Sutureless and Glue-free Versus Sutures for Limbal Conjunctival Autografting in Primary Pterygium Surgery: A Prospective Comparative Study
Ashok Sharma1, Hans Raj2, Aditi Gupta3, Amit Vikram Raina4
1 Associate Professor, Department of Ophthalmology, Government Medical College, Jammu, Jammu and Kashmir, India.
2 Assistant Professor, Department of Ophthalmology, Government Medical College, Jammu, Jammu and Kashmir, India.
3 Resident, Department of Ophthalmology, Government Medical College, Jammu, Jammu and Kashmir, India.
4 Resident, Department of Ophthalmology, Government Medical College, Jammu, Jammu and Kashmir, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ashok Sharma, 67/1, Channi Himmat, Jammu, Jammu and Kashmir – 180015, India.
E-mail: ashoaksharma@yahoo.co.in
Introduction
Sutureless and glue-free conjunctival autograft as a treatment modality for primary pterygium is recently gaining popularity but conventional technique of suturing conjunctival autograft is still practised widely.
Aim
To compare the outcome of sutureless and glue-free technique with sutures for limbal conjunctival autografting in management of primary pterygium.
Materials and Methods
A prospective interventional study was carried out in 50 consecutive eyes with primary nasal pterygium requiring surgical excision. Simple excision under local anaesthesia was performed followed by closure of the bare sclera by sutureless and glue-free conjunctival autograft in 25 eyes of 25 patients (group 1) and by the conventional method of suturing conjunctival autograft using interrupted 10-0 nylon sutures in 25 eyes of 25 patients (group 2), followed by bandaging for 24 hours in both the groups. Surgical time was recorded for both the techniques. Postoperative discomfort was assessed using preformed questionnaires. The patients were followed up for 6 months. During follow up, graft related complications and recurrence if any were noted.
Results
Mean surgical time for group 1 (23.20±1.55 minutes) was significantly less as compared to group 2 (37.76±1.89 minutes); (p=0.001). Postoperative symptoms were seen in less number of patients (20%) and were of shorter duration (2 weeks) in group 1 as compared to group 2 with 20 (80%) patients having symptoms lasting for 4 weeks; (p<0.001). Recurrence rate and conjunctival granuloma formation rate for group 1 (0%) and for group 2 (4%) were statistically insignificant.
Conclusion
Sutureless and glue-free conjunctival autograft technique is simple, easy, safe, effective and less time consuming than sutured limbal autograft technique with less postoperative discomfort and adverse events encountered with the use of suture material. Postoperative results of both techniques are comparable. Hence sutureless and glue-free conjunctival autografting is a good technique for the treatment of primary pterygium.
Conjunctival degeneration, Fibrin glue, Glue-free conjunctival autograft, Limbal stem cells
Introduction
Pterygium is defined as a degenerative ocular surface disorder with wing-shaped fibrovascular growth of the subconjunctival tissue onto the cornea. The epithelium may be normal, thick, or thin, but it may occasionally show dysplasia [1]. Localized limbal stem cell deficiency is thought as a causative factor for pterygium formation [2].
A small pterygium causes only slight irritation, cosmetic blemish, and slight heaviness or redness in the eyes but if gets advanced it can cause impairment of vision. Once it invades the cornea, it causes corneal opacity [3].
A number of surgical techniques have been described as methods for management of pterygium, including bare sclera resection [4], bare sclera resection followed by mitomycin C application at different point of time, doses, and concentrations [5,6], and pterygium excision plus conjunctival autografting or amniotic membrane placement [6]. Conjunctival autografting has also been advocated for the management of recurrent pterygium [7]. Limbal conjunctival autograft is currently the most popular surgical procedure [8]. Glue is widely used due to many advantages like easy fixation of the graft, shorter operation time, reduction in complications and postoperative discomfort but at the same time has some disadvantages also like high cost, the risk of transmission of infections and inactivation by iodine preparations [9–11].
The most common method of autograft fixation is suturing. But it has its own drawbacks like increased operating time, postoperative discomfort, inflammation, buttonholes, necrosis, giant papillary conjunctivitis, scarring and granuloma formation [12].
Sutureless and glue-free conjunctival autograft is a new, easy and cheaper technique for the management of pterygium [8,13].
The available literature comparing sutureless and glue-free conjunctival autograft with sutured conjunctival autograft is scanty. Further in view of problems encountered with the sutured graft and the trend towards increasing use of sutureless and glue-free grafting for pterygium surgery, a comparative study can throw light on the two techniques simultaneously comparing their merits and demerits, hence the current study was undertaken.
Materials and Methods
In this study, autologous limbal conjunctival grafting was done without sutures and glue, and the results were compared with those obtained with sutured autografts. Our objective was to lessen patient discomfort by using sutureless and glue-free technique rather than sutures when securing the graft.
This prospective interventional case study included consecutive 50 eyes with primary nasal pterygium requiring surgical excision. Patients were randomised using random table number method and two groups were formed with 25 eyes in each group.
a) Sutureless and glue-free technique - Group 1
b) Interrupted 10-0 nylon sutures – Group 2
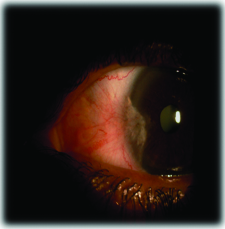
Inclusion criteria: Patients of all ages and of either sex presenting with primary nasal pterygium [Table/Fig-1]. Temporal pterygium was not included as it is very rare.
Exclusion criteria: Recurrent pterygium, glaucoma, retinal pathology requiring surgical intervention, history of previous ocular surgery or trauma.
Preoperative ophthalmic evaluation: Uncorrected and best corrected visual acuity, digital anterior segment photography, slit-lamp examination, and fundoscopy.
Surgical technique
Peribulbar anaesthesia with 2% lignocaine and 0.5% bupivacaine in 1:1 ratio was given preoperatively. The body of the pterygium was dissected 4 mm from the limbus, down to the bare sclera. Pterygium was removed from the cornea by avulsion. Only the thickened portion of conjunctiva and the immediate adjacent and subjacent Tenon’s capsule showing tortuous vasculature were excised. Large haemorrhages were tamponade with direct compression. Cautery was avoided. Oversized graft by 1mm was used after measuring with the Castroviejo-caliper. The graft was taken from superior 12 o’clock position. The graft was resected with the help of conjunctival scissors. No fluid or air was used for making the graft. Care was taken to include as little as possible of Tenon’s tissue in the graft. In group 1, the graft was placed on bare sclera and positioned so as to maintain the limbus-limbus orientation. The graft was kept apposed to the scleral bed for 10 minutes by applying gentle pressure with fine non-toothed forceps. During small bleed in the scleral bed, there is always a small ooze of the serum which acts as adhesive. Large bleed lifts the graft from scleral bed with subsequent complications, and should be tamponade before placing the graft.
In group 2, the corners of the graft were anchored with episcleral bites to maintain the position of the graft with interrupted 10-0 nylon sutures. In both the groups, the eye was bandaged for 24 hours. Topical antibiotic-steroid eye drops along with topical lubricants were given. Sutures were removed 2 weeks later.
The groups were compared with regards to the surgical time. Total surgical time was from first conjunctival cut to removal of lid speculum i.e. the time taken from the excision of pterygium to the time to secure the graft on the bed. Postoperative symptoms such as pain, foreign body sensation, watering, redness, photophobia etc., and complications were documented. Recurrence was defined as conjunctival growth extending greater than 1mm over the corneal surface.
Results
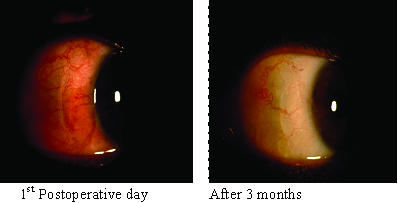
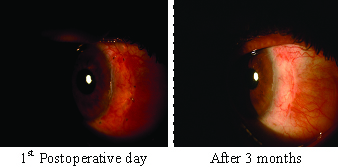
A total of 50 eyes of 50 patients were studied. Patients were divided into 2 groups; group 1 consisted of patients who underwent sutureless and glue-free limbal conjunctival autografting and group 2 comprised of patients who underwent suturing for limbal conjunctival autografting. The demographic profile of the patients is summarized in [Table/Fig-2]. Patients were followed up postoperatively on 2nd day, 1 week, 2 weeks, 4 weeks, 3 months and 6 months. [Table/Fig-3 & 4] show postoperative clinical photographs on day-1 and at 3 months. Both the groups were compared [Table/Fig-5]. The average surgical time for group 1 was 23.20±1.55 minutes and for group 2 was 37.76±1.89 minutes (p-value = 0.001). Postoperative symptoms were seen in 5 (20%) patients in group 1 and 20 (80%) patients in group 2 (p-value <0.002). The severity of symptoms was maximum on 1st Postoperative day for both the groups;the duration for which symptoms lasted was 2 weeks for group 1 and 4 weeks for group 2 (p-value < 0.001). Graft oedema was seen in 2 (8%) eyes in group 1 and 3 (12%) eyes in group 2 which resolved after 1 week. One patient (4%) had conjunctival granuloma and 1-patient (4%) had recurrence in group 2 (statistically insignificant). Graft anchoring related complications like retraction, graft displacement, wrinkling, loss, and shrinkage were not observed in the current study.
Demographic Profile of the Study Population
| Demographic Data | Group 1 (n=25) | Group 2 (n=25) |
|---|
| Range of age in (years)Mean age in (years) | 25-7542.65 ± 15.34 | 25-7543.77 ± 16.81 |
| SexMalesFemales | 1213 | 1312 |
| LateralityRightLeft | 1114 | 1213 |
| Site of pterygium | Nasal (100 %) | Nasal (100 %) |
Sutureless and Glue-free Flap
Comparison between Two Groups.
| Group 1 | Group 2 | p-value |
|---|
| Average Surgical Time (In Minutes) | 23.20 ± 1.55 | 37.76 ± 1.89 | = 0.001 |
| Complications Rate | | | |
| Postoperative symptoms | 5 (20%) | 20 (80%) | <0.002 |
| Duration of symptoms (in wks.) | 2 | 4 | <0.001 |
| Graft oedema | 2 (8%) | 3 (12%) | NS |
| Conjunctival granuloma | 0 (0%) | 1 (4%) | NS |
| Recurrence rate | 0 (0%) | 1 (4%) | NS |
Discussion
While performing surgery the surgeon should keep in mind the possibility of more aggressive recurrent pterygium, so that the operative procedure chosen should be such that it minimizes recurrence. Hence, the aim of pterygium surgery should not only be excision of pterygium but also prevention of its recurrence. Generally, the pterygium recurrences occur within the first 6 months after surgery [14]. One such method to prevent recurrence is autologous limbal conjunctival grafting. Limbal conjunctival autograft transplantation re-establishes the barrier function of limbus and hence significantly lowers the recurrence rate. It is either attached with sutures, or with biological adhesive like fibrin glue, which is derived from pooled human plasma, or with autologous fibrin. Suturing of the autograft is rather difficult and necessitates surgical experience and technical skills. Suzuki et al., reported that use of silk or nylon suture causes conjunctival inflammation and Langerhan’s cell migration into the cornea [15]. Increased operation time required for suturing is another problem for many surgeons [16]. In addition, sutures may cause patient discomfort, dellen formation, symblepharon or graft rupture [17,18].
Another alternative is to use biological tissue glue, like fibrin glue, for securing the graft. Advantages of using it are easy fixation of the graft, shorter operation time and reduction in complications and postoperative discomfort. But certain disadvantages are also associated with its use like high cost. Koranyi et al., reported the cost of 0.5ml of fibrin glue equal to the price of five 7/0 vicryl sutures [9]. Moreover, the risk of transmission of infections is there with its use. Virus removal and inactivation procedures that are used in its manufacturing process are of limited value against non-enveloped viruses such as hepatitis A virus and Parvovirus B19 [16]. Also, it is seen that fibrinogen compounds are susceptible to inactivation by iodine preparations like those used for conjunctival disinfection before pterygium surgery [17]. Apart from these options, there are studies which have shown successful outcome with sutureless and glue-free conjunctival autograft [8,10].
We compared the two techniques i.e. sutureless and glue-free conjunctival limbal autograft (group 1) and the sutured conjunctival limbal autograft (group 2) for primary pterygium surgery in our study.
In our study, the average surgical time was 23.20±1.55 minutes for group 1 and 37.76±1.89 minutes for group 2. It was comparable to mean operative time seen in study conducted by Elwan, in which sutureless and glue-free conjunctival limbal autografting took 24 (±5.64) minutes and suturing of conjunctival limbal autograft took 28.64 (±6.45) minutes [18]. The study was also comparable with other studies in terms of operating time for sutured autograft [19–21] and sutureless and glue-free conjunctival limbal autograft [10,22–24].
Postoperative symptoms like pain, watering and redness were seen in 5 (20%) patients in group 1 and in 20 (80%) patients in group 2. The symptoms were maximum on day 1 and then gradually disappeared within 2 weeks in group 1 and within 4 weeks in group 2. The results were similar to study conducted by Elwan on similar 2 groups where he concluded that postoperative signs and symptoms like pain, foreign body sensation, photophobia, hyperaemia and chemosis were significantly lower in the first postoperative month as well as significantly higher overall patient satisfaction in sutureless compared to sutured autograft [18]. Postoperative symptoms were also reported more with sutures and less with sutureless autograft by various authors [8,13,19–26]. Kim et al., reported that patient symptoms disappeared in 23 out of 36 eyes (64%) in one week and all the symptoms gone within two weeks after surgery in all patients [27].
Complications like graft oedema was seen in 2 (8%) patients in group 1 and 3 (12%) patients in group 2. Conjunctival granuloma and recurrence were not seen in case of group 1, although group 2 reported 1 (4%) case each of granuloma and recurrence after follow up of 6 months which were statistically insignificant. A similar study by Elwan showed conjunctival oedema in 8 patients (16%) and 6 patients (6%), recurrence in 3 patients (6%) and 8 patients (8%) and granuloma formation in 0 (0%) and 3 patients (3%) for sutureless and glue-free (group 1) and sutured (group 2) limbal conjunctival autograft respectively. The patients were followed for a period of 2 years. All cases of recurrence in group 1 occurred after 3 months and in group 2 after 6 months [18]. Malik et al., reported recurrence in 1 eye (2.5%) and no granuloma formation at 6 months in case of sutureless and glue-free autograft [8]. As per Hall et al., there was no recurrence at the end of 3 months in the glue group and 2 recurrences in the suture group [28]. Foroutan et al., observed a recurrence rate of 13.33% in three years follow up with autologous fibrin [10]. Wit et al., reported no recurrence in 15 eyes within a mean follow up period of 9.2 months. The reason being, apposition of the lids to the bulbar conjunctiva provides a natural biological dressing which allows a unique wound healing environment. Also, the use of sutureless and glue-free grafting technique results in an even tension across the whole of the graft interface, and no direct tension on the free graft edges resulting in reduced stimulus for the formation of subconjunctival scar. For a successful graft take up, a thin graft with meticulous dissection from the Tenon’s capsule is required [13].
Conclusion
Sutureless and glue-free limbal conjunctival autografting is a new novel technique for the treatment of primary pterygium. Not only the surgcal time required is less but also the complications encountered are fewer than suturing technique. Moreover, the feasibility and absence of cost factor, tedious suturing process and potential adverse reactions encountered with the use of foreign material make it superior to suturing. More research with longer follow up is required to add to the knowledge about both the techniques.
[1]. Hill JC, Maske R, Pathogenesis of pterygiumEye 1989 3:218-26. [Google Scholar]
[2]. Tseng SCG, Concept and application of limbal stem cellsEye 1989 3:141-57. [Google Scholar]
[3]. Oldenburg JB, Garbus J, McDonnell JM, McDonnell PJ, Conjunctival pterygia: Mechanism of corneal topographic changesCornea 1990 9:200-04. [Google Scholar]
[4]. D’Ombrain A, The surgical treatment of pterygiumBr J Ophthalmol 1948 32:65-71. [Google Scholar]
[5]. Kunitomo N, Mori S, Studies on the pterygium: A treatment of the pterygium by mitomycin C instillationActa Soc Ophthalmol Jpn 1963 67:601-07. [Google Scholar]
[6]. Mahar PS, Nwokora GE, Role of mitomycin C in pterygium surgeryBr J Ophthalmol 1993 77:433-35. [Google Scholar]
[7]. Kenyon KR, Wagoner MD, Hettinger ME, Conjunctival autograft transplantation for advanced and recurrent pterygiumOphthalmology 1985 92:1461-70. [Google Scholar]
[8]. Malik KP, Goel R, Gutpa A, Gupta SK, Kamal S, Mallik VK, Efficacy of sutureless and glue-free limbal conjunctival autograft for primary pterygium surgeryNepal J Ophthalmol 2012 4:230-35. [Google Scholar]
[9]. Koranyi G, Seregard S, Kopp ED, Cut and paste: A no suture, small incision approach to pterygium surgeryBr J Ophthalmol 2004 88:911-14. [Google Scholar]
[10]. Foroutan A, Beigzadeh F, Ghaempanah MJ, Eshghi P, Amirizadeh N, Sianati H, Efficacy of autologous fibrin glue for primary pterygium surgery with conjunctival autograftIranian Journal of Ophthalmology 2011 23:39-47. [Google Scholar]
[11]. Gilmore OJ, Reid C, Prevention of intraperitoneal adhesions: A comparison of noxythiolin and a new povidone iodine/PVP solutionBr J Surg 1979 66:197-99. [Google Scholar]
[12]. Starck T, Kenyon KR, Serrano F, Conjunctival autograft for primary and recurrent pterygia: Surgical technique and problem managementCornea 1991 10:196-202. [Google Scholar]
[13]. Wit D, Athanasiadis I, Sharma A, Moore J, Sutureless and glue-free conjunctival autograft in pterygium surgery: A case seriesEye 2010 24:1474-77. [Google Scholar]
[14]. Adamis AP, Starck T, Kenyon KR, The management of pterygiumOphthalmol Clin North Am 1990 3:611-23. [Google Scholar]
[15]. Suzuki T, Sano Y, Kinoshita S, Conjunctival inflammation induces Langerhans’ cell migration into the corneaCurr Eye Res 2000 21:550-53. [Google Scholar]
[16]. Ti SE, Chee SP, Dear KB, Tan DT, Analysis of variation in success rates in conjunctival autografting for primary and recurrent pterygiumBr J Ophthalmol 2000 84:385-89. [Google Scholar]
[17]. Kim HH, Mun JH, Park YJ, Lee KW, Shin PJ, Conjunctivolimbal autograft using a fibrin adhesive in pterygium surgeryKorean J Ophthalmol 2008 22:147-54. [Google Scholar]
[18]. Elwan SAM, Comparison between sutureless and glue-free versus sutured limbal conjunctival autograft in primary pterygium surgerySaudi Journal of Ophthalmology 2014 28:292-98. [Google Scholar]
[19]. Yuksel B, Unsal SK, Onat S, Comparison of fibrin glue and suture technique in pterygium surgery performed with limbal autograftInt J Ophthalmol 2010 3:316-20. [Google Scholar]
[20]. Goswami S, Chatterjee SS, Goswami S, Bhaduri G, A comparative study of use of fibrin glue and vicryl suture in conjunctival autograft transplantation following pterygium excisionIndian Journal of Basic and Applied Medical Research 2014 4:169-75. [Google Scholar]
[21]. Cha DM, Kim KH, Choi HJ, Kim MK, Wee WR, A comparative study of the effect of fibrin glue versus sutures on clinical outcome in patients undergoing pterygium excision and conjunctival autograftsKorean J Ophthalmol 2012 26:407-13. [Google Scholar]
[22]. Kulthe SB, Bhosale AP, Patil PU, Pandve HT, Is the surgical technique of a sutureless and glue-free conjunctivo limbal autograft after pterygium excision complications free?Medical Journal of Dr. D.Y. Patil University 2015 8:308-12. [Google Scholar]
[23]. Rangu RV, Wanjari A, Akhade N, Study of sutureless and glue-free conjunctiv alautograftInternational Journal of Recent Trends in Science And Technology 2014 10:480-82. [Google Scholar]
[24]. Majumder CH, A prospective study on “pterygium excision and conjunctival autograft-without suture, without glue”J Clin Exp Ophthalmol 2014 5:146 [Google Scholar]
[25]. Nishant K, Prasad V, Shahnawaz A, Akbar MA, Comparison of ‘cut and paste (using fibrin glue)’ Vs ‘cut and suture (using 8-0 vicryl sutures)’ techniques of pterygium surgeryInt J Cur Res Rev 2014 6:64-76. [Google Scholar]
[26]. Karalezli A, Kucukerdonmez C, Akova YA, Altan-Yaycioglu R, Borazan M, Fibrin glue versus sutures for conjunctival autografting in pterygium surgery: A prospective comparative studyBr J Ophthalmology 2008 92:1206-10. [Google Scholar]
[27]. Kim HH, Mun HJ, Park YJ, Lee KW, Shin JP, Conjunctivolimbal autograft using a fibrin adhesive in pterygium surgeryKorean J Ophthalmol 2008 22:147-54. [Google Scholar]
[28]. Hall RC, Logan AJ, Wells AP, Comparison of fibrin glue with sutures for pterygium excision surgery with conjunctival autograftsClin Experiment Ophthalmol 2009 37:584-89. [Google Scholar]