Bilateral Calcifying Cystic Odontogenic Tumour of Mandible: A Rare Case Report and Review of Literature
Pragun Khandelwal1, Amita Aditya2, Amit Mhapuskar3
1 Post Graduate Student, Department of Oral Medicine and Radiology, Sinhgad Dental College and Hospital, Pune, India.
2 Reader, Department of Oral Medicine and Radiology, Sinhgad Dental College and Hospital, Pune, India.
3 Professor and Head, Department of Oral Medicine & Radiology, Sinhgad Dental College and Hospital, Pune, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Amita Aditya, Reader, Department of Oral Medicine and Radiology, Sinhgad Dental College and Hospital, Vagabond (Bk), Off Sinhgad Road, Pune-411041, India.
E-mail: dr.amita30@rediffmail.com
Calcifying cystic odontogenic tumour (CCOT) is a relatively rare lesion of oral and maxillofacial region and forms only 2% of all odontogenic tumours. It was previously known as Calcifying odontogenic cyst and only recently has been classified as a tumour by WHO. The controversy regarding its origin can be owed to its diverse clinical and histopathological presentation and variation in reported malignant potential. It was first reported by Gorlin in 1962 and since then conundrum regarding its true nature has persisted. It is seen in association with other lesions like odontoma, ameloblastoma and ameloblastic fibroma. Both intra-osseous and extra-osseous forms of CCOT have been reported. It commnoly occurs in anterior region with equal preponderance in maxilla and mandible.
Here we present a rare case of bilateral CCOT in the posterior mandible of a 16-year-old male patient which was discovered incidentally during a radiographic examination.
CBCT, Incidental finding, Oral and maxillofacial region
Case Report
A 16-year-old patient reported to the Department of Oral Medicine & Radiology with the chief complaint of pain on right and left mandibular posterior region since 2 years. The pain was dull, intermittent and localized in nature. History of presenting illness also revealed that the pain typically occurred on visualization of food, persisted for initial 4-5 bites and then relieved on its own. Patient’s medical and dental history was non-contributory.
General physical and extra-oral examination of the patient did not reveal any abnormality. Intra-oral examination also did not reveal any significant finding, except for missing lower right second molar. History of chronic pain since two years in the absence of any significant clinical finding posed a diagnostic dilemma for us. However, considering the patient’s chief complaint of pain on seeing and having food; probability of salivary gland pathology like sialolithiasis could not completely be ruled out, despite of no abnormality detected on palpation of the submandibular salivary glands.
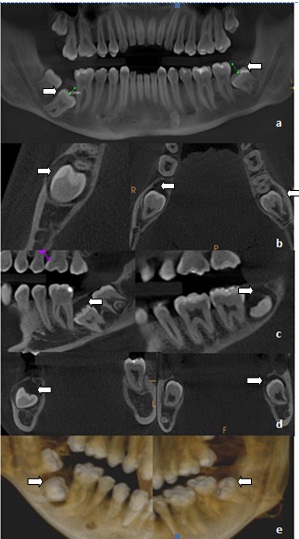
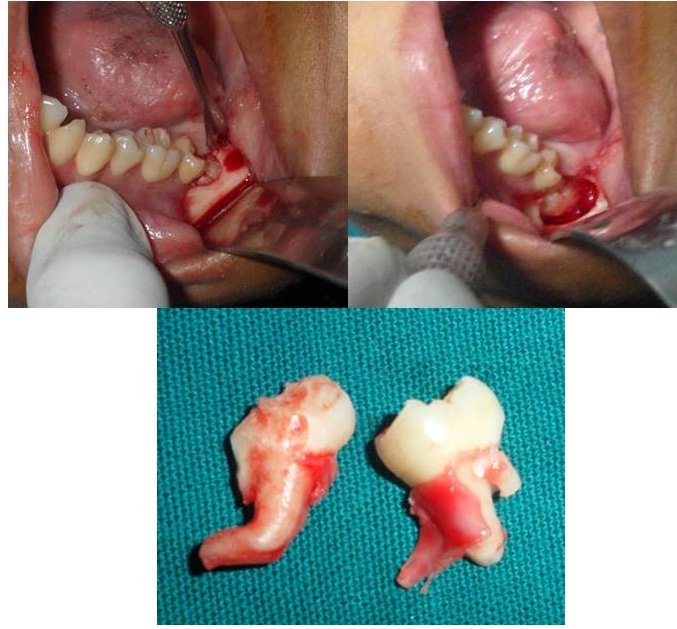
To get a clearer overview of the scenario and to rule out any other pathology, radiographic investigations were carried out, which included intraoral periapical radiograph of right and left mandibular posterior region, mandibular cross sectional occlusal [Table/Fig-1ab and c], Panoramic radiograph and PA mandible (blown mouth). The radiographs did not reveal any abnormality other than an incidental finding of well-defined and corticated radiolucency associated pericoronally with impacted lower right and left third molar. For further analysis of the radiolucencies, Cone Beam Computed Tomography (CBCT) was done. It revealed expansion and thinning of buccal cortical plate and expansion of lingual cortical plate in all the sections, a finding that was not appreciable on clinical examination [Table/Fig-2]. Radiographic features of the lesion indicated pericoronal cystic lesion associated with 38, 47 and 48. A radiographic differential diagnosis of dentigerous cyst and unicystic ameloblatoma was thought of.
Impacted 38 with multiple radio-opacities involving enamel of 36 and 37 suggestive of restorative material

Impacted 47 and 48 with well-defined and corticated radiolucency associated pericoronally

Cross-sectional mandibular occlusal showing cortical expansion

CBCT images (a) Reconstructed Panoramic, (b) Axial Section, (c) Sagittal Section, (d) Coronal Section, (e) Reconstructed 3D image showing expansion and thinning of buccal cortical plate and expansion of lingual cortical plate in all the sections
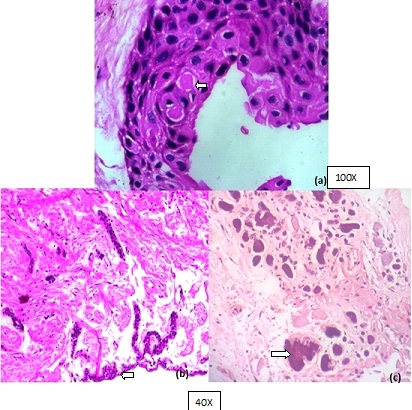
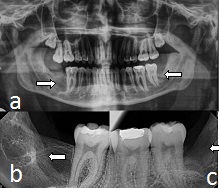
After obtaining due consent from the patient and carrying out routine haematological investigations, enucleation of the lesion along with the surgical removal of 38, 47 and 48 was done [Table/Fig-3]. Histopathological examination of the specimen revealed polyhedral cells with darkly standard eosinophilic cytoplasm resembling odontogenic epithelium with dystrophic calcification in the form of irregular basophilic calcifying structure. Some of the cells in the epithelium had undergone eosinophilic condensation resembling ghost cells [Table/Fig-4a-c]. Considering the history, clinical examination, investigations and characteristic histopathological findings, a final diagnosis of bilateral CCOT was made. Till the time of reporting, no recurrence was reported in our patient [Table/Fig-5].
Intraoperative photographs of the patient
Histopathological examination showing (a) Eosinophilic condensation shown by some cells, resembling ghost (b) Polyhedral cell with darkly stained eosinophilic cytoplasm resembling odontogenic epithelium. (c) Dystrophic calcification in form of irregular basophilic calcifying structure
Postoperative radiographs showing no recurrences
Discussion
Calcifying Cystic Odontogenic Tumour (CCOT) is a rare benign odontogenic tumour with persisting conundrum regarding its origin and malignant potential. Its clinical and radiographic features are not considered pathognomonic, and it is characterized by its histopathologic features [1].
CCOT is generally asymptomatic in nature. Radiographic features include generally unilocular, and rarely multilocular radiolucency with probability of calcified radiopacities within it. Since its recognition and description by Gorlin et al., the variable histology and clinical behaviour of CCOT has been an issue of much debate. According to updatation of the classification of odontogenic tumour by WHO, CCOT which was previously known as Calcifying Odontogenic Cyst (COC); is now widely considered as a neoplastic lesion [2].
CCOT is a rare tumour, and represents 2% of all odontogenic pathologic changes of jaw [3]. Around 65% of the CCOT are reported to occur in the anterior jaw [4].
This report presents an extremely rare case of bilateral mandibular CCOT in a 16-year-old patient, which was discovered incidentally during radiographic examination.
CCOT earlier termed as COC; was initially described as an oral variant of ‘calcifying epithelioma of Malherbe’ by Gorlin et al., [5]. A classification was proposed by Pretorius which categorized COCs into cystic and neoplastic variants [Table/Fig-6] [6]. It was later classified by WHO as an odontogenic tumour.
Classification of the so called COC by Praetorius et al., (1981) [6]
| Type 1: Cystic type |
| 1. Simple Unicystic type |
| 2. Odontomas producing type |
| 3. Ameloblastomatous proliferating type |
| Type 2 : Neoplastic type |
| 1. Dentinogenic ghost cell tumour |
CCOT represents 5-7% of the entire intraosseous odontogenic tumour, with equal predilection for maxilla and mandible. It generally occurs unilaterally in the 2nd to 3rd decade of life with no gender predilection. Around 65-67% of the cases of COC have been reported in the anterior region of the jaw [7]. As far as its presence in posterior region of jaw is concerned, few cases have been reported in maxillary posterior region [8]. In the present case, there was bilateral occurrence of CCOT in the mandibular posterior region, making it a rare presentation. CCOT are generally asymptomatic and hence discovered incidentally. However in the present case, patient complains of pain bilaterally. To the best of our knowledge, ours is the first reported case of bilateral CCOT.
Radiographically, CCOT appears as a unilocular or multilocular lesion with well defined margins. Calcifications are present in nearly one third to half of the cases. In 20% of the cases, CCOT are associated with odontome and ameloblastoma [7]. Most of the CCOT are between 2 cm to 4 cm in the greatest diameter, but can be as large as 12 cm. Root resorption can also be seen [1]. In the present case, radiographic images, CBCT in particular; were instrumental in diagnosing and localizing the lesions as the clinical features were invariably insignificant. This emphasizes the significance of imaging modalities in answering the diagnostic dilemmas as in the present case.
Histopathologically, the cystic lining in CCOT shows proliferation to the point that resembles ameloblastoma. Within this proliferation the epithelial cell undergoes characteristic ‘ghost cell’ keratinization. Ghost cell contains nuclear remnants, remnants of cytoplasmic organelles and numerous to no filaments [6]. Calcifications within the ghost cell are common. They first appear as fine basophilic granules that may increase in size and number to form extensive masses of calcified material [1]. In our cases similar histopathologic features were found from the samples collected bilaterally.
The intraosseous CCOT is treated mostly by enucleation. Recurrences have been reported, warranting more radical approach in certain cases. Some authors have reported incidences of malignant transformation in recurrent cases of CCOT. A case of CCOT of maxilla was reported by Li and Gao, which showed malignant transformation to Giant cell odontogenic carcinoma after multiple recurrences [9]. Hence, a long term follow up of such patients must be done.
Conclusion
Although CCOT is a rare lesion, it must be considered in the differential diagnosis of oral and maxilla-facial neoplasms. Considering its varied clinical and histopathological presentation, it may pose a diagnostic challenge to the clinicians. Hence, the clinicians must be cognizant of the features of this uncommon entity.
[1]. Charles A, Odontogenic cyst and tumours. In: Neville BW, Damm DD, Allen CM, Bouquot JEOral and maxillofacial pathology 2005 2nd edSt. LouisSaunders:589-642. [Google Scholar]
[2]. Sidana S, Poonja K, Galinde J, Poonja LS, Calcifying Cystic Odontogenic Tumour with Compound OdontomaJ Contemp Dent Pract 2013 3(1):36-9. [Google Scholar]
[3]. Knezevic G, Sokler K, Kobler P, Manojlovic S, Calcifying Odontogenic Cyst – Gorlin’s Cyst – Report of two casesColl. Antropol 2004 28(1):357-62. [Google Scholar]
[4]. Li TJ, Yu SF, Clinicopathologic spectrum of the so-called calcifying odontogenic cysts: a study of 21 intraosseous cases with reconsideration of the terminology and classificationAm J Surg Pathol 2003 27(3):372-84. [Google Scholar]
[5]. Rajendran R, Cyst and Tumours of Odontogenic Origin. In : Rajendran R, SivapathasundharamShafer’s textbook of Oral Pathology 2006 5th edElsevier:357-434. [Google Scholar]
[6]. Sonawane K, Singaraju M, Gupta I, Singaraju S, Histopathologic Diversity of Gorlin’s Cyst: A Study of Four Cases and Review of LiteratureJ Contemp Dent Pract 2011 12(5):392-7. [Google Scholar]
[7]. Zornosa X, Muller S, Calcifying Cystic Odontogenic TumourHead and Neck Pathol 2010 4(4):292-4. [Google Scholar]
[8]. Chindasombatjaroen J, Poomsawat S, Boonsiriseth K, Two unique cases of calcifying cystic odontogenic tumour in the maxillary posterior regionOral Surg Oral Med Oral Pathol Oral Radiol 2014 118(4):497-504. [Google Scholar]
[9]. Li BB, Gao Y, Ghost cell odontogenic carcinoma transformed from a dentinogenic ghost cell tumour of maxilla after multiple recurrenceOral Surg Oral Med Oral Pathol Oral Radiol 2009 107(5):691-95. [Google Scholar]