Altered Passive Eruption Complicating Optimal Orthodontic Bracket Placement: A Case Report and Review of Literature
Rohan Pulgaonkar1, Prasad Chitra2
1 Post Graduate Student, Department of Orthodontics, Army College of Dental Sciences, Secunderabad, India.
2 Professor and Head, Department of Orthodontics, Army College of Dental Sciences, Secunderabad, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rohan Pulgaonkar, Post Graduate Student, Department of Orthodontics, Army College of Dental Sciences, Secunderabad-500087, India. E-mail : dr.rohanpulgaonkar@gmail.com
An unusual case of altered passive eruption with gingival hyperpigmentation and a Class I malocclusion in a 12-year-old girl having no previous history of medication is presented. The patient reported with spacing in the upper arch, moderate crowding in the lower arch, anterior crossbite and excessive gingival tissue on the labial surfaces of teeth in both the arches. The inadequate crown lengths made placement of the orthodontic brackets difficult. Preadjusted orthodontic brackets have a very precise placement protocol which can affect tooth movement in all 3 planes of space if violated. The periodontal condition was diagnosed as altered passive eruption Type IA. Interdisciplinary treatment protocols including periodontal surgical and orthodontic procedures were used. The periodontal surgical procedures were carried out prior to orthodontic therapy and the results obtained were satisfactory. It is suggested that orthodontists should be aware of conditions like altered passive eruption and modalities of management. In most instances, orthodontic therapy is not hindered.
Bracket positioning, Crown lengthening, Depigmentation, Gingivectomy
Case Report
A 12-year-old female reported with a complaint of spacing between her upper front teeth. Additionally, she was conscious of dark gums in both arches on smiling [Table/Fig-1]. Examination revealed an Angle’s Class I malocclusion with midline diastema in the upper arch and moderate lower arch crowding. Teeth 21 and 31 were in crossbite with gingival recession seen with the lower incisor due to the trauma from occlusion [Table/Fig-2a&b].
Pre-treatment frontal smiling photograph

Pre-treatment intraoral photograph

Checking for presence of deep pockets

The diastema was on account of a thick maxillary labial frenum of the papillary penetrating variety. Both arches showed hyper pigmented gingivae with compromised smile aesthetics due to excessive gum show on smiling. A diagnosis of Altered Passive Eruption Type 1, Sub group A was made after thorough periodontal evaluation. Previous history taking revealed no drug usage which could have been a contributing factor. The case was complicated by the Altered Passive Eruption condition preventing placement of orthodontic brackets in their ideal positions.
A multidisciplinary approach to management was envisaged and included:
Initial gingivectomies in both arches to obtain sufficient crown lengths to enable orthodontic appliance placement and improve smile aesthetics.
Frenectomy of the thick maxillary labial frenum to enable diastema closure.
Depigmentation in both arches to improve gingival aesthetics.
Fixed orthodontic therapy to correct the malocclusion including diastema and crossbite.
Written informed consent was obtained prior to beginning procedures.
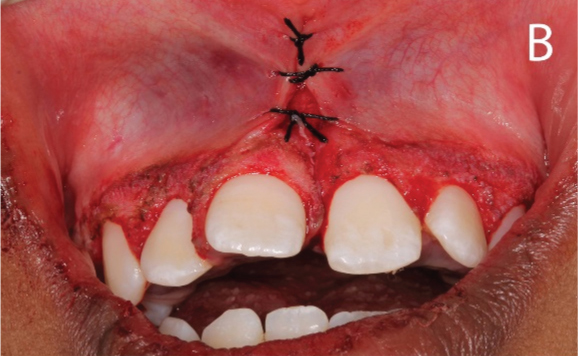
Treatment commenced with scaling and root planing a day prior to surgical procedures. The patient was put on chlorhexidine rinses three times daily for two weeks. Maxillary and mandibular acrylic stents were prepared in advance to enable accuracy during the gingivectomy procedure [Table/Fig-3a&b]. The surgical procedures were performed under local anaesthesia administered in the vestibular mucosa from the region of the 1st molar on one side to the other in both arches [Table/Fig-4a,b,5a,b]. The periodontal procedures (gingivectomy, depigmentation and frenectomy) were to be performed simultaneously to negate the need for repeated surgeries [Table/Fig-6a,b]. A soft tissue diode laser (Picasso, AMD Laser Technologies, USA) was used at the end on the operated sites to minimize bleeding and achieve haemostasis.

Mandibular surgical stent

Mandibular gingivectomy surgical incisions

Immediate postoperative view after mandibular surgery

Maxillary gingivectomy surgical incisions

Immediate postoperative view after maxillary surgery


Periodontal packs were placed on the operated surgical sites after completion of periodontal procedures and were left in place for a period of ten days [Table/Fig-6c]. Postoperative instructions regarding use of analgesics (ibuprofen), hygiene maintenance (chlorhexidine and saline rinses), brushing technique and food habits to be followed were given. The healing period was uneventful and the dressings were removed on the 10th postoperative day. The operated sites were then irrigated copiously with saline.
Coe-Pak placed after surgical procedures

There was a dramatic and marked improvement in the condition which was visible immediately [Table/Fig-7]. The crown lengths were now adequate to enable correct orthodontic bracket placement. The gingiva was a healthy pink with no scar tissue in the region of the frenectomy. The patient was satisfied with her gingival appearance and was encouraged to maintain good hygiene till the orthodontic appliances were placed.
Postoperative view 10 days after surgery

Two weeks later, the orthodontic fixed appliances were bonded in both arches (MBT 0.022 slot prescription). Brackets could be bonded in their specified positions to enable ideal tooth positioning. An initial phase of levelling, aligning and cross-bite correction was completed in three months time. The anterior crossbite correction ensured no further damage to the periodontium of the lower left central incisor. Records taken 6 months post-surgery show well aligned teeth with anterior crossbite corrected with no recurrence in the altered passive eruption condition anteriorly and posteriorly [Table/Fig-8a,b,c]. Orthodontic treatment progressed uneventfully with the patient in the space closure phase of therapy.
Initial bracket positioning with bite raised for cross-bite correction



Discussion
A variety of factors including teeth form/position and gingival tissue levels may influence overall smile aesthetics. Excessive gingival display, resulting in short clinical crowns, has been described in literature by several authors as “altered passive eruption (APE) [1,2]. This clinical situation has been attributed to failure in concluding the passive eruption phase.
Since treatment planning and management is different for active and passive phases of tooth eruption, surgical periodontal treatment, specifically crown lengthening, becomes imperative in patients requiring orthodontic therapy who present with altered passive eruption making placement of the brackets in predefined positions difficult. Types and management of altered passive eruption are listed in [Table/Fig-9] [3,4].
Classification & management of altered passive eruption [3,4]
| Type | Definition | Sub-Group | Treatment |
|---|
| Type I | The gingival margin is incisalor occlusal to the CEJ,and the mucogingival junctionis apical to the crest of bone.There is a wider gingivaldimension than generallyaccepted as the mean,as given by Bowers (1963)and Loe and Aniamo (1966). | Sub-Group AThe alveolar crestis located 1.5to 2 mmfrom the CEJ. | Gingivectomy |
| | Sub-Group BThe alveolar crestis coincidentwith the CEJ | Gingivectomy orscalloped inverse-beveled flap tothe CEJ, positioned(unrepositioned) flap,and osseous resection. |
| Type II | The gingival dimensionis normal. The free gingivalmargin is incisal orocclusal to the CEJand the mucogingivaljunction is positionedat the CEJ. | Sub-Group AThe alveolarcrest is located1.5 to 2 mmfrom the CEJ. | Apically positionedflap (repositioned flap) |
| | Sub-Group BThe alveolar crestis coincident withthe CEJ | Apically positionedflap with osseousresection. |
Numerous studies have in recent times detailed the need for lip repositioning procedures along with prosthetic rehabilitation of teeth to attain reduced gingival visibility and improve smile aesthetics [5–7]. Gingival depigmentation has also been established as an important tool in improving smile aesthetics [8].
Nart et al., studied the prevalence of altered passive eruption in orthodontically treated versus untreated patients and concluded that altered passive eruption is higher after orthodontic therapy but not to a significant level [9]. However, little is available in literature about management of cases with altered passive eruption and malocclusions mandating orthodontic intervention. These cases are especially hard to treat due to difficulty in accurate bracket positioning due to lack of clinical crown height and pose a challenge to orthodontists.
Altered passive eruption is a widely studied phenomenon, however, literature lacks clarity on treatment protocols to be followed when encountering such situations in patients requiring orthodontic treatment with fixed appliances. The incidence of this condition has not been fully studied in adults, although Volchansky and Cleaton- Jones, studied children aged between 6 and 16 years and found the incidence to be 12% [10] which reflects the rarity of the case reported here. AlpisteIllueca studied the mechanisms involved in the different types of altered passive eruption and also defined the morphology and dimensions for the same [11,12] which must be kept in mind while diagnosing and deciding the management protocols for such cases.
There is much confusion about timing of surgery for aesthetic crown lengthening in these cases, if at all planned, some stating that the gingivectomy should be performed after conclusion of orthodontic therapy to avoid a touch-up surgery at the end [13]. However, we found it impossible to bond orthodontic brackets in the patient without compromising on the biologic width of the teeth. In such situations, prior periodontal surgical procedures are advised initially to improve clinical crown heights and permit orthodontic appliance placement. We also acknowledge the importance of gingival depigmentation in selected cases as an established procedure in improving smile aesthetics and achieving higher levels of patient satisfaction.
However, caution should be exercised during orthodontic treatment to ensure that invasion of the biologic width of teeth is not compromised by placement of the brackets too gingivally. Residual composite resin around the bracket bases, which may cause chronic irritation of gingival tissues resulting in overgrowth, should be meticulously removed. It is interesting to note that studies implicating orthodontic treatment as a causative factor in altered passive eruption do not mention bracket positioning or invasion of biologic width due to residual composite resin around bracket bases.
Finally we acknowledge the possibility of recurrence of gingival overgrowth and gingival hyperpigmentation in some cases. Midline diastemas also have a high recurrence rate and permanent retention for the same was planned after completion of orthodontic therapy [14].
Conclusion
Altered Passive Eruption (APE) is a relatively uncommon finding in patients reporting for orthodontic treatment. Accurate diagnosis of the condition and its type is essential for management. The patient presented with a Class I malocclusion, spacing and altered passive eruption. The APE made orthodontic therapy difficult by hindering accurate appliance placement.
The case was managed with a combination of periodontal surgical (gingivectomy, frenectomy, depigmentation) and orthodontic procedures. Results obtained were good and the patient was highly satisfied with the aesthetic appearance. Gingivectomy enabled proper orthodontic appliance placement which was a prerequisite to successful correction of the malocclusion. Orthodontists should be aware of the possibility of such conditions occurring in a minority of patients reporting for treatment. Interdisciplinary management of these conditions most often leads to satisfactory results.
[1]. Miller PD, Allen EP, The development of periodontal plastic surgeryPeriodontol. 2000 1996 11:7-17. [Google Scholar]
[2]. Garber DA, Salama MA, The aesthetic smile: diagnosis and treatmentPeriodontol. 2000 1996 11:18-28. [Google Scholar]
[3]. Kurtzman GM, Silverstein LH, Diagnosis and treatment planning for predictable gingival correction of passive eruptionPract Proced Aesthet Dent 2008 20(2):103-8.quiz 110,121 [Google Scholar]
[4]. Coslet JG, Vanarsdall R, Weisgold A, Diagnosis and classification of delayed passive eruption of the dentogingival junction in the adultAlpha Omegan 1977 70(3):24-28. [Google Scholar]
[5]. Biniraj KR, Janardhanan M, Sunil MM, Sagir M, Hariprasad A, Paul TP, A combined periodontal - prosthetic treatment approach to manage unusual gingival visibility in resting lip position and inversely inclined upper anterior teeth: a case report with discussionJ Int Oral Health 2015 7(3):64-67. [Google Scholar]
[6]. Dayakar MM, Gupta S, Shivananda H, Lip repositioning: An alternative cosmetic treatment for gummy smileJ Indian Soc Periodontol 2014 18(4):520-23. [Google Scholar]
[7]. Gabric Panduric D, Blaškovic M, Brozovic J, Sušic M, Surgical treatment of excessive gingival display using lip repositioning technique and laser gingivectomy as an alternative to orthognathic surgeryJ Oral Maxillofac Surg 2014 72(2):404.e1-11. [Google Scholar]
[8]. Parwani S, Parwani R, Achieving better aesthetics by gingival depigmentation: report of three cases with a review of the literatureJ Mich Dent Assoc 2013 95(2):528-78. [Google Scholar]
[9]. Nart J, Carrió N, Valles C, Solís-Moreno C, Nart M, Reñé R, Prevalence of altered passive eruption in orthodontically treated and untreated patientsJ Periodontol 2014 85(11):e348-53. [Google Scholar]
[10]. Volchansky A, Cleaton-Jones PE, Delayed passive eruption – a predisposing factor to Vincent’s infection?J Dent Assoc S Afr 1974 29:291-94. [Google Scholar]
[11]. AlpisteIllueca F, Altered passive eruption (APE): a little-known clinical situationMed Oral Patol Oral Cir Bucal 2011 16(1):e100-04. [Google Scholar]
[12]. Alpiste-Illueca F, Morphology and dimensions of the dentogingival unit in the altered passive eruptionMed Oral Patol Oral Cir Bucal 2012 17(5):e814-20. [Google Scholar]
[13]. Robbins JW, Sequencing crown lengthening and orthodontic treatmentInside Dentistry 2010 5:54-57. [Google Scholar]
[14]. Morais JF, Freitas MR, Freitas KM, Janson G, Castello Branco N, Postretention stability after orthodontic closure of maxillary interincisor diastemasJ Appl Oral Sci 2014 22(5):409-15. [Google Scholar]