Transphyseal Injury of Distal Humerus: A Commonly Missed Diagnosis in Neonates
Sushma Malik1, Samruddhi R. Khopkar2, Charusheela Sujit Korday3, Shruti Sudhir Jadhav4, Atul R. Bhaskar5
1 Professor, Incharge Neonatology, Division of Neonatology, Department of Pediatrics, TN Medical College & BYL Nair Hospital, Mumbai, India.
2 Ex-Resident, Neonatology, Division of Neonatology, Department of Pediatrics, TN Medical College & BYL Nair Hospital, Mumbai, India.
3 Associate Professor, Neonatology, Division of Neonatology, Department of Pediatrics, TN Medical College & BYL Nair Hospital, Mumbai, India.
4 Assistant Professor, Neonatology, Division of Neonatology, Department of Pediatrics, TN Medical College & BYL Nair Hospital, Mumbai, India.
5 Consulting Pediatric Orthopaedic Surgeon, Division of Neonatology, Department of Pediatrics, TN Medical College & BYL Nair Hospital, Mumbai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sushma Malik, 3/7, Brady’s Flats, Sorab Bharucha Road, Colaba, Mumbai-400005, India.
E-mail: sushmamalik@gmail.com
Distal humeral physeal injury is a rare entity in newborns. Lack of ossific nuclei of the distal humerus in neonates results in a diagnostic dilemma as the injury is radiologically not visible and is often mistaken as elbow dislocation. Ultrasonography and Magnetic resonance imaging help to clinch diagnosis in the early period where plain radiographs fail to detect this entity. This condition warrants high index of suspicion along with good clinical acumen for early diagnosis and immediate management with closed reduction and immobilization to avoid long term complications. We present a case of delayed diagnosis of distal humeral physeal separation in a neonate which was managed conservatively at our neonatal intensive care unit with a good outcome without functional deformity.
Birth injury, Distal humeral physeal injury, Neonatal physeal injury
Case Report
A 24-year-old, primi gravida 35.4 weeks by dates with complete placenta previa was taken for emergency caesarean section in view of bleeding per vaginum and breech presentation. A male child weighing 1.510 kg was delivered who cried immediately after birth. At 18 hours of life the neonate was noticed to have swelling on right elbow with paucity of movements at right elbow joint. The distal finger movements, arterial pulsations and perfusion in that limb were well preserved. There was no bruising, ecchymosis or any history suggestive of external injury or fall. A plain anteroposterior radiograph and ultrasound of the local part of the baby on day one revealed only a soft tissue swelling around the right elbow joint [Table/Fig-1]. On day two of life a firm swelling was palpable at the distal end of humerus with painful restricted movements and muffled crepitus was heard. Other possible differentials of soft tissue swelling like traumatic injury, septic arthritis, swelling secondary to tight ligature of the identification band attached on the right upper arm and elbow or radial head dislocation were considered.
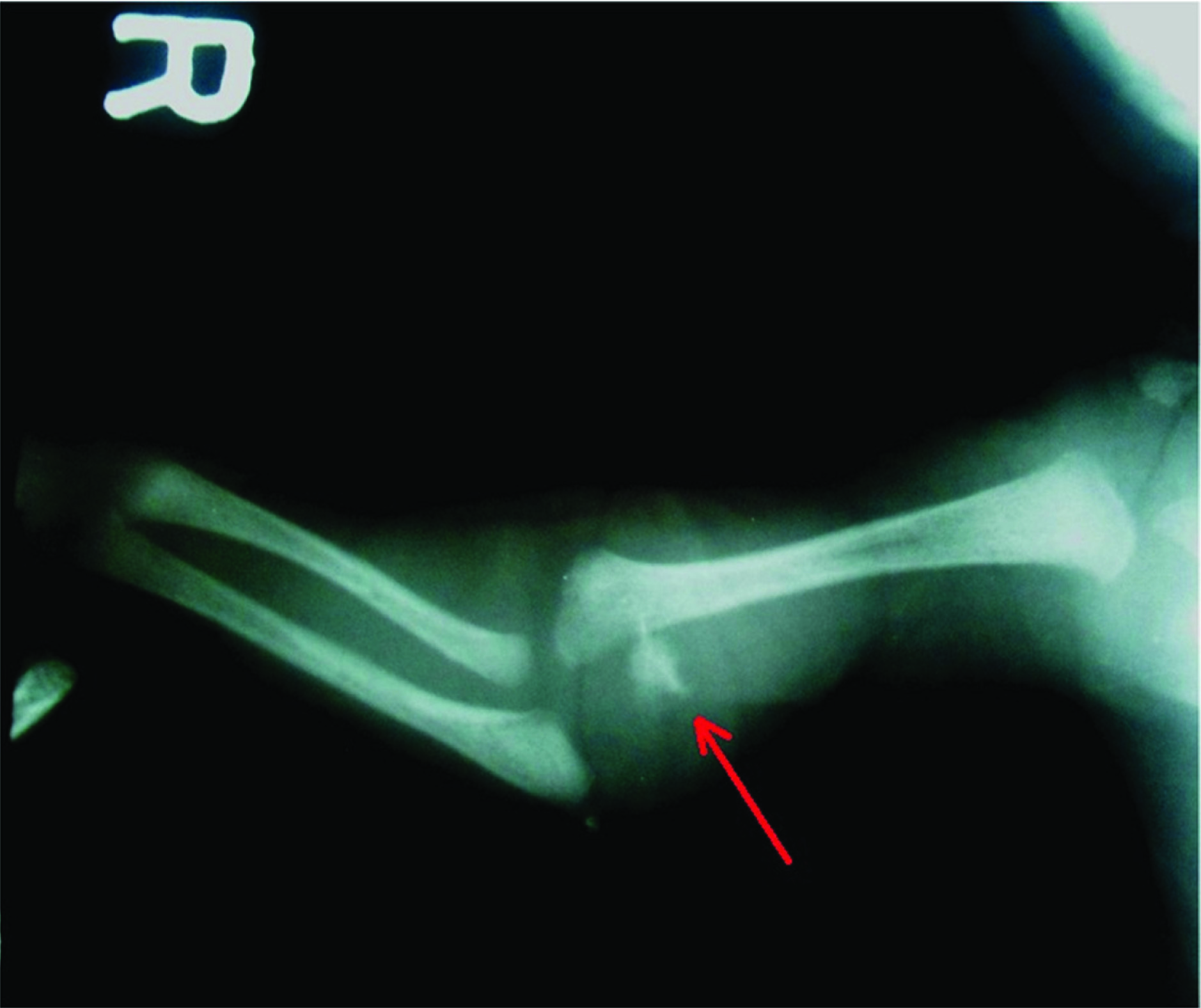
Radiograph on second day reveals postero-superomedial migration of both radius and ulna giving the spurious appearance of dislocation of right elbow

Repeat anteroposterior and lateral radiographs on day two of right elbow joint now revealed a posterosuperomedial migration of the radio-ulnar complex with dislocation of the elbow joint, without obvious evidence of fracture. The right elbow joint was splinted in 90 degrees flexion and semi-pronation to immobilize and reduce the elbow dislocation. After 14 days a repeat anteroposterior radiograph and ultrasonography showed a callus formation with transphyseal separation and postero-medial displacement of distal humeral physis thus clinching the diagnosis of distal physeal injury (Salter Harris Type II) in healing stage, which was initially erroneously diagnosed as elbow dislocation [Table/Fig-2]. Later, the splint was removed and the child was discharged with advice for regular follow up. On follow-up at two months, the right elbow radiograph revealed a re-modeled healed fracture without any displacement of bones. The child had a minor cubitus varus deformity with complete range of each movement at the right elbow joint with no limb shortening on the affected side.
Radiograph on day 14 shows callus formation due to distal humerus transphyseal separation (diagnosed on ultrasonography) and posteromedial displacement of radius and ulna
Discussion
Traumatic bone injuries occurring during birth are encountered in about 1 per 1000 live births [1]. Amongst long bone fractures, humerus, is the second commonest bone to be involved and fractures may occur in the shaft or in the epiphyseal regions [1,2]. Physeal injuries constitute about 20-30% of all childhood fractures and distal humerus physeal injury/ separation is uncommon and comprises 3.9% of these [3–5]. The risk factors for physeal injuries are difficult and instrumental deliveries, abnormal presentations, macrosomia and cephalopelvic disproportion. In our case, the neonate did not have history of birth trauma, child abuse or any obvious cause for the injury as against most of the previously reported cases, by Sherr Lurie N, Jacobsen S and Kaushal R, in which difficult labour or traction/ rotatory forces to the elbow was the cause for the injuries/ fracture [2,6,7].
Physeal injuries have been classified by Salter Harris into five types [5]. Type I injuries are characterized by a transphyseal plane of injury, with no bony fracture line through either the metaphysis or the epiphysis, type II injuries have fracture line extending from physis into metaphysis and type III injuries have fracture line extending from epiphysis into physis but not involving metaphysis. Type IV injuries have fracture line passing through the epiphysis, physis and metaphysis whereas type V injuries are compression fracture of the physis not involving the metaphysis or epiphysis. The outcome/prognosis depends more on the site of fracture rather than the Salter Harris classification.
Diagnosis of proximal and distal physeal injuries in neonates and at a young age is difficult before the ossification centres have Ossified, hence they are not visible on radiographs and therefore are often mistaken as dislocations [2]. Meticulous clinical examination can differentiate between elbow dislocation and distal humeral physeal fracture. In the distal humeral physeal injury the three point relationship between the olecranon process of ulna, the medial and the lateral condyle of humerus is maintained which is always disrupted in elbow dislocation [4]. However, the swelling and pain can restrict this assessment. Clinical findings of soft tissue swelling, pain and paucity of movements on affected side are consistently present in these cases, as was with our patient. Occasionally, a muffled crepitus is heard on passive movement of the joint and the fractured segments have a smooth contour due to the overlying physeal cartilage.
During assessment of the neonate it is imperative to also look for signs of radial and ulnar nerve palsy as reported by Kaushal R et al., [7]. Detailed examination of our child did not have any evidence of nerve injury. In a case series of six patients diagnosed with this fracture studied by Jacobsen S et al., the age of diagnosis varied from day one to thirty of life with majority being diagnosed late [6]. Our patient’s diagnosis was established on day 14 of life when radiograph/ ultrasound revealed callus formation, though clinically the child had presented on day one of life.
Radiographs generally fail to demonstrate the early physeal injury as neonates lack the ossification center in capetullum often giving the spurious appearance of elbow dislocation [4]. Postero-medial displacement of radio-ulnar complex has been a constant radiographical sign in almost all cases of transphyseal distal humeral fracture/separation injury, so was in our case too. Ultrasound of the elbow has emerged as an important modality that provides valuable information in demonstrating fractures, dislocations and physeal separations of the unossified cartilage especially when X-rays are inconclusive or ambiguous [2,8]. Ultrasonography has the advantage of being readily available, inexpensive, non-irradiating and non-invasive technique for early diagnosis [2,6,8,9]. However, it is highly operator dependent and can be painful and uncomfortable in the setting of fracture [4].
Arthrography can give good information about the cartilage damage and the visualisation of fracture but it is invasive and carries the risk of infection, hence, it is not advisable as routine investigation [7]. MRI of the elbow is the earliest and most accurate modality for diagnosing physeal injury. The need of anaesthesia to keep the baby still during MRI and its cost are the limiting factors [4].
The time of diagnosis and the type of fracture are crucial to decide the management of physeal injury. Closed reduction with splint immobilisation has been the treatment modality of choice for type I and type II physeal fractures if detected early [4,10,11]. However, if there is a delay in diagnosis or presentation, management is largely conservative in neonatal period [4]. The majority of type I and II injuries should not have attempted manipulation after 5 days. Type III, IV and V are very rare to occur at birth and often require open reduction and internal fixation and may require supracondylar osteotomy for cosmetic benefits at a later age [10,12].
Conclusion
Fracture separation of the distal epiphysis of the humerus is a rare birth trauma. The unimpressive clinical findings, difficult roentographic orientation due to invisible ossification nuclei, lack of knowledge and awareness of anatomical relationship of this entity often pose a diagnostic challenge in the neonates. A high index of suspicion along with diagnostic modalities of ultrasonography or magnetic resonance imaging help in their early detection and appropriate management.
[1]. Bhat VB, Kumar A, Oumachigui A, Bone injuries during deliveryIndian J Pediatr 1994 61:401-05. [Google Scholar]
[2]. Sherr-Lurie N, Bialik GM, Ganel A, Schindler A, Givon U, Fractures of the humerus in the neonatal periodIsr Med Assoc J 2011 13(6):363-65. [Google Scholar]
[3]. Baker A, Methratta ST, Choudhary AK, Transphyseal Fracture of the distal humerus in a neonateWest J Emerg Med 2011 12(2):173 [Google Scholar]
[4]. Soyuncu Y, Cevikol C, Soyuncu S, Yildirim A, Akyildiz F, Detection and treatment of traumatic separation of the distal humerus epiphysis in a neonate: a case reportUlus Travma Acil Cerrahi Derg 2009 15(1):99-102. [Google Scholar]
[5]. Lawrence W, Kriti S, John PD, Pediatric fracture patterns. In Kliegman RM, Stanton BF, St. Geme, Schor NF, Behrman RENelson textbook of paediatrics 2011 19th ednPhiladelphiaSaunders:2389-2390. [Google Scholar]
[6]. Jacobsen S, Hansson G, Nathorst-Westfelt J, Traumatic separation of the distal epiphysis of the humerus sustained at birthJ Bone Joint Surg Br 2009 91(6):797-802. [Google Scholar]
[7]. Kaushal R, Gupta PN, Gupta R, Bahadur R, Distal humeral epiphyseal separation associated with radial nerve palsy in a neonate as a result of birth traumaInjury Extra 2005 36:12-14. [Google Scholar]
[8]. Navallas M, Diaz-Ledo F, Ares J, Sanchez-Buenavida A, Lopez-vilchez MA, Solano A, Distal humeral epiphysiolysis in the newborn: utility of sonography and differential diagnosisClin Imaging 2013 37(1):180-84. [Google Scholar]
[9]. Dias JJ, Lamont AC, Jones JM, Ultrasonic diagnosis of neonatal separation of the distal humeral epiphysisJ Bone joint Surg Br 1988 70:825-28. [Google Scholar]
[10]. Barrett WP, Almquist EA, Staheli LT, Fracture Separation of the Distal Humeral Physis in the NewbornJ Pediatr Orthop 1984 4(5):617-19. [Google Scholar]
[11]. Princic J, Tonin M, Ales A, Birth trauma as the cause of fracture of the distal epiphysis of the humerus. A case reportUnfallchirurg 1995 98(9):487-88. [Google Scholar]
[12]. Carson S, Woolridge DP, Colletti TJ, Kilgore K, Pediatric Upper Extremity InjuriesPediatr Clin N Am 2006 53:41-67. [Google Scholar]