Macroglossia Associated with Lymphangioma: Surgical Management of An Interesting Case
Tapan Nagpal1, Dixit Shah2, BS Manjunatha3, Amit Mahajan4
1 Professor, Department of Ear, Nose and Throat, Dheeraj General Hospital Sumandeep Vidyapeeth, Vadodara, Gujrat, India.
2 Senior Lecturer, Department of Oral and Maxillofacial Surgery, K.M. Shah Dental College and Hospital, Sumandeep Vidyapeeth, Vadodara, Gujrat, India.
3 Associate Professor, Department of Oral Anatomy and Histology, Faculty of Dentistry, Taif University, Kingdom of Saudi Arabia.
4 Professor, Department of Oral and Maxillofacial Surgery, K.M. Shah Dental College and Hospital, Sumandeep Vidyapeeth, Vadodara, Gujrat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. BS Manjunatha, Associate Professor, Faculty of Dentistry, Al-Hawaiya, Taif University, Taif, Kingdom of Saudi Arabia. E-mail : drmanju26@hotmail.com
Lymphangioma is considered as benign as well as a hamartomatous lesion of the lymphatic vessels that shows a marked predilection for the head and neck region. The most common site for intraoral lymphangiomas is the anterior two-thirds on the dorsal surface of tongue resulting in macroglossia. Such patients have a tendency of speech disturbances, poor oral hygiene, and bleeding from tongue following a trauma. A child with markedly enlarged tongue presents a unique challenge to the clinicians. Aesthetic, occlusal, functional and psychosocial problems may arise as a result of this condition. The indexed patient presented with an enlarged tongue. Wide excision of the lesion was done as a treatment.
Glossectomy, Hamartomatous, Large tongue, Swallowing
Case Report
A 15-year-old young boy was referred to the Department of Oral and Maxillofacial Surgery, KM Shah Dental College and Hospital, Vadodara, with a chief complaint of protrusion and increase in size of the tongue [Table/Fig-1a,b]. The patient was relatively asymptomatic and gave a history of trauma while playing in the ground 8 years back and resulted in injury to permanent lower incisors and a cut/nick on the tongue. Patient was immediately taken to a local hospital and was treated by suturing. Since then, the patient complains of increased in size with protrusion of tongue. Patient did not have any history of dysphagia, stridor, respiratory distress, nasal obstruction, nasal discharge or bleeding. Sleep and diet were normal. On examination, a diffusely enlarged tongue [Table/Fig-2] associated with anterior open bite was evident on palpation, the swelling was soft, non-tender and pebbly. The mouth opening was normal and there was slight restricted tongue movements. The speech was some what affected with open bite and incompetent lips mainly the lower lip. Hard tissue examination showed over-angulation of lower incisors with flattening of the alveolar ridge. A complete pre-operative blood analyses were within normal limits. ECG and chest X-ray were performed and appeared normal. A thorough history and physical examination were performed for congenital abnormalities such as Beckwith-Wiedemann syndrome, hypothyroidism commonly associated with macroglossia as one component.
Clinical photographs showing protrusion and enlargement of tongue (frontal and lateral views)

Photograph showing diffuse macroglossia associated with crenation and papillations on lateral border of tongue

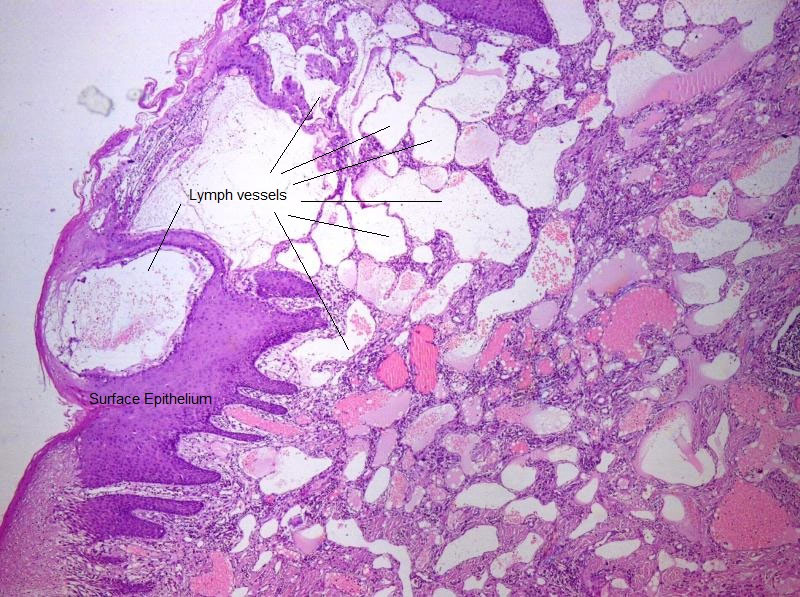
A magnetic resonance imaging (MRI) showed no morphological changes of tongue and revealed normal intensity with normal muscular structure and no defects in the salivary glands. The surgical treatment was explained to the patient and parents. After obtaining the informed written consent, a reduction glossectomy was performed, using a modified key hole wedge design [Table/Fig-3a&b]. This technique was chosen to obtain a reduction of tongue volume in three planes, preserving the vascular-nerve bundle. Tissue excised was sent for histopathological examination [Table/Fig-3c]. On microscopic examination, numerous large dilated spaces lined by endothelial cells mimicking lymph vessels filled with pale eosinophilic material close to the surface epithelium were noted [Table/Fig-4] and confirmed to be a ‘Lymphangioma’. One year postoperative follow up of patient had remarkable prognosis without any recurrence of lesion and good aesthetic enhancement and functions of the tongue [Table/Fig-5a&b]. (Presently, he is undergoing orthodontic treatment for mandibular prognathism and open bite.
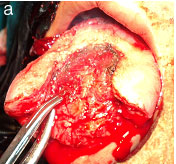

Photograph showing surgically excised tissue

Photomicrograph showing numerous large to small vascular spaces lined by endothelial cells mimicking lymph vessels
Photographs showing normal appearing tongue of 6th month follow-up without any recurrence (both frontal and lateral views)

Discussion
Lymphangioma is a rare congenital, hamartomatous malformation of the lymphatic vessels resulting from sequestration of lymphatic tissue that has retained its potential for growth and do not communicate with other lymphatic tissue [1,2]. A child with markedly enlarged tongue presents a unique challenge to the clinician. Lymphangioma lesions are non-tender or slightly painful in the initial stage. When lymphangioma manifests as macroglossia, interference with swallowing speech and respiratory difficulties are common, if left untreated [3]. Macroglossia is a non specific term, used in pediatrics to simply denote the presence of a ‘large tongue’ [4]. It may be produced by various processes and lymphangioma represent a group of special interest and significance among non infectious and non malignant nature [5].
The original description of lymphangioma was given by Virchow in 1854. The origin is considered to be congenital anomaly of the lymphatic system rather than a true neoplasm present as developmental malformations arising from sequestration of lymphatic tissue that do not communicate with the rest of the lymphatic channels [1]. In our case, the patient was relatively asymptomatic and noticed the lesion after the trauma eight years back. It is believed that embryologically, lymphangioma develops from five primitive buds developing from the venous system which include paired jugular sacs, paired posterior sacs and a single retroperitoneal sac.
Currently, it is debated that lymphangioma is a true neoplasm which results from transformed lymphatic endothelial cells, stromal cells or both [6]. Such patients tend to show speech disturbances, poor oral hygiene, and bleeding from tongue due to trauma [7].
Recently, Usha V et al., have reported a case of infantile lymphangioma having pebbly surface with other features. The patient should be evaluated thoroughly by proper history and physical examination, so as to rule out any syndrome associated with enlarged tongue as one component. The assessment should include complete examination of the tongue for any mass or change in color and consistency. If any complaints of chronic airway obstruction, pulmonary hypertension, subsequently, chest radiography and echocardiography are to be done. Computed tomography (CT) and magnetic resonance imaging (MRI) may be very useful radiological adjuvants to delineate soft tissues and to show the extent of tumors and other masses [8].
Surgical excision and radiation therapy are major treatment options and other methods such cryo therapy, electro-cautery, sclerosing with sclerosing agent, laser surgery and radio frequency tissue ablation technique are also used [7,9].
The type, size, involvement of anatomical structures and infiltration to the surrounding tissues are the important factors to be considered before deciding the treatment of lymphangioma [10]. Surgical excision is the preferred treatment and complete removal of intraoral lymphangioma mean complete removal of the affected organ [7]. The successful management of macroglossia requires a multidisciplinary approach. In our case, debulking of tongue under general anaaesthesia was performed with central wedge incision and suturing was done. Due to non encapsulated and “infiltrating” nature of the lymphangioma of tongue, complete removal is invariably impossible and recurrence is common. Sclerosing agents usually do not respond in cases of lymphangioma unlike haemangiomas. Surgical debulking of the tumor is, therefore the treatment of choice with objective of having a functional tongue. The prognosis is generally good for most patients [11].
Most case reports on macroglossia have indicated that surgery should be performed in early childhood and it is difficult to decide the right amount of reduction as the tongue grows continuously until preschool years [8,12]. Few reports have shown that a repeated tongue resection is needed for recurrent macroglossia [13]. Chronic cases of macroglossia have problems speech, swallowing and may affect the dentofacial skeleton. Several of methods of tongue reduction have been proposed to preserve the mobility and sensation of the tongue. In the case reported here, tongue reduction was planned to reduce aesthetic problems and improve the functional abilities after surgery. Postoperative findings showed that tongue reduction method is a successful treatment of choice for macroglossia.
Conclusion
Basically, lymphangioma is a disease of childhood dentist may be the first healthcare professional to come across. In such instance, preservation of taste, restoration of tongue size for articulation, correction of dental and mandibular deformities as well as cosmesis to be taken care of. Proper diagnosis and management, according to clinical evaluation of the patient may help improve the patient’s quality of life by reducing the functional and psychological disturbances including cosmetic disfigurement.
[1]. Morley SE, Ramesar KC, Macleod DA, Cystic hygroma in an adult: a case reportJ R Coll Surg Edinb 1999 44:57-58. [Google Scholar]
[2]. Bernnan TD, Miller AS, Chen S, Lymphangiomas of the oral cavity: A clinicopathologic, immunohistochemical and electron microscopic studyJ Oral Maxillofac Surg 1997 55:932-35. [Google Scholar]
[3]. Dinerman WS, Myers EN, Lymphangiomatous macroglossiaLaryngoscope 1976 86:291-96. [Google Scholar]
[4]. Morfit HM, Lymphangioma of the tongue. Treatment and appraisal of long-term resultsArch Surg 1960 81:761-67. [Google Scholar]
[5]. Rigg JP, Waldapfel R, Lymphangiomas of the tongueArch Otolaryngol Head Neck Surg 1940 31(6):966-73. [Google Scholar]
[6]. Yaita T, Onodera K, Xu H, Oya K, Histomorphometrical study in cavernous lymphangioma of the tongueOral Diseases 2007 13:99-104. [Google Scholar]
[7]. Guelmann M, Katz J, Macroglossia combined with lymphangioma: a case reportJ Cli Pediatr Dent 2003 27:167-70. [Google Scholar]
[8]. Mixter RC, Ewanowski SJ, Carson LV, Central tongue reduction for macroglossiaPlast Reconstr Surg 1993 91(6):1159-62. [Google Scholar]
[9]. Hartl DM, Roger G, Denoyelle F, Nicollas R, Triglia JM, Garabedian EN, Extensive lymphangioma presenting with upper airway obstructionArch Otolaryngol Head Neck Surg 2000 126:1378-82. [Google Scholar]
[10]. Usha V, Sivasankari T, Jeelani S, Asokan GS, Parthiban J, Lymphangioma of the tongue - a case report and review of literatureJ Clin Diagn Res 2014 8(9):ZD12-14. [Google Scholar]
[11]. Sunil S, Gopakumar D, Sreenivasan BS, Oral lymphangioma - Case reports and review of literatureContemp Clin Dent 2012 3(1):116-18. [Google Scholar]
[12]. Kaufman Y, Cole P, McKnight A, Hatef DA, Hollier L, Edmonds J, A modified keyhole technique for correction of macroglossiaPlast Reconstr Surg 2008 122(6):1867-69. [Google Scholar]
[13]. Morgan WE, Friedman EM, Duncan NO, Sulek M, Surgical management of macroglossia in childrenArch Otolaryngol Head Neck Surg 1996 122(3):326-29. [Google Scholar]