Colon-Cut-off-Sign in the CT-Scanogram – Evidence of Pancreatitis?
Anna Schrum1, Fabian Scheer2, Reimer Andresen3
1 Medical Assistant, Institute of Diagnostic and Interventional Radiology/Neuroradiology, Westküstenklinikum Heide, Academic Teaching Hospital of the Universities of Kiel, Lübeck and Hamburg, Germany.
2 Medical Specialist, Institute of Diagnostic and Interventional Radiology/Neuroradiology, Westküstenklinikum Heide, Academic Teaching Hospital of the Universities of Kiel, Lübeck and Hamburg, Germany.
3 Professor, Institute of Diagnostic and Interventional Radiology/Neuroradiology, Westküstenklinikum Heide, Academic Teaching Hospital of the Universities of Kiel, Lübeck and Hamburg, Germany.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anna Schrum, WKK Heide Radiologie, Esmarchstraße 50, 25746 Heide, Germany.
E-mail: aschrum@wkk-hei.de
One of the less considered but radiologically characteristic signs in conventional radiographic imaging of the abdomen in acute pancreatitis is the so-called colon-cut-off-sign. This sign refers to the abrupt termination of gas filling of the colon at the level of the left flexure. The more distal part of the colon usually shows a markedly reduced or a lack of gas filling. This bowel gas distribution, which feigns a constriction of the colon at the left flexure, has been observed within the context of acute pancreatitis for over 50 years. The frequency and sensitivity of the Colon-cut-off-sign fluctuate considerably in different studies. It can also be demonstrated in computed tomography (CT) and in the retrograde contrast medium filling of the colon.
We report on a patient who was admitted to the department of internal medicine with pronounced, progressive upper abdominal pain, combined with fever, elevated CRP, lipase and amylase, and leukocytosis, with suspected pancreatitis. Colonoscopy was interrupted due to stenosis in the area of the left flexure, a stenosing tumour being suspected. Over the course of further diagnostics, the scanogram of the abdominal CT already showed a colon-cut-off-sign. In addition, exudative pancreatitis with a stenosing process in the area of the left colonic flexure was found. A solid tumour could be ruled out in repeated endoscopy.
Radiological signs, CT, Exudative pancreatitis
Case Report
A 53-year-old male patient was hospitalized with progressive upper abdominal pain. Physical examination findings: abdomen soft, no tenderness, no guarding, physiological peristaltic sounds. Laboratory results showed leukocytosis as well as elevated CRP, lipase and amylase. On the basis of the pronounced clinical symptoms, the patient was admitted to the department of internal medicine with the suspected diagnosis of a pancreatitis. As a result of pain exacerbation and an endoscopic examination in the area of the left flexure, the patient was referred to the department of radiology for a CT-scan of the abdomen. The abdominal CT was performed with oral contrasting of the gastrointestinal tract with water and rectal contrasting of the bowel with diluted gastrograffin as well as intravenous contrast medium (portal-venous phase, 3 mm slice thickness). The CT-scanogram showed an over-inflation of the transverse colon as well as the termination of contrast medium filling of the colon at the level of the left flexure [Table/Fig-1]. In comparison, the descending colon and the sigmoid colon showed a normal contrast medium filling. A review of the Spiral-CT revealed a thickening of the colon wall in the area of the left flexure and peripancreatic fluid flows [Table/Fig-2], which spread out caudally along the renal fasciae. The pancreas itself did not show any necrotic areas. A stenosing colonic tumour in the area of the left flexure was ruled out. Free intra-abdominal air was not detected. An ileus-typical distribution of bowel gas was not present either.
CT-scanogram after oral contrasting of the gastrointestinal tract with water and rectal filling with diluted gastrographin. Evidence of an over-inflation of the transverse colon (T) as well as termination of contrast medium filling of the colon at the level of the left flexure (arrow), the so-called colon-cut-off-sign. Pronounced contrast medium filling of the descending colon (D) and of the sigmoid colon (S)

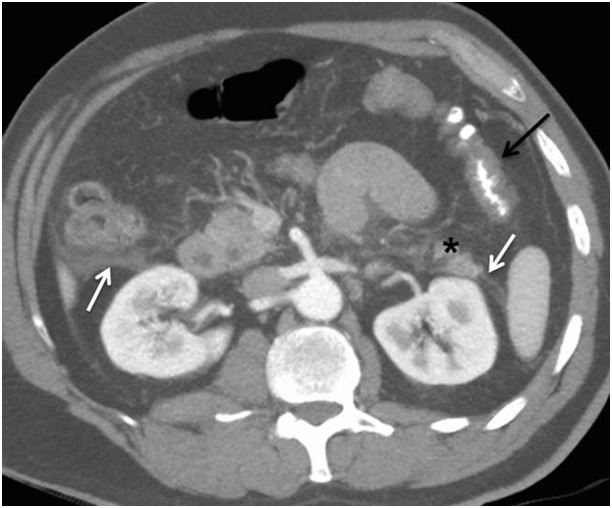
Abdominal CT after oral contrasting of the gastrointestinal tract with water and rectal filling with diluted gastrographin, as well as intravenous contrast medium administration; axial slice in the portal-venous phase.
Wall thickening of the left flexure (black arrow), the correlate of the colon-cut-off-sign. In the case of oedematous exudative pancreatitis, fluid flows are seen on the renal fasciae (white arrows). Section of the tail of the pancreas (asterisk)
Under abstinence from food and with antibiotic treatment (Metronidazole 400 mg (1-0-1) and Ceftriaxone 2g (1-0-0)) of the pancreatitis, the symptoms improved. A follow-up coloscopy did not produce any evidence of a cancerous process.
Discussion
The spread of inflammatory exudates along the phrenicocolic ligament including the transverse mesocolon is the reason for the constriction of the colon in the area of the left flexure, the correlate of the colon-cut-off-sign [1].
The phrenicocolic ligament is a fold of the peritoneum that extends from the left flexure to the postero-lateral surface of the left haemidiaphragm. This ligament marks the point at which the colon leaves the peritoneal space and represents an important anatomical endpoint for the spread of abdominal diseases. It is also connected to the medial surface of the transverse mesocolon as well as directly or indirectly to the gastrosplenic, gastrocolic and splenorenal ligaments. These ligamentous connections also explain why the different types of disease such as pancreatic and stomach cancer, splenic artery bleeding and the rupture of an abdominal aortic aneurysm can cause a circumscribed constriction of the colon in the left flexure [2–4]. The clinical pictures of the neoplastic and inflammatory diseases often show great similarities. The colon-cut-off-sign has even been described within the context of a ureter rupture in one case report [5].
The various different imaging methods used for clarification of acute pancreatitis differ in their level of diagnostic value. The value of epigastric ultrasonography in acute diagnostics is somewhat small, as an assessment of the pancreatic parenchyma is often limited by the over-inflation of the transverse colon and the ascending colon. This occurs in around 1/3rd of the patients in the acute stage of pancreatitis. The plain abdominal X-ray is often normal in the case of mild pancreatitis and is useful initially for excluding other abdominal pathologies, such as a hollow organ perforation with the collection of free air or an ileus. In severe cases, however, a locoregional reflectory ileus of the small intestine is often seen (sentinel loop) or a colon-cut-off-sign in the area of the left colonic flexure. The first-line procedure for excluding complications remains the CT or alternatively magnetic resonance imaging, if possible combined with magnetic resonance cholangiopancreatography (MRCP).
Over the past years, computed tomography has clearly made for quicker diagnosis of acute pancreatitis. CT is not only suitable for confirming the clinical diagnosis but also for classifying the stage of the disease and for excluding other abdominal diseases. In particular the differentiation between necrotic and oedematous-exudative pancreatitis is possible CT-morphologically [6]. Conclusions may be drawn as to the prognosis under correlation with the clinical parameters and using the CT Severity Index developed by Balthazar [7] and the Modified CT Severity Index developed by Mortele et al., [8]. Complications of pancreatitis, such as fluid-collections or retentions and pseudocysts or abscess-formations as well as bleeding and biliary obstruction are also detectable [6]. It is also possible to clearly determine vascular complications such as pseudoaneurysmas [9] or portal vein thrombosis [10]. Despite the advantages of CT-imaging for the exclusion of complications in the diagnosis of acute pancreatitis, the recognition of guiding radiological findings such as the colon-cut-off-sign on a conventional abdominal overview image remains important, as this is often the first imaging method performed.
Conclusion
In acute diagnosis, when investigating unclear abdominal symptoms, the CT-scanogram prepared for planning the field of examination may provide information on a level of importance equivalent to that of the conventional radiograph. A colon-cut-off-sign that can already be distinguished in the scanogram should already bring to mind important differential diagnoses of pathologies in the area of the left upper abdomen, such as pancreatitis, rupture of an abdominal aortic aneurysm or tumours of the stomach and colon.
[1]. Pickhardt PJ, Signs in Imaging, the Colon Cut-off SignRadiology 2000 215:387-89. [Google Scholar]
[2]. Oliphant M, Berne AS, Meyers MA, The subperitoneal space of the abdomen and pelvis: planes of continuityAJR Am J Roentgenol 1996 167:1433-39. [Google Scholar]
[3]. Mohiuddin S, Sakiyalak P, Gullick HD, Stenosing lesions of the colon secondary to pancreatitisArch Surg 1971 102:229-31. [Google Scholar]
[4]. Politoske EJ, Ruptured abdominal aortic aneurysm presenting as an obstruction of the left colonAm J Gastroenterol 1990 86:745-47. [Google Scholar]
[5]. Liao MT, Chang WC, Tsai SH, Huang GS, Yu CY, The colon cutoff sign: an unusual indicator of urologic diseaseUrology 2008 71:1052 [Google Scholar]
[6]. Sureka B, Bansal K, Patidar Y, Arora A, Imaging lexicon for acute pancreatitis: 2012 Atlanta Classification revisitedGastroenterol Rep (Oxf) 2015 :piigov036 [Google Scholar]
[7]. Balthazar EJ, Robinson DL, Megibow AJ, Ranson JH, Acute pancreatitis: value of CT in establishing prognosisRadiology 1990 174:331-36. [Google Scholar]
[8]. Mortele KJ, Wiesner W, Intriere L, A modified CT severity index for evaluating acute pancreatitis: improved correlation with patient outcomeAJR Am J Roentgenol 2004 183:1261-65. [Google Scholar]
[9]. Moll R, Debus S, Franke S, Schindler G, Pseudoaneurysm of the right gastric arteryVasa 2002 31:205-08. [Google Scholar]
[10]. Easler J, Muddana V, Furlan A, Portosplenomesenteric venous thrombosis in patients with acute pancreatitis is associated with pancreatic necrosis and usually has a benign courseClin Gastroenterol Hepatol 2014 12:854-62. [Google Scholar]