The purpose of this study was to demonstrate atypical MRI features in cases of tubercular spondylitis resembling neoplastic lesions and to stress that tuberculous spondylitis should be one of the differential diagnosis in any spinal pathologies especially in developing countries.
Materials and Methods
This was a prospective study done in the patients diagnosed as tuberculous spondylitis on 0.2 T Siemens MRI between June 2011 and December 2014 in a tertiary care hospital in India. FSET2 Sagittal, SET1 Sagittal, FSET2 Axial, SET1 Axial sequences were done in all cases with additional FIR (Fat Suppressed) and SET1 Coronal sequence where ever required.
Inclusion Criteria: Patients diagnosed as tuberculous spondylitis with atypical MRI features such as :-
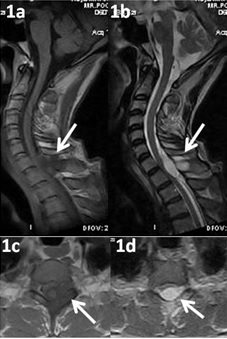
Selective involvement of posterior elements (pedicle, transverse & spinous processes and lamina) only [Table/Fig-1].
Bony Destruction without involvement of intervertebral discs [Table/Fig-2,3].
Solid soft tissue component (Intraspinal and pre & para vertebral [Table/Fig-4].
Noncontiguous bony lesions [Table/Fig-5].
T1(1a, 1c) & T2(1b, 1d) Axial and Sagittal images showing altered signal intensity in the spinous process of D1 vertebra (white arrows) with extradural soft tissue component compressing the spinal cord. Intervertebral disc and verterbral bodies appear normal
T1(2a) & T2(2b) Sagittal images showing altered signal intensity with reduction in height of D7 vertebral body (white arrows) with extradural soft tissue component compressing the spinal cord. Adjacent Intervertebral discs appear normal.

T2 Sagittal image showing altered signal intensity with bulging of posterior column of L3 vertebral body (white arrows). No soft tissue component seen. Adjacent Intervertebral discs appear normal

T1(4a) & T2(4b) Sagittal images showing altered signal intensity in the spinous process of D6 vertebra (white arrows) with extradural soft tissue component compressing the spinal cord. Intervertebral disc and verterbral bodies appear normal

Sagittal(5a), T2 Coronal (5b) and Sagittal (5c) images showing altered signal intensity involving the L2 vertebral body and spinous process of L3 vertebra with intraspinal and paraspinal soft tissue component (white arrows). Adjacent Intervertebral discs appear normal

Exclusion Criteria: Patients diagnosed as tuberculous spondylitis with typical MRI features such as contiguous bony lesions, Discitis/disc height reduction, Endplate changes and Pre and paravertebral abscess formation.
In 59 patients where MR imaging findings were atypical and there were imaging features which were equivocal or favoured the possibility of neoplastic lesion. Hence CT guided fine needle aspiration was done from the involved posterior vertebral elements and adjacent soft tissues, cytology showed caseating material and giant cells which were confirmatory for tubercular lesions. In our study we considered fine needle aspiration cytology gold standard for confirmation of the diagnosis.
Results
Among 59 cases, 37 cases were males (63%) showing ~2:1 ratio in our study. Cases of different age group varying from 20 – 65 years were seen in our study. Lumbo-sacral region involvement (30.5%) is the commonest in our study followed by dorsal and cervical region. Multiple level lesions are seen in 14 cases (23.7%) [Table/Fig-6]. All the 59 (100%) cases show no involvement of intervetebral disc. Posterior appendage involvement seen in 32 cases (54.2%) in which spinous process and lamina were affected in all the cases and only 8 cases showed involvement of pedicles. Soft tissue component seen in Intraspinal (37.2%) and paraspinal (45.7%) compartments [Table/Fig-6]. Cord compression seen in 19 cases (32.2%), out which only 7 cases (11.8%) shows cord oedema [Table/Fig-7].
Regional Involvement of Tuberculous Spondylitis
| S.No | Region | No. of Cases |
|---|
| 1. | Cervical | 11(18.6%) |
| 2. | Dorsal | 16(27.1%) |
| 3. | Lumbosacral | 18(30.5%) |
| 4. | Multilevel lesions | 14(23.7%) |
Various Pattern of Tuberculous Spondylitis
| S.No | Pattern of involvement | No. of Cases |
|---|
| 1. | Disc sparing | 59(100%) |
| 2. | Intraspinal soft tissue component | 22(37.2%) |
| 3. | Paraspinal soft tissue component | 27(45.7%) |
| 4. | Posterior appendages | 32(54.2%) |
| 5. | Cord compression | 19(32.2%) |
| 6. | Cord edema | 7(11.8%) |
Discussion
In 1782, Sir Percival Pott described the Tuberculous Spondylitis and surgical management of paravertebral abscess. Hence, tuberculous Spondylitis was coined as ‘Pott’s Disease’ [5]. Tubercular spondylitis is the commonest form of skeletal tuberculosis presenting as low grade chronic infection caused by Mycobaterium tuberculosis. Basic pathology in Tuberculous spondylitis is combination of osteomyelitis and arthritis involving more than one vertebra. In adults spinal TB classically present as spondylodiscitis involving the intervertebral disc second arily from adjacent infected vertebra whereas in children the disease primarily starts from the intervertebral disc due to the vascularized nature [6]. On X – ray, it presents as reduction of disc space, involvement of vertebral end plates, loss of cortical definition of the affected vertebra, variable degrees of vertebral collapse and rarely we can also see the paraspinal soft tissue component. It usually affects dorsal spine, however any part of spine may be involved. The usual patterns of vertebral involvement are paradiskal, anterior and central [3]. Tubercular involvement of posterior element is relatively less frequent [7].
Relative intervertebral disc preservation, vertebral endplates erosions, anterior wedging, pre & paravertebral and intraosseous abscesses with a subligamentous spread, vertebral body collapse, extradural, subdural and intramedullary tuberculomas are useful diagnostic clues for tuberculous spondylitis in MRI [6]. On MRI, typical tuberculous spondylitis appears as the involved vertebra and adjacent disc shows decreased signal intensity on T1W and increased signal intensity on T2W images with reduction of disc height and soft tissue component or collection in the paravertebral and intraspinal compartment. Jung NY et al., stated that thin and smooth enhancement of abscess wall and well defined paraspinal abnormal signal is more in favour of tubercular abscess [8]. Pyogenic and fungal spondylitis, sarcoidosis, metastasis and lymphoma are the close differential diagnosis for tuberculous spondylitis [9]. Differentiating tuberculous spondylitis from these conditions is very important since the line of management completely differs and also early intervention helps in minimizing the residual spinal deformity and permanent neurological deficits [10].
According to Osborn tuberculous spondylitis shows no gender predilection and is more common in younger age group in the developing countries, whereas in the western world, middle aged people (mean 40-45 years) are commonly affected [11]. But in our study cases of different age group varying from 20–65 years were seen. It correlates well with a study showing mean age of 39 +/- 16 years by Mirsaeidi et al., [12]. Our study shows tuberculous spondylitis has slight male predilection (63%). Thoraco-lumbar junction is most commonly affected in tuberculous spondylitis, but our study more number of cases were seen involving the lumbo-sacral region [3,6,9].
Contiguous involvement of two or more vertebral bodies are usually seen in spinal tuberculosis by hematogenous spread through the one vertebral artery feeding two adjacent vertebrae [13,14]. Noncontiguous multiple level vertebral body involvement is rarely seen in tuberculous spondylitis and only two level involvements is seen in most of the studies [13–16]. Recent studies show the incidence of multiple level contiguous vertebral involvements varies from 1.1-16% [17].
In our study multiple level skip lesions were seen in 14 cases (23.7%) without involvement of intervertebral discs. A study by Khattry et al., reported a case of tuberculous spondylitis in an adolescent was misdiagnosed as neopalstic disease, due to multiple skip lesions involving vertebral bodies and pedicles with sparing of the intervertebral discs. They stated that in a case of multilevel skip lesions of spine with sparing of intervertebral discs and absence of paravertebral soft tissue component favours neoplastic lesion whereas the presence of paravertebral lesion/collection favours tuberculous pathology [9].
Posterior element involvement is very rare in tuberculous spondylitis, however isolated posterior element involvement may be seen without other changes [18]. In a series of pott’s spine, 3 cases involving only the posterior arch which they described it as atypical of pott’s and typical of neoplasms [19]. Sinan et al., reported that 10% of their tuberculous spondylitis cases having isolated posterior arch involvement [20]. Our study shows 32 cases (54.2%) out of 59 cases of atypical tuberculous spondylitis shows posterior elements involvement.
Differential diagnosis of multiple spinal lesions must include tuberculous spondylitis, metastatic neoplasm and pyogenic spondylitis [21]. Nowadays presentation of tuberculous spondylitis are variable and atypical, hence whole body bone scan or MRI spine will be helpful in the diagnosis [21].
At times tubercular spondylitis may have a very bizarre appearance so that it cannot be differentiated from neoplastic lesions. Sometimes it presents without any bony involvement. Recognition of spinal TB in developed countries can be difficult because it is uncommon. It presents in a similar fashion to malignant deposits in the spine, which are encountered more frequently [5]. In a single vertebra disease, nutrition of the disc continues from the side of the healthy vertebra and hence the disc stays normal [22]. Hence disc involvement is not always necessary in spinal tuberculosis.
Atypical tuberculous spondylitis can be best evaluated with MRI, and it includes spondylitis without discitis, isolated central lesion in single vertebral body, non-contiguous skip vertebral body lesions, isolated posterior vertebral elements involvement and isolated intraspinal canal lesions. Image guided biopsy is very helpful for early diagnosis and prompt intervention if the clinical and imaging findings are not very helpful arriving diagnosis, especially with the atypical presentations [23].
Limitations
MRI has certain limitations, though it is very sensitive imaging modality to detect bone, soft tissue and disc changes at very early stage and we could even see subtle changes but specificity was not very high and we needed to confirm the diagnosis of tubercular lesions by other means, mainly by demonstrating the acid fast bacilli in sputum and by fine needle aspiration cytology from the lymphnodes, soft tissue and bony lesions.
Conclusion
On MRI, tubercular spondylitis may have variable pictures on imaging. In some cases we get atypical findings and it is difficult to diagnose it as tubercular lesion on imaging only. For any spinal and paraspinal lesions, we should also consider the possibility of tubercular aetiology along with other. Since early diagnosis avoids unnecessary delay in the treatment thereby reducing morbidity and possible complications.