Case Report
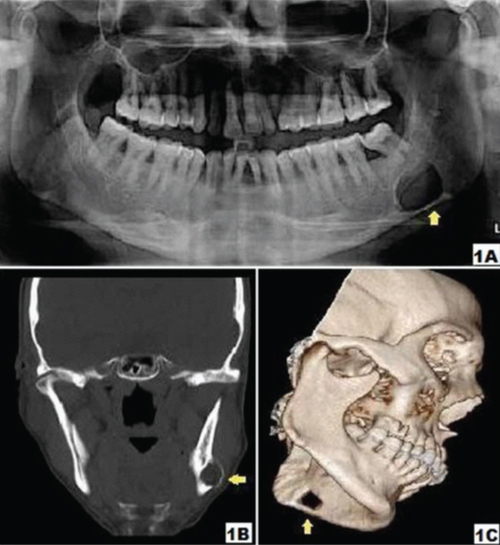
Case 1
A 45-year-old male patient was referred with a panoramic radiograph by a local practicing dentist for an opinion regarding radiolucent lesion in mandible [Table/Fig-1a]. On viewing the radiograph, it was observed that a well defined, unilocular, corticated, oval shape radiolucent lesion of size 3.8 cm; was noted in the left posterior mandible below the inferior alveolar canal. The thinning of inferior border of mandible was distinctly noted. The posterior teeth showed no pathology. The medical history, clinical examination & clinical tests were noncontributory. The coronal view of computed tomogram (CT) showed hypodense lesion with thinning and expansion of buccal cortical plate [Table/Fig-1b]. The 3D reconstructed CT showed bone defect in the left posterior mandible, with soft tissue density (adipose tissue) [Table/Fig-1c]. Based on these findings, the diagnosis of Stafne’s bone cavity was made. The patient is on regular follow-up since two years with no changes in the lesion.
Panoramic radiograph: (a) showing well-defined unilocular, corticated, oval shape radiolucent lesion below the inferior alveolar nerve canal apical to left third molar. Note the thinning of inferior border of mandible (arrow); (b) shows coronal view of CT scan showing hypodense lesion with buccal cortical plate expansion; (c) shows 3D reconstructed CT scan
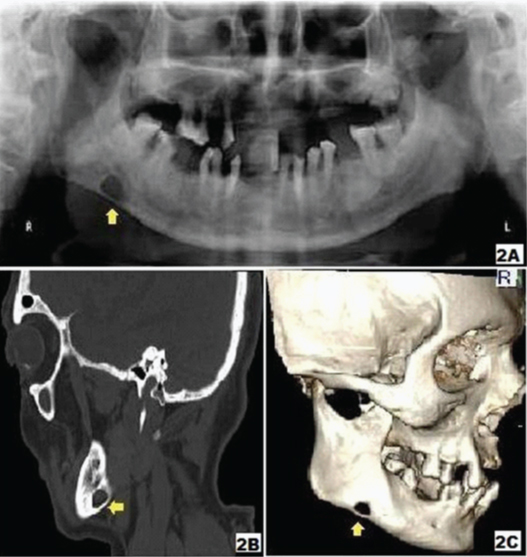
Case 2
A 57-year-old male patient was referred from a rural health centre with a panoramic radiograph [Table/Fig-2a] for an opinion of a lesion on right posterior mandible. The radiolucent lesion presented as a well-defined, unilocular, corticated and oval shape, of size 2 cm; below the right inferior alveolar canal. The thinning of inferior border of mandible was distinctly noted. The medical history, clinical examination and clinical tests were noncontributory. The sagittal view of CT scan [Table/Fig-2b] showed well defined cavity with thinning and expansion of bucco-lingual cortical plate. The 3D reconstructed CT [Table/Fig-2c] showed a demarcated bone defect in the right posterior mandible. The content of the cavity and the soft tissue density suggested presence of adipose tissue. Based on these findings, the diagnosis of Stafne’s bone cavity was made. The patient is on regular follow up since 12 months with no alteration in the lesion.
Panoramic radiograph: (a) showing well defined unilocular, corticated, oval shape radiolucent lesion below the inferior alveolar nerve canal apical to right third molar. Note the thinning of inferior border of mandible (arrow); (b) shows sagital view of CT scan showing well defined hypodense lesion on the right side of the mandible; (c) shows 3D reconstructed CT scan
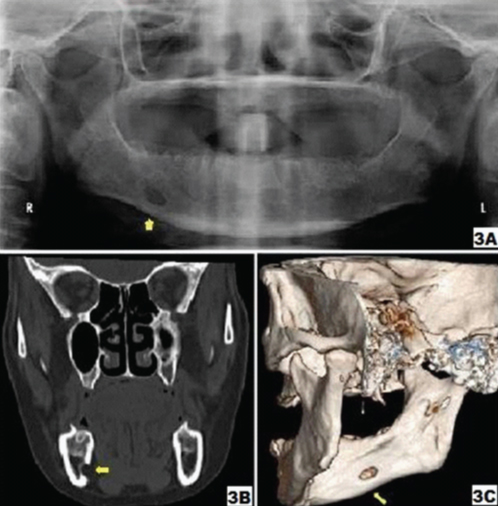
Case 3
A 64-year-old female was referred by a practicing dentist with a panoramic radiograph for a specialist opinion regarding radiolucent lesion in the right mandible [Table/Fig-3a]. On construing, it was observed that a well-defined, unilocular, corticated, oval shape radiolucent lesion of size 1.8 cm; was present below the right inferior alveolar canal. The medical history, clinical examination and clinical tests were noncontributory. The coronal view of CT scan showed a well-defined cavity with thinning and minor expansion of lingual cortical plate [Table/Fig-3b]. The 3D reconstructed CT revealed a cortical defect on the lingual surface of right body of mandible [Table/Fig-3c]. The density of the soft tissue in the defect was of adipose tissue. Based on these findings, the diagnosis of Stafne’s bone cavity was made. The patient is on regular follow up since ten months and no radiographic changes are observed.
Panoramic radiograph: (a) showing well-defined unilocular, corticated, oval shape radiolucent lesion below the inferior alveolar nerve canal apical to right second molar region (arrow); (b) shows coronal view of CT scan showing well-defined hypodense lesion on the right side of the mandible; (c) shows 3D reconstructed CT scan
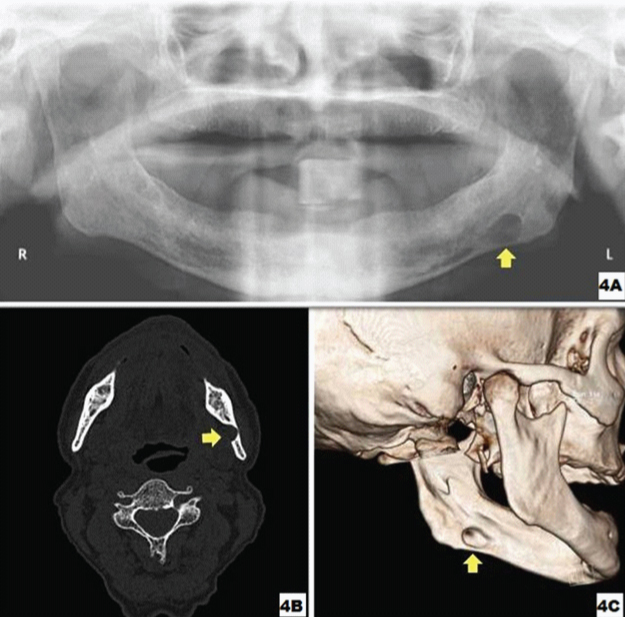
Case 4
A neurophysician treating a 72-year-old male for neuralgia of mandibular nerve, referred him with a panoramic radiograph to rule out nerve tumour in the left body of mandible [Table/Fig-4a]. On viewing, it was observed that a well defined, unilocular, corticated, oval shape radiolucent lesion of size 2.5 cm; was located below the left inferior alveolar canal. The medical history, clinical examination and clinical tests were noncontributory. The axial view of CT scan showed well defined defect with thinning of buccal cortical plate and discontinuity of lingual plate [Table/Fig-4b]. The 3D reconstructed CT revealed a cortical defect on the lingual surface of left body of mandible, with soft tissue density (adipose tissue) in the centre [Table/Fig-4c]. Based on these findings, the diagnosis of Stafne’s bone cavity was made. The patient’s apprehension was solved and is on regular follow-up since six months and no radiographic changes are noted.
Panoramic radiograph: (a) showing well-defined unilocular, corticated, oval shape radiolucent lesion below the inferior alveolar nerve canal apical to left third molar region (arrow). Note the thinning of inferior border of mandible (arrow); (b) shows axial view of CT scan showing well-defined hypodense lesion on left side of mandible; (c) shows 3D reconstructed CT scan
Case 5
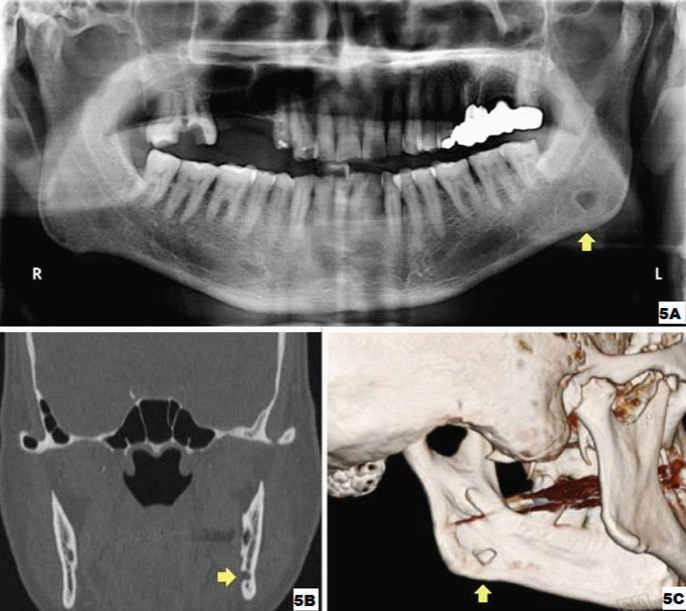
A 64-year-old male was referred by a practicing prosthodontist with a panoramic radiograph for an opinion regarding radiolucent lesion in the left angle of mandible [Table/Fig-5a]. It was observed that a well-defined, unilocular, corticated, oval shape radiolucent lesion of size 0.8 cm; located below the inferior alveolar canal. The medical history, clinical examination and clinical tests were noncontributory. The coronal view of CT scan showed well-defined cavity and discontinuity of lingual plate [Table/Fig-5b]. The 3D reconstructed CT revealed a cortical defect on the lingual surface of mandibular angle [Table/Fig-5c]. The soft tissue density in the defect was suggestive of adipose tissue. The diagnosis of Stafne’s bone cavity was made. The patient is on regular follow up since six months and no radiographic changes are noted.
Panoramic radiograph: (a) showing well-defined unilocular, corticated, round shape radiolucent lesion below the inferior alveolar nerve canal apical to left third molar (arrow); (b) shows coronal view of CT scan showing the hypodense lesion with discontinuous lingual cortical plate; (c) shows 3D reconstructed CT scan
Discussion
Stafne’s bone cavity (SBC) is a rare, asymptomatic, localized, non-progressive, non healing, unilateral oval shaped radiolucent defect in the posterior region of the mandible usually in the first molar to angle area below the mylohyoid line and the inferior alveolar canal and above inferior border of mandible [1–8]. It was first described by Edward C. Stafne in 1942 [9]. Several terms have been used to describe this entity, like Stafne static bone defect, Stafne cyst, static bone cyst, Stafne cavity, latent bone cyst, static bone cavity, lingual mandibular bone depression and idiopathic bone cavity [2–4,7,10]. SBC is an invagination in the medial surface of the mandible and is considered as pseudocyst. The cavities are assumed to be formed by the remodeling of the mandibular cortex around the extension of salivary gland tissue [3–6,11]. SBC is thought to be developmental in origin, although it does not appear to be present since birth. Till date, cases reported in the literature are mostly after 40 years of age and none affecting children.
This paper illustrates five rare cases of Stafne’s bone cavity which were either referred for opinion or were wrongly diagnosed by practicing health professionals as jaw tumor leading to psychological distress in these patients. This article also focuses on reviewing the published literature, differential diagnosis along with use of various diagnostic imaging resources for this bone defect and to add five new Indian cases to the scientific literature.
Stafne’s bone cavity (SBC) is a localized, non-progressive, non- healing lesion of mandible [1,3,4,7,8]. In past it was considered as a cyst, but rather it is a variation in the development of the bone cortex and hence the term cavity or defect is more appropriate. The scientific literature states four types of SBC - posterior lingual, anterior lingual, buccal aspect of ascending ramus and lingual aspect of ascending ramus. The posterior lingual variant is most frequently seen on radiograph in submandibular gland fossa, with an incidence between 0.10% and 0.48%. The anterior lingual variant is rare and usually situated between the mandibular incisor and premolar area, above the insertion of mylohyoid muscle. The buccal or lingual variant is located on the ascending ramus and is an unusual finding [1,2,10].
The cause and pathogenesis of SBC is still uncertain. Various hypotheses are proposed in the development of SBC and they are: the mandible developing around the lobe of the submandibular salivary gland during embryonic life; deficient bone formation; abnormal vascular pressure from facial artery leading to necrosis; and resorption of adjacent bone. The most commonly accepted view is that it originates from the pressure applied by the glandular tissue on the lingual cortex of the mandible [5,7,10,11]. The submandibular gland is directly related with the posterior variant, while the sublingual gland is related to the anterior variant, and the parotid gland with the two variants of the ascending ramus of mandible. The bone defect is either empty or frequently contains salivary gland, adipose tissue, connective tissue, muscles, blood vessels and rarely lymph nodes [1,3,4,6–11]. In all the present cases, the lesion was located anterior to the distal border of mylohyoid muscle and the radiographic features were consistent with adipose tissue.
SBC is asymptomatic and seen commonly in males than females with a ratio of 6:1 [1,7,10] and usually after the age of 40 years; which is in consistent to our present case series wherein all our cases were above 45 years of age and the male to female ratio is 4:1. It is generally detected incidentally on routine radiographs of mandible, as was in all our cases. Radiographically, the cavity appears as an elliptical, oval or round homogeneous well-defined unilocular radiolucency, often with a sclerotic margin, and between 1 to 3 centimeter in size, located in the first molar to angle area below the mylohyoid line and the inferior alveolar canal and above inferior border of mandible [1–8]. All these features were present in all our cases except that the size of SBC varied from 0.8 cm to 3.8 cm. However, bilobate lesions, bilateral lesions, lesions above the inferior alveolar canal, and lesions without sclerotic margins have also been reported [2–8].
The three dimensional images will assist in final diagnosis of SBC. The size and extent of the cavity is best seen with computed tomography scan (CT) using both soft tissue and bone window settings. Segev et al., stated that CT scans should be supported with Magnetic Resonance Imaging (MRI) to know the content of the cavity [6]. Sialography can also be used to determine the presence of glandular tissue in the bone cavity; although it is difficult to perform and the procedure is painful [3–5,8,10]. In the present case series; the axial, coronal and sagittal CT images using both soft-tissue and bone window settings in all the cases confirmed the content of SBC of having adipose (fat) tissue.
Irrespective to the content of SBC, it is significant to differentiate the asymptomatic bone cavity from other intraosseous pathologies like keratocystic odontogenic tumour, ameloblastoma, fibro-osseous lesion, traumatic bone cyst, eosinophilic granuloma, multiple myeloma and primary or metastatic malignant lesions of jaw [1,4–7,10,11]. Diagnostic evaluation is usually required to rule out intraosseous lesions. Importantly, absence of bucco-lingual swelling and symptomless lesion is enough to rule out possible benign or primary malignant odontogenic pathologies. In all our cases, the different views of CT scan using soft-tissue window as well as on 3D reconstruction images showed buccal &/or lingual bone defect with irregular borders and presence of adipose tissue.
The diagnosis is usually made on a clinical presentation, typical radiographic location and lack of symptoms. It can be confirmed by CT scan or Magnetic resonance imaging (MRI). Biopsy is not required for the diagnosis. Biopsy if performed, then salivary gland tissue is usually seen. However, muscle, blood vessels, fat, connective tissue, or lymphoid tissue may also be seen. Treatment is not recommended but periodic follow up along with panoramic radiograph is advisable, although the cavity is static and benign in nature. Surgical intervention should be performed only in cases of uncertain diagnosis or in exceptional cases where the pathology is unusually severe. Diagnostic dilemma can lead to unnecessary treatment like endodontic treatment, osseous trephination and osseous exploration [2,5,6,10,11].
Conclusion
Stafne’s bone cavity is an incidental finding on the radiograph which should be usually confirmed by CT scan &/or MRI so as to avoid invasive procedures. General dentist should not consider all radiolucencies as pathological lesions and should use advanced imaging modalities in doubtful cases. Regular follow-up with radiographic monitoring is recommended.
[1]. Etoz M, Etoz O, Sahman H, Sekerci A, Polat H, An unusual case of multilocular Stafne bone cavityDentomaxillofacial Radiology 2012 41:75-78. [Google Scholar]
[2]. Quesada-Gomez C, Valmaseda-Castello E, Berini-Aytes L, Gay-Escoda C, Stafne bone cavity: a retrospective study of 11 casesMed Oral Patol Oral Cir Bucal 2006 11:E277-80. [Google Scholar]
[3]. Terro W, Crean J, Not all radiolucent images are pathological lesions (Stafne cyst)Dental News 2006 13(3):22-27. [Google Scholar]
[4]. Branstetter B, Weissman J, Kaplan S, Imaging of a Stafne Bone Cavity: What MR Adds and Why a New Name Is NeededAm J Neuroradiol 1999 20:587-89. [Google Scholar]
[5]. Belmonte R, Velez M, Garcia F, Garcia A, Infante P, A Stafne’s cavity with unusual location in the mandibular anterior areaMed Oral Patol Oral Cir Bucal 2005 10:173-79. [Google Scholar]
[6]. Segev Y, Puterman M, Bodner L, Stafne bone cavity – Magnetic resonance imagingMed Oral Patol Oral Cir Bucal 2006 11:E345-47. [Google Scholar]
[7]. Dolanmaz D, Osman A, Etoz A, Pampu A, Kilic E, Sisman Y, Diagnosis of Stafne’s Bone Cavity With Dental Computerized TomographyEur J Gen Med 2009 6(1):42-45. [Google Scholar]
[8]. Sisman Y, Etoz O, Mavili E, Sahman H, Ertas E, Anterior Stafne bone defect mimicking a residual cyst: a case ReportDentomaxillofacial Radiology 2010 39:124-26. [Google Scholar]
[9]. Stafne EC, Bone cavities situated near the angle of the mandibleJADA 1942 29:1969-72. [Google Scholar]
[10]. Sisman Y, Miloglu O, Sekerci A, Yilmaz A, Demirtas O, Tokmak T, Radiographic evaluation on prevalence of Stafne bone defect: a study from two centres in TurkeyDentomaxillofacial Radiology 2011 000:1-7. [Google Scholar]
[11]. Nikzad S, Azari A, Khezri F, Diagnosis of a Lingual Mandibular Bone Defect (Stafne’s Bone Defect) by CT ScanIran J Radiol 2010 7(1):27-30. [Google Scholar]