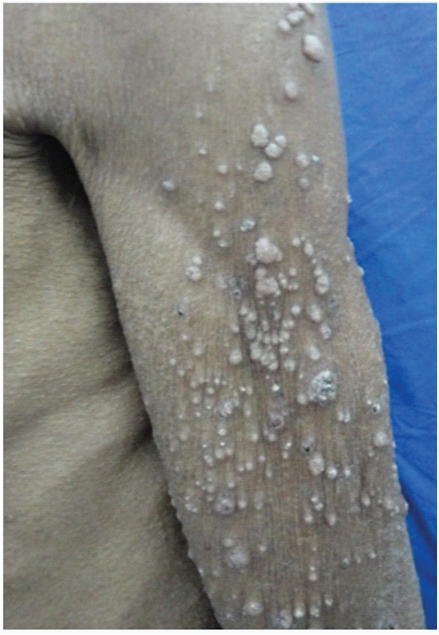
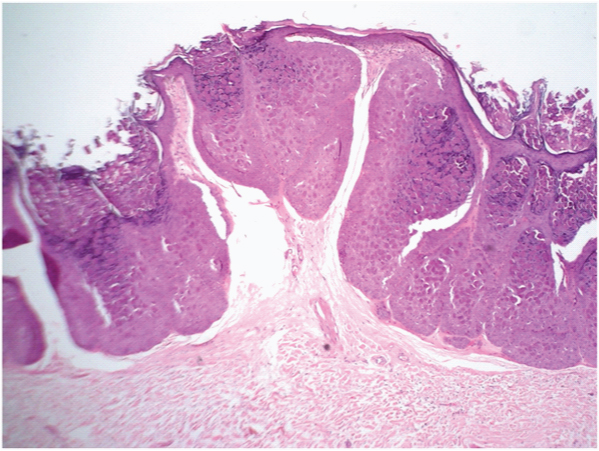
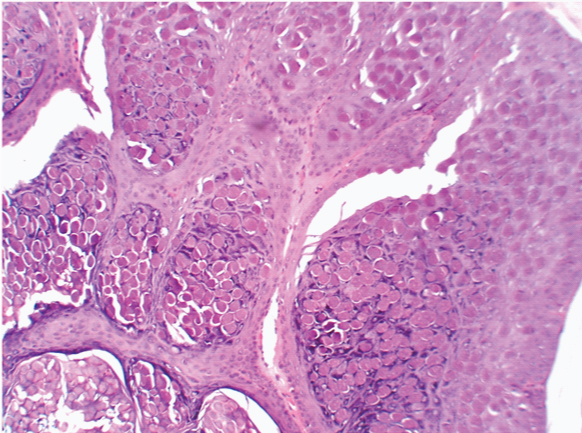
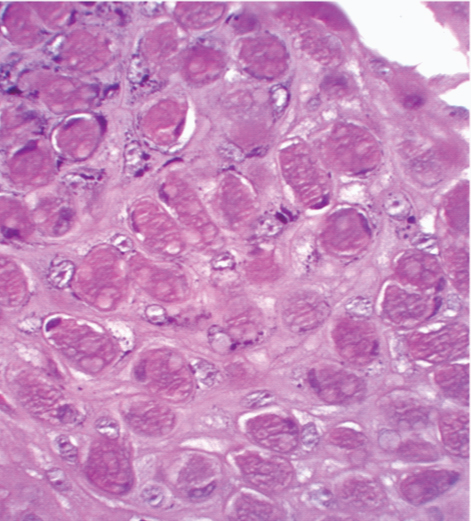
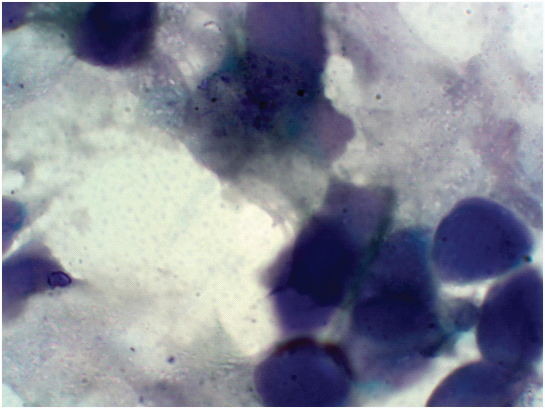
A 58-year-old, sero positive male, labourer by occupation, presented with multiple skin lesions all over body since 2 months. Patient gives history of blood transfusion thrice, 10 years back. Patient was known case of HIV since twenty four months and was on Anti Retroviral treatment (Tenofovir, Lamivudine and Efavirenz fixed dose combination) since eighteen months. There was no history of drug abuse or extramarital sexual contact. No history of any sexually transmitted disease or herpes zoster. Patient married since 35 years, his partner is also sero positive for HIV, diagnosed one year ago. On cutaneous examination, there were multiple (more than 100) shiny, non discharging, non tender, papulonodular lesions over face, neck [Table/Fig-1,2] and bilateral upper extremities [Table/Fig-3], few of them having central umbilication. Most lesions were approximately measuring about 10 to 20mm. Few lesions were below 10 mm in size. Koebnerization was present [Table/Fig-3]. There was no mucosal involvement. There were no other signs or symptoms related to AIDS (Acquired immunodeficiency syndrome). His CD4 count was 174cells/microlitre. Lymph nodes were not palpable and systemic examination was unremarkable. Routine haematological and biochemical investigations were within normal limits. Clinically differential diagnosis of cutaneous cryptococcosis, disseminated molluscum contagiosum (MC) was made. Histopathological examination revealed epithelial hyperplasia [Table/Fig-4]. Distinct large eosinophilic intracytoplasmic inclusion bodies (Henderson Peterson bodies) were seen in the squamous epithelial cells pushing the nucleus to a corner [Table/Fig-5,6]. Giemsa stain (Tzanck smear) of the lesions was done and the diagnosis of molluscum contagiosum was confirmed [Table/Fig-7]. Patient was treated with cryotherapy with little improvement for two months. After two months, he did not turn up for follow-up.
Giant molluscum over face & neck

Shiny, papulonodular lesions, few of them with central umbilication over face

Giant molluscum seen on upper extremity
Haematoxylin Eosin stain, (low power 40x) Epithelial hyperplasia with few distinct eosinophilic deposits
Haematoxylin Eosin stain, (high power 100x) squamous epithelial cells showing distinct large eosinophilic intracytoplasmic inclusions (Henderson Peterson bodies) pushing the nucleus to a corner
Haematoxylin Eosin stain, (high power 400x) Squamous epithelial cells showing distinct large eosinophilic intracytoplasmic inclusions (Henderson Peterson bodies) pushing the nucleus to a corner
Tzanck smear (Giemsa stain, 1000x, oil immersion) Squamous epithelial cells showing distinct basophilic intracytoplasmic inclusions (Henderson Peterson bodies)
Discussion
Molluscum contagiosum (MC) is a very common benign self-limiting mucocutaneous viral infection caused by molluscum contagiosum virus (MCV) belonging to the Pox virus family. Incidence peaks in pre-school children [1]. In children the infection is acquired through fomites and close contact while in adults having genital lesions, the disease is ususally sexually transmitted. Disease is self-limiting in immunocompetent individuals, while it is severe and prolonged when associated with Human Immunodeficiency Virus (HIV) infection. In the presence of HIV infection, the clinical appearance and the course of molluscum contagiosum are atypical. Upper trunk and the face are more frequently involved sites [2]. Between 10-20% of patients with symptomatic HIV disease or AIDS have molluscum contagiosum (MC) [3]. Usually the lesions of MC in HIV infected patients are multiple (up to 100 or more). In most of the patients with AIDS, MC lesion is found to be extragenital. The sites most frequently involved are the upper trunk and the face. The lesions can be present extensively over the face including eyelids [4]. Various other sites affected are neck, axillae, groin and buttocks [5]. The typical distribution indicates that the transmission of the virus by occasional contact, or through objects and fomites is more likely than sexual transmission [6]. In a cohort study conducted by Ratnam I et al., 4 of 199 HIV positive patients, developed molluscum contagiosum as immune reconstitution inflammatory syndrome (IRIS) phenomenon. Lesions of molluscum appeared a median of eight weeks after starting HAART [7]. There are case reports of IRIS presenting even as an inflamed molluscum [8].
The lesions of molluscum in patients of HIV can appear verrucous, pruritic or eczematous [9]. Lesions of molluscum can have a wide variety of presentations like comedones, abscesses, furuncles, condylomas, syringomas, keratoacanthomas, basal cell carcinomas, ecthyma, sebaceous nevus of Jadassohn, and cutaneous horn [10]. Differential diagnosis of molluscum contagiosum virus disease includes cryptococcosis, penicillinoses, histoplasmosis, pneumocystosis, pyogenic granuloma, basal cell carcinoma, kerato acanthoma, and atypical mycobacterial infections [11]. In immunosuppressed patients, the disease tends to take a chronic course and often is unresponsive to various treatments. Individual lesions of MC may be quite large with a diameter of 10 mm or more and designated as “giant molluscum contagiosum” [12]. The pathogenesis of giant lesion as well as the modified morphology of MC in HIV infected state is as yet unknown. Various factors such as decrease in number of T cells, impaired natural killer cell function, impaired blastogenic reponses to mitogens and antigens and decrease in Langerhans cells, have been thought to play a role in the pathogenesis of giant molluscum contagiosum in HIV patients [13]. The lesions are usually persistent and tend to recur after treatment. Giant molluscum contagoisum was also reported to occur in an immunocompetant patient [14], patient with idiopathic CD4 lymphocytopenia [15], a patient of chronic psoriasis on efalizumab therapy [16].
There are different treatment modalities for molluscum contagiosum which include surgical methods, cytodestructive methods. Surgical methods, such as, curettage, electrodessication, cryotherapy, and laser surgery are used. Cytodestructive methods include use of cantharadin, iodine, lactic acid, phenol, salicylic acid, silver nitrate, tretinoin, and trichloroacetic acid. Chemotherapeutic and antiviral drugs like Cidofovir, interferon and imiquimod are effective [8]. There are case reports where giant molluscum occurring in HIV patients, regressing with HAART [17], combination of HAART and topical imiquimod [18,19], paclitaxel [20].
Local destructive therapies are usually ineffective in patients with impaired immune functions with widespread and disfiguring eruptions. In these cases, Antiviral and immunomodulatory medications have been more successful in these cases [21].
Amino Levulinic Acid-Photodynamic therapy was used successfully in the treatment of recalcitrant molluscum contagiosum in an HIV individual by Gold [22]. PDT (photodynamic therapy) is a viable option for treating molluscum contagiosum in HIV-positive patients and immunocompromised children [23].
Conclusion
Any patient, thus, presenting with giant mollusca contagiosa or any atypical form of molluscum contagiosum especially of the face should be thoroughly investigated for immunosuppressive states especially HIV infection.
[1]. Dohil MA, Lin P, Lee J, Lucky AW, Paller AS, Eichenfield LF, The epidemiology of molluscum contagiosum in childrenJ Am Acad Dermatol 2006 54:47-54. [Google Scholar]
[2]. Singh VR, Singh S, Pandey SS, Numerous giant mollusca contagiosa and kaposi’s sarcomas with HIV diseaseIndian J Dermatol Venereol Leprol 1996 62:173-4. [Google Scholar]
[3]. Matis WL, Triana A, Shapira R, Eldred L, Polk BF, Hood AF, Dermatologic findings associated with human immunodeficiency virus infectionJ Am Acad Dermatol 1987 17:746-51. [Google Scholar]
[4]. Katzman M, Carey JT, Elmets CA, Jacobs GH, Lederman MM, Molluscum contagiosum and the acquired immunodeficiency syndrome: clinical and immunological details of two casesBr J Dermatol 1987 116:131-38. [Google Scholar]
[5]. Johnson A, Dover JS, Cutaneous manifestations of human immunodeficiency virus disease. In: Fitzpatric TB, Eisen AZ, Wolf K, et al, edsDermatology in general medicine 1993 New YorkMcGrow-Hill:2663 [Google Scholar]
[6]. Vozmediano JM, Manrique A, Petraglia S, Romero M, Nieto I, Giant molluscum contagiosum in AIDSInt J Dermatol 1996 35:45-47. [Google Scholar]
[7]. Ratnam I, Chiu C, Kandala NB, Incidence and risk factors for immune reconstitution inflammatory syndrome in an ethnically diverse HIV type 1-infected cohortClin Infect Dis 2006 42(3):418-27. [Google Scholar]
[8]. Lehloenya R, Meintjes G, Dermatologic manifestations of the immune reconstitution inflammatory syndromeDermatol Clin 2006 24:549-70. [Google Scholar]
[9]. Hogan MT, Cutaneous infections associated with HIV/AIDSDermatol Clin 2006 24:473-95. [Google Scholar]
[10]. Czelusta A, Yen-Moore A, Van der Straten M, Carrasco D, Tyring SK, An overview of sexually transmitted diseases: Part III, Sexually transmitted diseases in HIV infected patientsJ Am Acad Dermatol 2000 43:409-32. [Google Scholar]
[11]. Bhanumathi N, Vishwanath BK, Extensive, molluscum contagiosum in a HIV positive womanIndian J Sex Transm Dis 2008 29:89-91. [Google Scholar]
[12]. Petersen CS, Gerstoff J, Molluscum contagiosum in HIV infected patientsDermatology 1992 184:19-21. [Google Scholar]
[13]. Thappa DM, Karthikeyan K, Manjunath JV, Giant molluscum contagiosumIndian Journal of dermatology 2002 47(3):167-68. [Google Scholar]
[14]. Vardhan P, Goel S, Goyal G, Kumar N, Solitary giant molluscum contagiosum presenting as lid tumor in an immunocompetent childIndian Journal of Ophthalmology 2010 58:236-38. [Google Scholar]
[15]. Arora S, Arora G, Sahai K, Borde P, Idiopathic CD4 lymphocytopenia presenting as recurrent giant molluscum contagiosumIndian J Dermatol Venereol Leprol 2013 79:555 [Google Scholar]
[16]. Weisenseel P, Kuznetsov AV, Flaig M, Prinz JC, Disseminated Eruptive Giant Mollusca Contagiosa in an Adult Psoriasis Patient during Efalizumab TherapyDermatology 2008 217:85-86. [Google Scholar]
[17]. Sen S, Bhaumik P, Resolution of giant molluscum contagiosum with antiretroviral therapyIndian Journal of dermatology, venereology, leprology 2008 74(3):267-68. [Google Scholar]
[18]. Singhal S, Archana S, Reddy S, Murugnantham TV, Hamedullah A, A case report of molluscum contagiosum infection in an HIV infected individualInt J Med Res Health Sci 2013 2(3):712-15. [Google Scholar]
[19]. Choudhary VS, Singh A, Gupta S, Koley S, Augmented effect of five percent imiquimod cream and antiretroviral therapy in resolution of giant molluscum contagiosumIndian J Sex Transm Dis and AIDS 2008 29(2):102-04. [Google Scholar]
[20]. Sisneros SC, Recalcitrant Giant Molluscum Contagiosum in a Patient With Advanced HIV Disease — Eradication of Disease With PaclitaxelTop HIV Med 2010 18(5):169-72. [Google Scholar]
[21]. Hanson D, Diven DG, Molluscum ContagiosumDermatology Online Journal 2007 9(2):2 [Google Scholar]
[22]. Gold MH, The use of ALA-PDT in the treatment of recalcitrant molluscum contagiosum in HIV / AIDS affected individualsJ Laser Surg Med 2003 15:40 [Google Scholar]
[23]. Gold MH, Moiin A, Treatment of verrucae vulgaris and Molluscum Contagiosum with Photodynamic TherapyDermatol Clin 2007 25:75-80. [Google Scholar]