Emphysematous pyelonephritis (EPN) is one of the most common clinical form of emphysematous infections of upper urinary tract [1]. EPN is an acute, severe, necrotizing infection of the renal parenchyma and perirenal tissue, which causes gas within the renal parenchyma or in the perinephric tissue and has been associated with a high degree of morbidity and mortality [2]. Mortality rates up to 40-50% have been reported in published series [3,4]. Kelly and McCallum reported the first case of EPN in 1898 [5]. Diabetes and ureteric obstruction were the predisposing factors [6] and Escherichia coli the most common organism isolated. The modalities of treatment of EPN have evolved over the years from an aggressive surgical approach to a more conservative approach.
Herein, we present our 5 year experience of conservative management of EPN with analysis of risk factors for poor outcome.
Materials and Methods
All patients (n=8) admitted to Regional Institute of Medical Sciences (Imphal, India) and Jawaharlal Nehru Institute of Medical Sciences (Imphal, India) over the last 5 years with a diagnosis of EPN and who were treated conservatively were included for study and their case records were reviewed. Demographic factors (age, gender, background and diabetes mellitus), clinical factors on presentation and at the time of discharge (symptom, shock, azotaemia, altered sensorium, leucocytosis, Thrombocytopenia) and radiological data (initial imaging modality, CT classification) were collected for analysis. On the basis of CT scan finding, EPN was grouped into four classes based on the modified classification recommended by Huang and Tseng as follows- Class 1: gas confined to renal parenchyma; Class 2: gas extending to perinephric space and confined within the Gerota’s fascia; Class 3: gas extending beyond the Gerota’s fascia; and Class 4: gas involving both kidneys or gas in a solitary functioning kidney [7]. Azotaemia was defined as serum creatinine greater than 2.5 mg/dl. Thrombocytopenia was defined as platelet count less than 100x109/L. Hypoalbuminaemia was defined as serum albumin less than 2.5 g/dl. Shock was defined as systolic blood pressure less than 90 mm Hg. Percutaneous drainage was performed using Ultrasound guidance.
Statistical Analysis
Chi-square and Fisher’s exact tests were used to compare the categorical variables, and Mann-Whitney U-test was used to compare the continuous variables. A p-value of <0.05 was considered to indicate statistical significance, and analysis was carried out with IBM-SPSS statistics version 20.
Results
From July 2010 to June 2015 in 2 medical institutes (Regional Institute of Medical Sciences and Jawaharlal Nehru Institute of Medical Sciences) of Manipur, 8 patients were diagnosed with EPN using USG and CT. As shown in [Table/Fig-1], all the patients were diabetic (87.5%) except for one who had left lower ureteric stricture who was on steroid for nephrotic syndrome.
Demographic details of patients with EPN
| Variables | Survivors (n=5) | Nonsurvivors (n=3) | p-value |
|---|
| Age (yrs) | 46.6 ± 6.7 | 56.3 ± 8.5 | (0.12) |
| Mean duration of symptoms (days) | 4.0 ± 1.0 | 6.6 ± 1.1 | (0.017) |
| Mean duration of diabetes (yrs) | 6.5 ± 4.6 | 8.0 ± 7.0 | (0.53) |
| Sex Women | 3 | 2 | 1.0 |
| Men | 2 | 1 |
| Azotaemia | 4 | 2 | 1.0 |
| Leucocytosis | 2 | 1 | 1.0 |
| Thrombocytopenia | 0 | 3 | 0.018 |
| Shock | 0 | 3 | 0.018 |
| Altered sensorium | 0 | 3 | 0.018 |
| Conservative treatment (medical ± PCD) | 4* | 3 | 1.0 |
| Immediate Nephrectomy | 1 | 0 | 1.0 |
*One patient needed insertion of additional PCN
Their mean age was 50.25±8.46 (range 38-65) years, with male/female ratio being 3:5. The mean duration of symptoms before admission was 5.63±1.69 days, and the most common symptom was fever. Other symptoms included vomiting (25%), loin pain (75%) haematuria (12.5%) and palpable mass (25%). On presentation, three patients (37.5%) had septic shock, one of whom required immediate haemodialysis for acute kidney injury.
The right kidney was affected in 5 patients (62.5%), left in remaining 3 patients (37.5%). Pus culture in those who underwent percutaneous drainage (PCD) (7 out of 8) grew E coli in 71.4%, Klebsiella in 14.3% and Proteus in 14.3%.
Out of 8 patients, 7 underwent conservative management with antibiotics and PCD and only 1 underwent immediate nephrectomy. Four patients with conservative management deteriorated and 2 needed additional PCD and remaining 2 underwent emergency nephrectomy. Out of these 4 patients, 1 patient who underwent additional PCD insertion survived. The success rate with conservative management was 57.14 % (4 out of 7), immediate nephrectomy was 100% (1 out of 1) and that with emergency nephrectomy when conservative management failed was 0% (0 out of 2). The patient with nephrotic syndrome with left lower ureteric stricture was managed conservatively with antibiotics and PCD and completely recovered from EPN. Later, he underwent left nephrectomy as the left kidney was non-functioning. The overall survival rate was 62.5% (5 out of 8).
There was no significant difference in survival between survivors and nonsurvivors with regard to age, sex, duration of diabetes, azotaemia, leucocytosis at presentation and treatment methods given. Shock, Thrombocytopenia, altered sensorium and late presentation to the hospital were associated with poor prognosis.
[Table/Fig-2] shows the radiologic profile of 8 patients with EPN and their respective treatment. Immediate nephrectomy was performed in only one patient who had Class 3 EPN and rest of the patients (87.5%) underwent conservative management. The radiological classifications and outcomes are outlined in [Table/Fig-3].
Radiologic profile of 8 patients with EPN and their respective Treatment
| CT classification | Conservativemanagement | Immediatenephrectomy | Total, n (%) |
|---|
| Class 1 | 2 | 0 | 2 (25) |
| Class 2 | 3 | 0 | 3 (37.5) |
| Class 3 | 2 | 1 | 3 (37.5) |
| Class 4 | 0 | 0 | 0 |
Radiologic classification and their outcomes
| Category | Total | Mortality (%) |
|---|
| Class 1 | 2 | 0 (0.0) |
| Class 2 | 3 | 1 (33.3) |
| Class 3 | 3 | 2 (66.7) |
| Class 4 | 0 | 0 (0.0) |
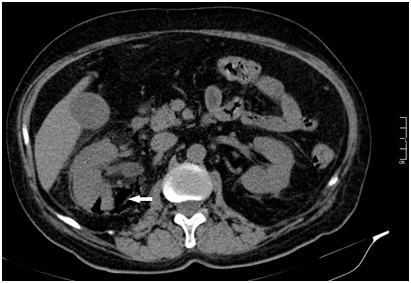
In this study, none of the patients had Class 4 EPN. The highest mortality rate of 66.7% was observed in Class 3 EPN which was followed by Class 2 [Table/Figure-4] with the mortality rate of 33.3%. All Class 1 (100%) patients survived.
Class 2 emphysematous pyelonephritis. Computed tomographic scan shows right sided EPN with extension of gas into the perinephric space (arrowhead)
Fifty seven percent of patients had at least 2 months of follow-up. One patient presented with recurrent pyelonephritis on the ipsilateral side 3 weeks after discharge from the hospital and was readmitted and managed conservatively with antibiotics.
Discussion
EPN is rare but potentially life-threatening urologic emergency. Several factors are involved in its pathogenesis which includes abnormally high glucose levels within the renal tissue, presence of gas forming organisms, impaired vascular supply, reduced host immunity and presence of urinary tract obstruction [8]. EPN is strongly associated with diabetes mellitus which is explained by high level of tissue glucose coupled with impaired tissue blood supply in diabetics.
Similar to other published articles, the majority of the patients (87.5%) in our study suffered from diabetes mellitus [7,9,10].
From the literature, there is a preponderance of EPN in females, owing presumably to their increased susceptibility to urinary tract infection [11]. The male/female ratio in our study was 3:5. In line with other series, the majority of our patients presented with fever with or without loin pain. Our patients had symptoms for 3 days or more before admission. This may explain why in 3 patients, the infective process had lapsed into septic shock.
Laboratory data in our patients conformed to those reported in the literature, with leucocytosis, Thrombocytopenia and azotaemia being the most common findings [9,11,12].
In line with other series, the most common causative pathogen in our study was E coli, followed by other gram-negative organisms [4,13].
According to the pattern of gas in CT, EPN was classified into Type I and Type II [14]. We followed the modified classification of Huang and Tseng on the basis of the extent of gas on CT [15].
In our study, serum creatinine level at presentation was not a poor prognostic factor, as reported in the literature [14].
Thrombocytopenia, shock and altered sensorium were associated with poor prognosis as reported in other articles [14,16].
Owing to the small sample size of our study, it was difficult to carry out multivariate analysis to identify the most significant risk factor. The diagnosis of EPN was made on USG except in 1 patient who had ureteric stricture. CT scan was performed in all cases to determine the extent of disease and to classify EPN. For screening of EPN, USG can be used and this can be followed up with CT scan to confirm the diagnosis and to assess the extent of gas or abscess. The successful outcome of PCD and antibiotics was 57.14% (4 out of 7), comparable to 66-92% in other series [17,18]. In our study, only one patient had immediate nephrectomy and he survived. Rescreening was done in 57.14% (4 in 7 patients) patients who were on conservative management as there was no improvement or worsening of symptoms. Out of 4 patients with progressive deterioration, 2 needed additional PCD and only one survived. Two patients underwent emergency nephrectomy and both succumbed to the disease death.
Conclusion
EPN is a serious condition with significant mortality. The prognosis of patients with EPN has changed over the years. Mortality has declined with prompt and aggressive medical management and minimally invasive strategies. Nonsurvivors tend to be those patients who seek medical treatment late. Age and sex of the patient did not affect the survival. Creatinine level and leucocytosis at initial workup did not have any impact in overall survival. Thrombocytopenia, shock and altered sensorium at presentation are the strong predictors of mortality. EPN can be successfully treated with antibiotics and percutaneous drainage. Nephrectomy can be reserved for patients who do not respond to conservative management or patients with multiple risk factors.
*One patient needed insertion of additional PCN