Multiple myeloma (MM) is a bone marrow based multifocal plasma cell neoplasm associated with M-protein in the serum and/or urine and accounts for approximately 10% of all haematological malignancies [1]. It is the second most common haematological malignancy [2]. The disease spans a clinical spectrum from asymptomatic to aggressive forms due to deposition of abnormal immunoglobulin chains in tissues [1]. The diagnosis is established by a proper correlation of clinical history, physical findings, laboratory and radiological evaluation followed by confirmation with bone marrow findings. MM usually presents with anaemia, but pancytopenia as a presenting symptom of MM is unusual [2,3]. Here, we share our experience of ten cases of MM presenting as pancytopenia, and as such resulting in a prolonged work up of the patients before initializing the treatment.
Materials and Methods
In this retrospective study, cases which were diagnosed as multiple myeloma in the haematology department of Kasturba Medical College, Mangalore for a period of 30 months were collected. The complete blood picture, peripheral smear examination, bone marrow aspirate & protein electrophoresis of all the cases were reviewed. Cases of MM presenting with pancytopenia were included in the study. The inclusion criteria for pancytopenia was haemoglobin < 10gm/dl, total leucocyte count < 4000 cells/cumm and platelet count <1.5 lacs cells/cumm. Chemotherapy induced pancytopenia in known cases of myeloma were excluded from the study.
The clinical information and investigations were obtained from medical and laboratory archives. Laboratory variables analysed were haemoglobin, total leukocyte count, differential leukocyte count, platelet count, mean corpuscular volume (MCV), mean corpuscular haemoglobin (MCH) and mean corpuscular haemoglobin concentration (MCHC). The reticulocyte count & reticulocyte production index (RPI) were calculated for all the cases. Erythrocyte sedimentation rate (ESR) was estimated by Westergren’s method. Ethical clearance has been taken from institutional ethics board.
Results
During the study period, a total of 10 cases presented with pancytopenia. The mean age at presentation was 66.3 years (range: 59-72 years) with male: female ratio being 8:2. These patients presented to the outpatient clinic with non-specific symptoms; fatigue and weakness being the most common symptom (100%) and pallor being the most common sign (100%). Other presenting features were fever (4 cases, 40%), loss of appetite (3 cases, 30%), bone pain (2 cases, 20%) and loss of weight (1 case, 10%). Common infectious diseases like malaria and dengue were excluded in all the cases.
Average ESR was 104mm/hour. The mean values of haemoglobin, total leucocyte count and platelet count were 7.7mg/dl, 2898cells/mm3 and 68,200cells/mm3 respectively [Table/Fig-1].
Age & sex characteristics, Haemoglobin, TLC, Platelet count, ESR & bone marrow plasma cell percentage among the multiple myeloma cases
| Case | Age(years) | Sex | Hb(gm/dl) | TLC cells/mm3 | Platelet countcells/mm3 | ESR | BM plasma cell % |
|---|
| 1 | 68 | F | 10 | 3140 | 71,000 | 120 | 62 |
| 2 | 70 | M | 7 | 2630 | 1,03,000 | 100 | 74 |
| 3 | 72 | M | 8.2 | 3670 | 75,000 | 82 | 61 |
| 4 | 71 | M | 7.7 | 1220 | 18,000 | 124 | 78 |
| 5 | 59 | F | 9.4 | 3530 | 1,23,000 | 160 | 48 |
| 6 | 68 | M | 8.6 | 3750 | 56,000 | 110 | 63 |
| 7 | 61 | M | 5.3 | 2980 | 1,11,000 | 116 | 56 |
| 8 | 66 | M | 8.6 | 3760 | 53,000 | 140 | 69 |
| 9 | 65 | M | 3.5 | 2000 | 16,000 | 88 | 52 |
| 10 | 62 | M | 7.7 | 2300 | 54,000 | 68 | 68 |
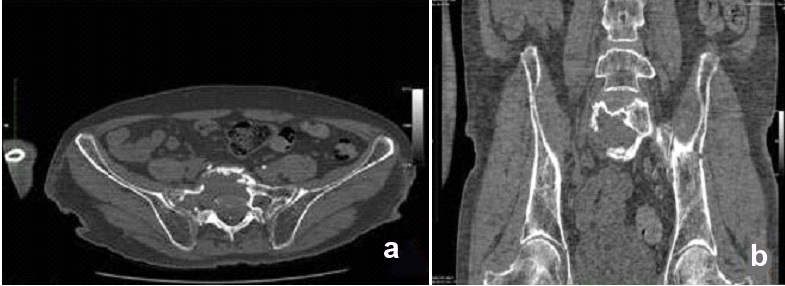
Imaging studies revealed lytic lesions of bone [Table/Fig-2a and 2b]. The peripheral smears reviewed showed normocytic normochromic anaemia with anisocytosis. Rouleaux formation was evident in 90% of cases [Table/Fig-2c and 2d]. Blood urea nitrogen and serum creatinine were increased.
a,b) Axial & coronal bone window CT images of pelvis at S1 level shows generalized osteopenia with multiple small punched out cortical & intramedullary lytic lesions involving left iliac bone & neck of left femur. Evidence of large well defined lytic lesion with adjacent areas of cortical breach involving S1 vertebral body & adjacent right sacral ala; c) Peripheral smear showing pancytopenia with significant rouleuxing & an occasional plasma cell. [Leishman stain, 400x]; d-f) Bone marrow aspirate showing high cellularity with increased number of plasma cells; e) binucleate plasma cells; & f) atypical plasma cells. [Leishman stain, 40x, 100x, 400x]
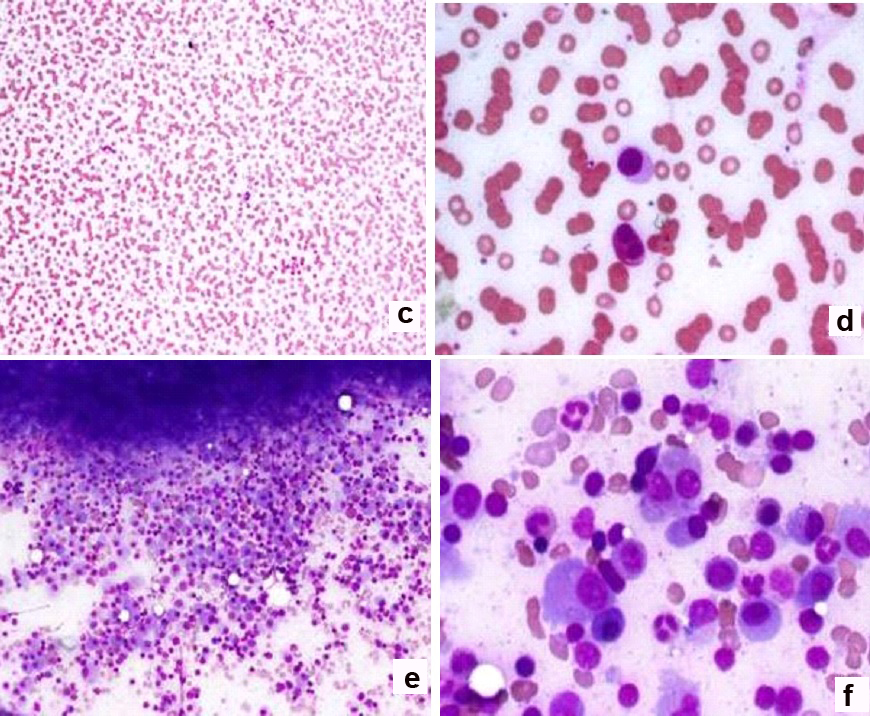
High-resolution serum electrophoresis, which was done in all cases, showed a dense, sharp to wide M band in the gamma globulin region. A 24-hour urinalysis by protein electrophoresis revealed positive urine Bence Jones protein in 100% cases. Bone marrow aspirations were hypercellular. Bone marrow plasma cell percentage was increased with an average of 63.1% [Table/Fig-2e and 2f]. Bone marrow biopsy correlation was obtained in 100% cases.
Discussion
According to World Health Organization (WHO), plasma cell myeloma, multiple myeloma or myelomatosis is a disease characterized by clonal proliferation of plasma cells in the bone marrow, which leads to suppression of normal haematopoiesis, destruction of bone, renal failure and recurrent infections [1].
The International Myeloma Working Group criteria is used for establishing the diagnosis of multiple myeloma that includes signs of end-organ damage such as hypercalcaemia, renal insufficiency, anaemia or bone lesions [2].
Anaemia is a common initial presentation in myeloma patients but in more advanced cases, thrombocytopenia and neutropenia may also develop leading to pancytopenia [3]. In such advance cases with unusual presentations, high index of suspicion aided by specific and reliable laboratory examinations including morphology are required for diagnosis and also to evaluate its aggressiveness and extent [4]. Pancytopenia in multiple myeloma may be attributed to several reasons. Most often it is due to the plasma cell proliferation replacing normal haematopoietic cells. Other causes include fas-ligand mediated apoptosis or cytokine-mediated bone marrow failure or even renal failure induced erythropoietin deficiency [5]. In this study, we emphasize diagnostic challenges of multiple myeloma manifesting as pancytopenia on initial presentation. The study also highlights the impact of morphology on the diagnostic and prognostic approach to MM with emphasis on the planning and monitoring of appropriate chemotherapy.
Myeloma is a disease which predominantly affects middle-aged and elderly persons. The median age of distribution is around 70 years [6]. The mean age of the patients of multiple myeloma who presented with pancytopenia in our study was 66.3 years with male predominance. The presenting symptoms were non-specific in nature such as weakness, fatigability, recurrent infections and sometimes bone pain [3]. Most of these non-specific symptoms were due to cytopenias secondary to suppression of haematopoiesis [3]. The extent of organ involvement, severity of complications, drug sensitivity and therefore the clinical course differed widely among patients [4]. Subramainain et al., has reported bone pain and fatigue as the most common presenting symptoms [7]. In our study, weakness and easy fatigability was seen in 100% cases but only 20% cases presented with bone pain.
Anaemia in myeloma and plasma cell percentage in the marrow are directly related to each other. As stated by Tsuchiya et al., the absence of anaemia is considered as one of the favourable prognostic factor in the long term survival of myeloma patients [7–9].
Most myeloma patients exhibit a tendency to bleed during their disease course. The incidence of abnormal bleeding is higher in more advanced phases, although it may be an early manifestation. The severity of bleeding in these patients may vary from petechiae to exsanguinations [1]. Even though bleeding manifestation is a well-known feature of myeloma, its pathogenesis has remained obscure. The proposed aetiologic factors often suggested have been; 1) the presence of abnormal plasma proteins impairing normal coagulation; and 2) deficient clot retraction, of unstated cause [10].
In present study, mean values of haemoglobin, total leucocyte count and platelet count were 7.7g/dl, 2898/cumm and 68,200/cumm respectively. A study conducted by Subramanian et al., [7] reported pancytopenia in 9% of multiple myeloma patients; however they also reported 71% of patients having haemoglobin of <8.5g/dL and thrombocytopenia of <1,00,000/cumm in 16.4% cases. In our study, peripheral smear showed rouleaux formation in 90% of cases which was in concordance with Subramanian et al., [7].
Bone marrow aspirates and biopsies were hypercellular with suppressed normal haematopoiesis and plasma cell proliferation. Ninety percent cases, showed a plasma cell percentage of >50% in the bone marrow aspirate which correlated with other studies [4]. In contrast to aspirate, the bone marrow biopsy showed >50% of plasma cells in all ten cases. Terpstra et al., Singhalet al., and Pich et al., have stated that biopsy tends to show a higher percentage of plasma cell infiltrate compared to aspirate [9,11,12]. A large study conducted by Weinzierl AP et al., demonstrated 10% or more clonal plasma cells in 96% of patients [13]. The patterns of plasma cell infiltration in the bone marrow biopsy were diffuse, nodular, and interstitial and mixed in 60%, 10%, 20% and 10% respectively.
On reviewing the large series reports and studies dealing with MM, it was found that a detailed analysis of pancytopenia in multiple myeloma has not been done. Rather, many studies on pancytopenia have reported MM as one of its cause [7,9]. In this study, we have analysed the haematological parameters, bone marrow findings and the plasma cell percentage in those patients presenting with pancytopenia.
MM patients are generally treated with alkylating agents, but, when associated with pancytopenia, these patients will require a mandatory addition of dexamethasone in order to avoid the haematopoietic stem cell damage by alkylating agents [14].
Conclusion
Presentation of multiple myeloma as pancytopenia is not uncommon. An elderly patient with non-specific complaints and a raised ESR is the usual presentation in multiple myeloma. The presence of pancytopenia may be misleading in such cases and hence may be a cause for delay in the diagnosis and treatment. A differential of myeloma must be thought of in elderly patients with pancytopenia as it can be easily diagnosed by bone marrow examination and quantitative serum protein electrophoresis.