Neuroendocrine tumours are uncommon tumours arising from ‘neuroendocrine cells’ in the body. These cells have their origin in the neuroectoderm. Otto Lubarsch, in 1888, first described carcinoid tumours when he reported 2 patients with ileal carcinoids discovered at autopsy [1]. In 1907, Siegfried Obendorfer, a German pathologist at the University of Munich, coined the term ‘Karzinoide’ or carcinoma-like to describe the tumour which appeared malignant on histology but behaved in a more benign fashion [2]. Recognition of endocrine properties of these tumours came to light when Rapport and his colleagues isolated serotonin (5 HT) in 1952 [3]. Carcinoid tumours were found to arise from Kulchitsky or Enterochromaffin cells, which are part of the diffuse neuroendocrine system of the gastrointestinal tract. Lembeck identified serotonin in ileal carcinoids a year later in 1953 [4].
While no reliable epidemiological data is available describing the prevalence of carcinoid tumours in India, the estimated incidence of these rare tumours is about 5.25 per 100,000 people [5] accounting for just 0.66% of all malignancies in the west [6]. The incidence is likely to be falsely low in our country as accurate diagnostic facilities remain out of reach of the majority of the population, symptoms being non-specific and therefore the tendency of patients to present late in the course of the disease.
Most carcinoids arise in the gastrointestinal tract (55%) and broncho-pulmonary system (30%) [7]. The commonest location for these tumours is the small bowel [8] with nearly half of these (45%) occurring in the distal ileum [9]. Small bowel carcinoids present in the 6th to 7th decade [10] and up to 30% of these lesions are multiple [11]. Patients typically present with abdominal pain and/or sub-acute intestinal obstruction, which is due to the desmoplastic reaction in the mesentery leading to kinking of small bowel or direct luminal narrowing. Confirmation of diagnosis is based on histopathology with additional help from immunohistochemistry for Chromogranin A [12]. The extent of disease determines the 5-year survival, which is 65% for loco-regional disease [13]. There is paucity of data on small bowel carcinoids in our country, especially in the south Indian population. This study not only describes the symptoms and management of carcinoid tumours, but more importantly includes a sufficiently long follow up period as well.
Materials and Methods
A review of our hospital medical records in the study period showed 30 cases of small bowel tumours treated in the last 9 years. Of these 30 cases, 14 were carcinoids accounting for 46.6% of all small bowel tumours. The remaining included 10 cases of Gastrointestinal stromal tumour (GIST), 4 cases of lymphoma and 2 cases of adenocarcinoma. In total, 14 patients diagnosed with small bowel carcinoids, ten male and four female presenting to the Department of General Surgery at M.S. Ramaiah Medical Teaching Hospital over a period of 9 years from December 2005 to November 2014 were considered for the study [Table/Fig-1]. Their ages ranged from 43 to 67 years (Mean age: 54.4 years).
Distribution of small bowel carcinoids
| Carcinoid site | Number | % of Total | Male:Female | Stage | % of Total | Mortality |
|---|
| Jejunum | 2 | 14.3 | 2:0 | T3N0M0 = 2 | 14.3 | NIL |
| Ileum | 12 | 85.7 | 10:2 | T3N0M0 = 4 | 28.6 | NIL |
| | | | T3N1M0 = 4 | 28.6 | 1 |
| | | | T3N1M1 = 4 | 28.6 | 1 |
All the patients were symptomatic. The duration of symptoms varied from 1.5 to 10 years (Mean duration: 7 years). Intestinal colic was the commonest symptom in 12 out of 14 patients; two patients with jejunal carcinoids had epigastric pain mimicking peptic ulcer disease of 10 years duration. Twelve patients presented with intermittent sub-acute intestinal obstruction of nearly one and a half years duration after having non-specific abdominal symptoms for few years. Eight patients had significant loss of weight. Clinical findings were of mildly distended abdomen with intermittent borborgymi in those with sub-acute obstruction (12 patients) of which two patients had an ill-defined lower abdominal mass in the right iliac fossa and hypogastrium. In the remaining 2, there were no abdominal findings [Table/Fig-2].
| Carcinoid Site | Symptoms | Clinical Examination |
|---|
| Epigastric Pain | Intestinal Colic | Features of Intermittent SAIO | Abdominal Distention | Intestinal Borborgymi | Abdominal Mass | None |
|---|
| Jejunum | 2 | - | - | - | - | - | 2 |
| Ileum | - | 12 | 12 | 12 | 12 | 2 | - |
All patients underwent X-ray abdomen in erect and supine views showing dilated jejunal coils in 12 patients with sub-acute intestinal obstruction (SAIO). Eight patients underwent thin barium study of the small bowel. Eight patients had a Computed Tomography (CT) Scan Abdomen with oral and IV contrast. The remaining could not afford a CT Scan. Oesophagogastroduodenoscopy (OGD) was performed in two patients in whom acid peptic disease was suspected. Colonoscopy was done in 2 patients.
Twelve patients with SAIO underwent laparotomy and two patients with epigastric pain underwent a laparoscopy-assisted procedure. All tumour specimens were analysed histologically and immunohistochemically for Chromogranin A activity after the histological diagnosis of carcinoid tumour was made. Postoperatively 24 hour urinary 5-hydroxy indole acetic acid (5HIAA) level was assessed in all the patients. All patients included in the study were regularly followed up. The study was approved by the Academic & Institutional Ethical Committee of MS Ramaiah Medical College.
Results
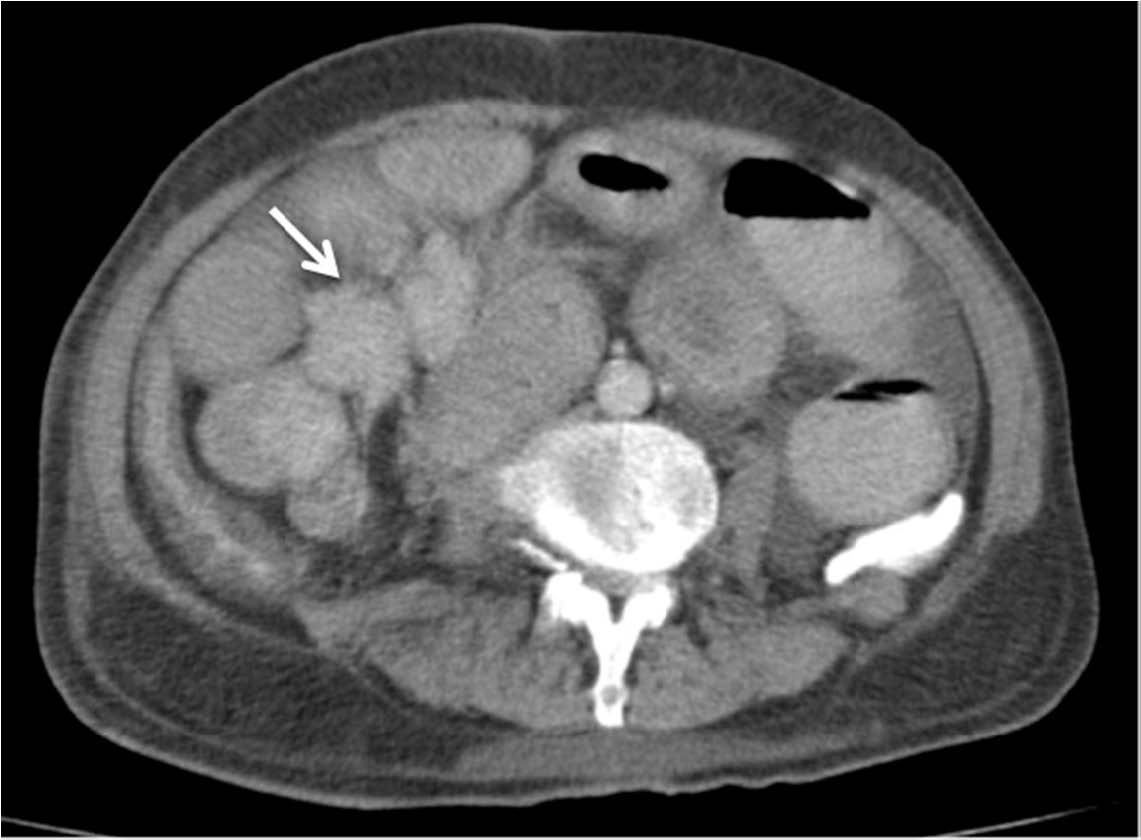
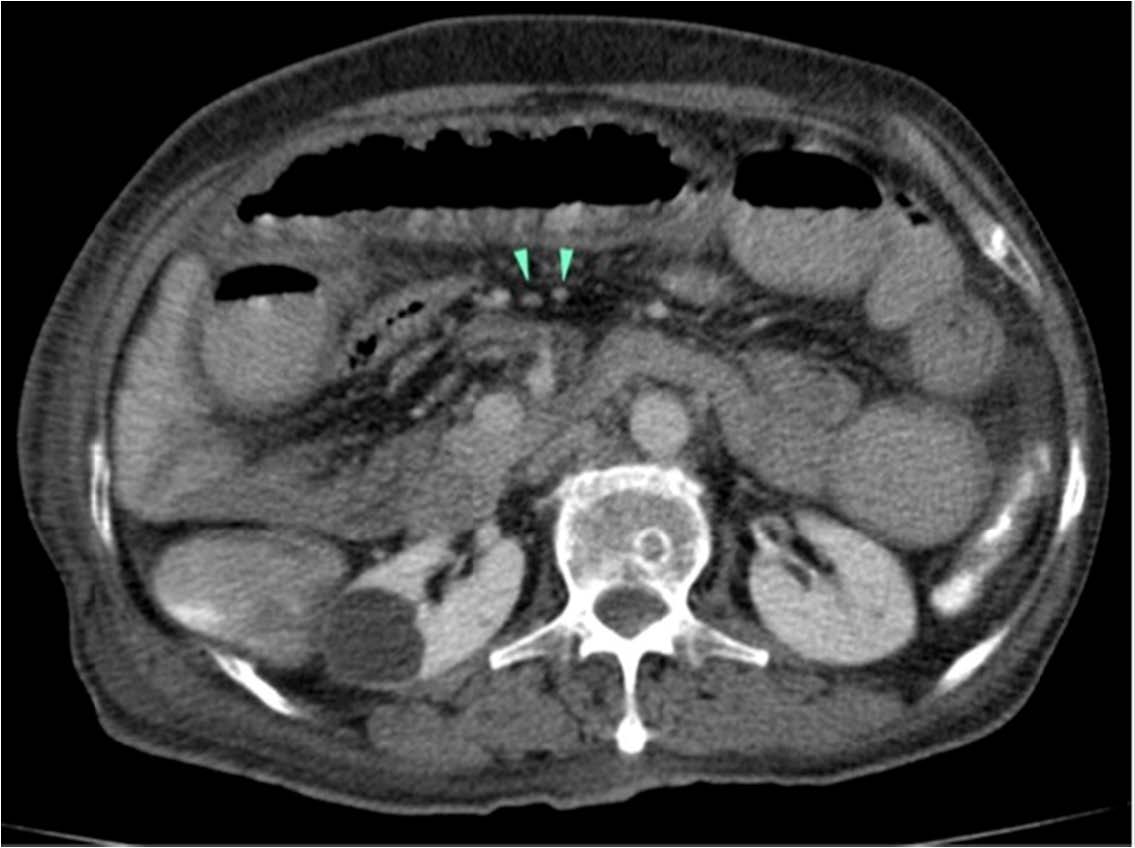
Fourteen patients of small bowel carcinoid tumours were included in the study after review of medical records. Along with the clinical features mentioned earlier in methodology, X-Ray abdomen was suggestive of small intestinal obstruction in 12 patients. In 8 patients in whom it was performed, barium study showed dilated loops of small intestine in all. In the contrast enhanced CT (CECT) abdomen of 6 patients, small bowel (ileal) narrowing with proximal dilatation was seen. In two, cocooning of ileal loops at the ileo-caecal junction was seen, along with mesenteric lymph node enlargement but there were no findings suggestive of carcinoid [Table/Fig-3,4]. Colonoscopy performed in 2 patients showed features of large bowel obstruction at the ileo-caecal junction. Oesophagogastroduodenoscopy of the 2 patients with epigastric pain was normal. Based on the clinical and radiological features, the pre-operative diagnosis considered was stricture of the ileum probably due to tuberculosis in 8 patients, caecal carcinoma in two and acid peptic disease in two other patients with jejeunal carcinoids who had abdominal symptoms for the preceding 8 to 10 years. In the two patients presenting more recently in the series, a small bowel GIST was suspected on clinical grounds due to the ill-defined mass felt per abdominally in them and the presence of ileo-caecal obstruction. In none, a preoperative diagnosis of carcinoid of small bowel was entertained [Table/Fig-5].
CT Abdomen showing spiculated masss (arrow) arising from distal ileum
Mesenteric lymph node enlargement on CT abdomen (arrow heads)
Preoperative investigations and diagnoses
| Carcinoid Site | Pre-operative Diagnosis | Pre-operative investigations |
|---|
| Abdominal X Ray (all 14 patients) (All 14 Patients) | Barium Study (8 Patients) | CECT Abdomen (8 Patients) | Esophago-Gastro-Duodenoscopy (2 Patients) | Colonoscopy (2 Patients) |
|---|
| Jejunum | APD = 2 | NORMAL | – | – | NORMAL | - |
| Ileum | Ileal Stricture (? TB) = 8 | Dilated Jejunal Coils | 6 Cases: Ileal Narrowing Dilated Small Bowel Loops | 6 Cases with Ileal Narrowing & Proximal Dilation | – | – |
| Carcinoma Caecum = 2 | Dilated Proximal Small Bowel | 2 Cases: Ileal Narrowing & Dilated Proximal Bowel | – | – | – |
| Small Bowel GIST = 2 | Dilated Proximal Small Bowel | | 2 Cases: Cocoon of Ileal Loops at the IC Junction + Enlarged Lymph Nodes | | Features Suggestive of Large Intestinal Obstruction at IC Junction |
Intraoperatively, the more recent 8 patients were diagnosed to have carcinoid of the small intestine due to the experience gained from the previous 6 cases. All cases had solitary tumours of the small bowel. All showed desmoplasia of the mesentery with kinking of the small bowel. Ten patients underwent resection anastomosis of the tumour-bearing segment of small intestine with a minimum of 3cm clear surgical margins with removal of adjacent mesentery. Four of the 14 patients underwent right hemicolectomy due to the close proximity of the tumour to the ileo-caecal junction. Eight out of fourteen patients showed lymph node enlargement in the mesentery [Table/Fig-6]. The liver and peritoneum were normal in ten patients. In four patients who also had lymph node enlargement, liver metastases were found. None of the patients demonstrated features of carcinoid syndrome.
Resected bowel containing ileal carcinoid with cocooning of small intestinal loops (white arrow) that caused intestinal obstruction; excised mesenteric lymph node mass (yellow arrow)

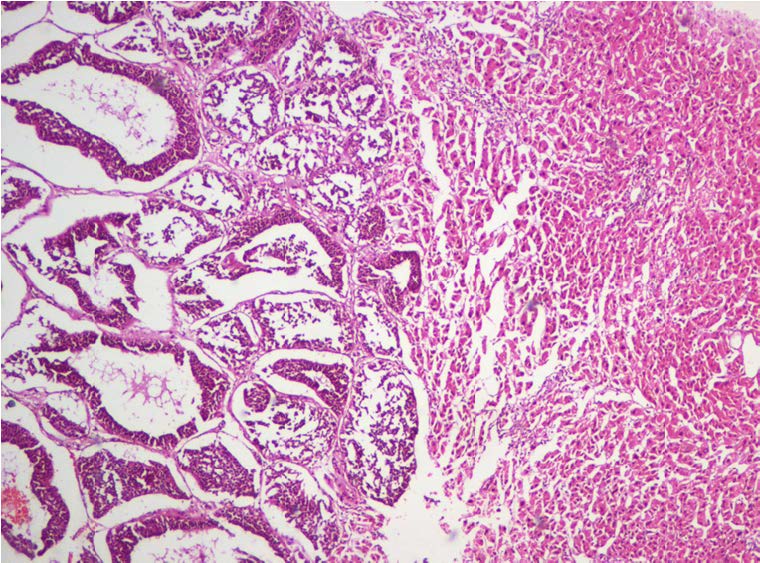
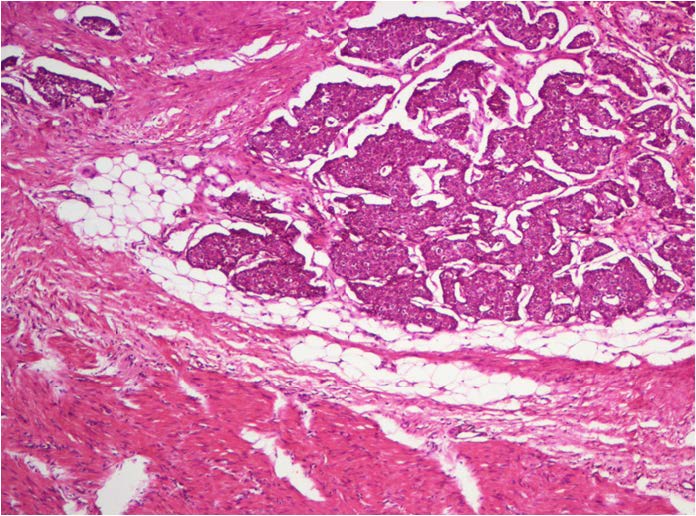
The cut surface of gross specimen showed polypoidal type of lesions with stenosis of the affected segment in all cases. Histopathological examination confirmed carcinoid tumour of the small bowel in all the cases [Table/Fig-7]. There was lymph node metastasis in eight of them who had macroscopically enlarged lymph nodes in the mesentery and four of these patients additionally had liver metastases, which were confirmed on liver biopsy [Table/Fig-8]. Of these 4 patients with liver metastasis, 2 underwent metastasectomy as they were solitary, while only biopsy was done in the other two as they had multiple liver metastases.
Microscopy: H&E stained section showing tumour cells invading intestinal muscle coat (20X)
Microscopy: H&E stained section showing metastatic tumour cells in biopsied liver nodule (20X)
Postoperatively 24 hour urinary 5-hydroxy indole acetic acid (5HIAA) level was assessed and found to be normal in 12 patients while being mildly raised in two of them. All patients showed positivity for Chromogranin A on immunohistochemistry [Table/Fig-9]. Twelve patients recovered uneventfully and at a mean follow up of 4.3 years were found to be free of disease. Two of the patients died, 3 and 5 months respectively after right hemicolectomy due to inanition and intercurrent infection.
Operative procedure and postoperative investigations
| Carcinoid Site | Operative Procedure Performed | Post-Operative Investigations | |
|---|
| Diganostic Laproscopy with Open Resection Anastomosis | Laprotomy and (1) Resection anastomosis + (2) Lymphadenectomy + (3) Liver Metastasectomy/Biospy | 24 Hour Urinary 5 - HIAA | Histopathology | IHC for Chromogranin A |
|---|
| Jejunum | 2 | – | Normal | Jejunal Carcinoid | Positive |
| Ileum | – | (1) = 4 Patients(1) + (2) = 4 Patients(1) + (2) + (3) = 4Patients | Mild Raise in 2 of 12 CasesNormal in 10 Cases | Ileal Carcinoid + Lymph Node Mets. in 8; Liver Mets. in 4 | Positive |
Discussion
Carcinoid tumours of the small intestine are rare, slow growing neuroendocrine tumours arising from the enterochromaffin cells found in the crypts of Lieberkuhn. It gets its name from the fact that though benign it has carcinoma-like features microscopically [2]. The endocrine properties of carcinoid tumours were recognized in 1948 when Rapport et al., isolated and named Serotonin (5HT), as the vasoconstrictor substance in the serum. Lembeck identified Serotonin in an ileal carcinoid and confirmed it as the major hormone responsible for the Carcinoid syndrome [4,8]. The term enterochromaffin refers to the ability to stain with chromium or chrome salts in 5-HT containing cells. The term carcinoids in this era, is apt only for midgut i.e. small bowel carcinoids. The remaining carcinoid tumours should be termed neuro-endocrine tumours followed by their site of origin and the endocrinopathy that is present.
The incidence of carcinoid is increasing and this is thought to be largely due to the introduction of more sensitive diagnostic tools. The majority of the carcinoids are found within the gastrointestinal tract (55%) and bronchopulmonary system (30%) [7]. Population based statistics show that within the gastrointestinal tract, the small intestine is the most common site of carcinoids (45%) followed by rectum (20%), appendix (17%), colon (11%), stomach (7%). Far less common anatomical sites have been reported in literature, including breast, larynx, thymus and gall bladder [14–17].
Carcinoid tumours account for highest percentage of small bowel tumours, representing approximately 1/3 of all small intestinal neoplasia [13], with 75% of small bowel carcinoids arising in the distal ileum within 60cm of the ileocaecal valve [9]. The incidence of these tumours increases with their proximity to the caecum. In our institution, the retrospective analysis found small bowel to be the commonest site of carcinoids (60%) and carcinoid tumours to be the commonest variety of small intestinal neoplasms (46.6%). Due to the indolent nature of these tumours, patients usually have non-specific symptoms for years before presenting late in the course of the disease when the diagnosis is made. Patients in the present series had symptoms ranging in duration from 1.5 to 10 years with a mean of 7 years. They present in the 6th or 7th decade of life and manifest with either intestinal colic or intermittent partial intestinal obstruction and are found to be locally advanced on laparotomy. In 40% of patients, carcinoids are discovered during emergency surgery for small bowel obstructions. Tumour infiltration into the mesentery provokes an intense fibrotic reaction (desmoplastic) that results in kinking of small bowel and resultant ischemia leading to small bowel obstruction [10]. In our series, 12 out of 14 patients (71.4%) had intermittent small intestinal obstruction, and in 8 patients (57%) carcinoid was recognized intraoperatively.
As non-specific as the initial symptoms of carcinoids may be, specific diagnostic techniques enable identification and localization of these tumours. Twenty-four hour urinary serotonin metabolite measurement is one such biochemical method used. Strodel et al., found elevated 5 HIAA (5-hydroxy indole acetic acid) in 24-hour urinary samples to be 100 percent specific and 73% sensitive for these cases. The combination of elevated platelet serotonin levels and urinary serotonin along with raised 5-HIAA leverls may be accurate in identifying carcinoids in nearly 84% of patients [8].
Locally advanced disease with typical mesenteric involvement can be identified on CT abdomen scans as an ill-defined mass at the root of mesentery with characteristic radiating dense soft tissue strands caused by thickened neurovascular bundles [18]. CT scan was done in ten patients who had a localized disease, but did not suggest a diagnosis of carcinoid. CT and MRI are equally effective at demonstrating regional and distant metastasis with a sensitivity of 77% and 80% respectively yet can underestimate the extent of disease in 25% of the cases.
Octreoscan has been found to be superior to that of cross sectional imaging with CT or MRI. Localisation of the tumour site with Indium -111 (In 111) labeled Octreotide (Somatostatin receptor scintigraphy) is helpful. The diagnostic sensitivity of octreoscan ranges between 80-90% [19]. It can also be used as a follow up tool.
Small bowel carcinoids are frequently multiple, exhibiting multicentricity in up to 30% of cases [8] though our series was composed of only solitary small bowel carcinoids. They often display metastases to the regional lymph nodes (39%) or the liver (31%) [8]. In our series, in 8 out of 14 cases (57%) regional lymph node metastasis was noted, with four of these having distant metastasis to the liver (28.5%). Percentage of patients with carcinoid syndrome is however only 5-7% [8,20]. It is commoner in younger patients in whom carcinoid tumours also have a more aggressive course. None of the patients in the study developed features of carcinoid syndrome, even on follow up, in spite of the presence of multiple metastases in two patients.
The preferred treatment remains radical surgical resection. The extent of resection depends on the size and location of the primary tumour. The resection of the small bowel primary with the mesenteric nodal disease is effective in relieving symptoms of gastrointestinal obstruction and was true in all the patients. This also leads to improved survival compared to patients in whom this cannot be achieved. An 83% 5-year survival rate has been described following surgery (cyto-reductive therapy) for the primary tumour [21]. All the patients in present series had localized or loco-regional disease and 12 out of 14 patients were disease free at a mean follow up of 4.3 years.
Carcinoid tumours are composed of small epithelioid cells, of low mitotic index with occasional acinar or rosette formation. Mixed tumours with acinar and glandular features have a median survival of 4.5 years and carry the best prognosis while poorly differentiated ones with the worst prognosis have a median survival of only 0.5 years. Nine of the cases (64.3%) had well differentiated tumours and the remaining 5 (35.7%) had moderately differentiated tumours. Diagnosis was additionally confirmed by immunohistochemical positivity for Chromogranin A which is the major granin expressed in gastric carcinoids and in serotonin producing carcinoids of the ileum and appendix. It is elevated in 85 to 100% of carcinoids regardless of functionality of the tumour [22]. All of our patients showed Chromogranin A positivity on immunohistochemistry.
Survival depends on stage or extent of carcinoid disease, tumour histology (grade), depth of tumour invasion and gender, race and age [5]. The Surveillance Epidemiology and End Results (SEER) Programme data showed overall 5-year and 10-year survival rates for well to moderately differentiated small bowel carcinoids to be 65% and 49% for localized disease, 71% and 46% for regional spread, and 54% and 30% for distant spread respectively [5].
Conclusion
Carcinoid tumours of the small bowel in southern India seems to be uncommon entity, compared to the Western population. In patients of the 5th decade or greater, with sub-acute intestinal obstruction or chronic abdominal pain, where intestinal tuberculosis is considered as a possible diagnosis, carcinoid tumours should be a differential diagnosis. Though the course of the disease is relatively benign, wide surgical resection of the lesion along with the mesentery and lymph nodes gives the best outcome. The diagnosis is often made intraoperatively on finding the presence of contraction and kinking of the mesentery due to desmoplastic reaction produced by the tumour. With the application of modern diagnostic tools such as CT and MRI in cases of chronic abdominal pain, it is possible that we will diagnose and identify these once thought to be elusive tumours more frequently than before.