Ovarian Leiomyoma Along with Uterine Leiomyomata: A Common Tumour at an Uncommon Site
Indira Gunasekaran1, Manjiri Phansalkar2, Lal Bahadur Palo3, Renu G’Boy Varghese4
1 Post Graduate Student, Department of Pathology, PIMS, Puducherry, India.
2 Professor, Department of Pathology, PIMS, Puducherry, India.
3 Associate Professor, Department of Obstetrics and Gynaecology, PIMS, Puducherry, India.
4 Professor and Head, Department of Pathology, PIMS, Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Indira Gunasekaran, No: 19, 23rd Cross St, Avvai Nagar, Lawspet, Puducherry – 605008, India. E-mail : drindirag@gmail.com
Ovarian leiomyoma is one of the rarest benign tumours of the ovary, mostly seen in women of reproductive age group. Here we report a case of ovarian leiomyoma as an incidental finding in a patient of 38-year-old woman with uterine leiomyomata. Peroperatively, her left ovary appeared bulky & she underwent total abdominal hysterectomy with left salpingo-oophorectomy. Macroscopically, in addition to uterine leiomyomata, a grey-white solid mass was seen entirely within the ovary without any capsular breach. Microscopically, the ovarian mass resembled its uterine counterpart without any evidence of atypia or necrosis. Masson trichrome stain & immunohistochemistry for desmin positivity confirmed the smooth muscle origin of the tumour cells.
Despite its rarity, ovarian leiomyoma has to be considered as one of the differential diagnosis of ovarian spindle cell tumours. In difficult cases, immunohistochemistry aids the diagnosis.
Desmin, Ovary, Spindle cell tumour, Trichrome stain
Case Report
A 38-year-old woman (Para 1 Live 1) was admitted with complaints of mass per abdomen for past 1 month. Her past history was unremarkable with exception that she had a Copper T for past 13 years. Her mother also underwent hysterectomy for fibroid uterus.
On physical examination she was found to have fibroid uterus of 16 weeks size. Other laboratory findings were within normal limits. Transabdominal ultrasonography detected bulky uterus with multiple fibroids. Right ovary was within normal limits and the left ovary was not visualized.
Laparotomy was performed under epidural anaesthesia. Peroperatively, the left ovary was found to be bulky in addition to the multiple uterine fibroids. There were no adhesions. Right ovary and both tubes were unremarkable. Total abdominal hysterectomy with left salpingo-oophorectomy was performed & specimen was sent for histopathology.
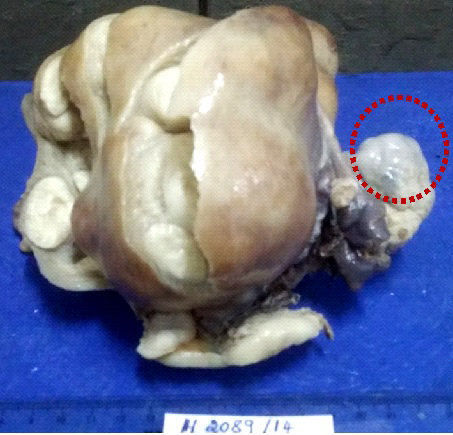
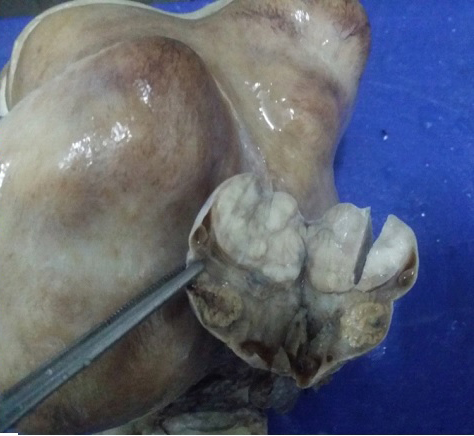
Grossly, uterus with cervix measured 15x11x5 cm. Outer surface of uterus was bulky & bosselated. Cut surface showed multiple intramural & subserosal fibroids. Left ovary measured 5.5x4x2.5 cm with a solid, firm, nodular mass which was distinctly separate from the uterus. Outer surface was smooth, cut section revealed a well circumscribed, grey white solid mass with lobulated appearance and measured 2.5 cm in diameter. This mass was found within the capsule of the ovary and the surrounding ovarian stroma was compressed. It was distinct from the uterine leiomyoma [Table/Fig-1,2].
Multiple uterine fibroids with distinctly separate ovarian mass
Cut section of ovary- well circumscribed mass seen within the ovarian stroma
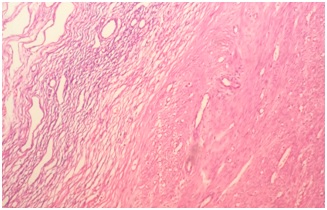
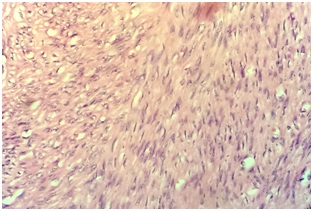
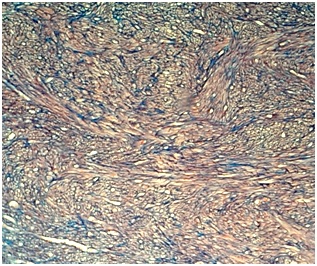
Microscopic examination of the ovarian mass revealed a well demarcated tumour surrounded by a rim of normal ovarian stroma. The tumour was composed of interlacing fascicles of spindle shaped cells with rod shaped bland nuclei interspersed with foci of collagen deposition. There was no evidence of any nuclear atypia or pleomorphism in the sections studied. Mitosis was very sparse [Table/Fig-3,4].
Tumour composed of interlacing fascicles of spindle shaped cells and surrounded by compressed ovarian stroma (H&E x 100)
Spindle cells with rod shaped blunt nucleus without atypia or pleomorphism (H&E x 400)
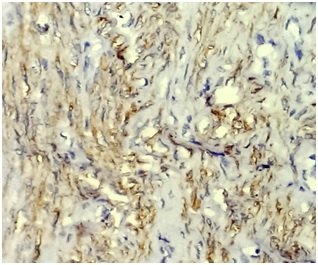
On Masson Trichrome, the tumour cells stained red in colour which indicated the smooth muscle nature of the spindle cells [Table/Fig-5]. Immunohistochemically, these spindle cells showed diffuse cytoplasmic positivity for desmin [Table/Fig-6].
On Masson Trichrome tumor cells stained red in colour. (Masson Trichrome x100)
Desmin showed diffuse cytoplasmic positivity. (Desmin x400)
Discussion
Ovarian leiomyoma was first described in the year 1862 by Sangalli [1] which is a rare tumour accounting for 0.5% to 1% of all the benign ovarian tumours [2,3]. Approximately 80 cases have been reported in literature till 2012 [4].
Ovarian leiomyomas are usually small and asymptomatic and in majority of the cases were discovered incidentally either during pelvic examination, at surgery or at autopsy [5–7]. Rarely in symptomatic cases, the presentations can vary from either abdominal pain, mass per abdomen, hydronephrosis, elevated CA-125, Meigs’ syndrome or polymyositis [8–10]. Most of them are usually unilateral, however few cases with bilateral involvement have been reported in paediatric/young adult groups particularly less than 35 years of age [3,11].
Histogenesis of ovarian leiomyoma is not yet well established, few studies state that they probably originate from smooth muscle cells in ovarian hilar blood vessel, cells in the ovarian ligament, smooth muscle cells or multipotential cells in the ovarian stroma, undifferentiated germ cells or cortical smooth muscle metaplasia of endometriotic stroma, smooth muscle present in mature cystic teratomas & smooth muscle in the wall of mucinous cystic tumour [7,12,13]. They often co-exist with uterine leiomyoma suggesting a common etiology or identical hormonal stimulation [9].
Both macroscopically and microscopically the tumour resembles their uterine counterpart [14].
The main differential diagnosis includes ovarian fibroma, thecoma, cellular fibroma, sclerosing stromal tumour, broad ligament leiomyoma extending into the hilum of ovary and pedunculated or wandering leiomyoma [15].
Agarwal et al., stated that ideally primary ovarian leiomyoma has to be entirely within the ovary with no similar lesions in the uterus or elsewhere [2]. However, many other authors noticed the co-existing uterine leiomyomas. A clinicopathological study on smooth muscle tumours of the ovary done by Lerwill MF et al., found 22 cases of ovarian leiomyoma, out of which 12 cases were associated with uterine leiomyomas with histological features similar to that of their uterine counterparts [14].
Another study done by Doss BJ et al., on fifteen cases of ovarian leiomyomas, found out that about 78% of cases were associated with uterine leiomyomas [12]. In the present study, it was found within the ovary and was completely encircled by the ovarian capsule, not adherent to the uterus or salphinx.
Microscopically, the tumour needs to be differentiated from fibroma which is comprised of bundles of spindle shaped cells with pointed nuclei and often exhibit storiform pattern rather than the fascicular pattern. Masson Trichrome helps to distinguish smooth muscle cells from fibrous tissue. Other differential is cellular thecoma comprised of lipid laden theca cells in a fibrous stroma, in which the tumour cells are stained with oil red O.
Immunohistochemistry is confirmatory in doubtful cases especially desmin, α-SMA (Alpha-Smooth Muscle Actin) and inhibin helps in differentiating leiomyomas from fibromatous tumour. Diffuse desmin positivity for tumour cells favours leiomyomas over fibromatous tumours, which are typically negative or may show focal positivity. SMA is often positive in both these tumours hence it is not helpful in differentiating the both. Thecomas are strongly positive for α-inhibin and does not express SMA. In the present study, masson trichrome staining & desmin positivity on IHC confirmed the smooth muscle origin of the tumour cells [8].
Leiomyoma also needs to be differentiated from the leiomyosarcoma by considering features such as mitotic activity, tumour necrosis and cytological atypia.
Conclusion
Despite its characteristic morphology, they need to be distinguished from other benign tumours like ovarian fibroma, thecoma, sclerosing stromal tumour, and broad ligament leiomyoma extending into the hilum of ovary, pedunculated or wandering leiomyoma. In such cases, extensive sampling and immunohistochemistry aids in arriving at a definitive diagnosis.
[1]. Tsalacopoulos G, Tiltman AJ, Leiomyoma of the ovary- report of three casesS Afr Med J 1981 59:574 [Google Scholar]
[2]. Agarwal R, Kumar M, Agarwal L, Agarwal KK, A huge primary ovarian leiomyoma with degenerative changes: an unusual presentationJ Clin Diagn Res 2013 7(6):1152-54. [Google Scholar]
[3]. Tomas D, Lenicek T, Tuckar N, Puljiz Z, Ledinsky M, Kruslin B, Primary ovarian leiomyoma associated with endometriotic cyst presenting with symptoms of acute appendicitis: a case reportDiagnostic Pathology 2009 4:25 [Google Scholar]
[4]. Sharma S, Valiathan M, Kumar P, Ovarian leiomyoma- rare tumour with unusual presentations: Report of 2 cases with brief review of literatureIJCRR 2014 6(15):28-32. [Google Scholar]
[5]. Lema VC, Massinde AN, Rambao PF, Ndaboine E, Matovero D, Rumanyika RN, Bizarre presentation of bilateral ovarian leiomyoma: a case reportTanzan J Health Res 2013 15(4):1-5. [Google Scholar]
[6]. Usta U, Karadag N, Turkmen E, Haltas H, Primary leiomyoma of the ovaryTrakya Univ Tip Fak Derg 2006 23(1):39-42. [Google Scholar]
[7]. Patne SCU, Kumar M, Raghuvanshi S, Agarwal NR, Unilateral primary ovarian leiomyoma with degeneration masquerading as ovarian malignancyWorld J Surg Res 2013 2:50-53. [Google Scholar]
[8]. Rajabi P, Hani M, Bagheri M, Mirzadeh F, Large ovarian leiomyoma in young womanAdv Biomed Res 2014 3(1):88 [Google Scholar]
[9]. Pandit MJ, Watson NR, Mackenzie IZ, Leiomyoma of the ovaryJ Obstet Gynaecol 1997 17:503-04. [Google Scholar]
[10]. Choi SY, Park JS, Lee JW, Kim BG, Bae DS, A rare case of primary ovarian leiomyoma with atypical Meigs’ syndromeKorean J Obstet Gynecol 2012 55(4):285-89. [Google Scholar]
[11]. Taskin MI, Ozturk E, Yildirim F, Ozdemir N, Inceboz U, Primary ovarian leiomyoma: A case reportInt J Surg Case Rep 2014 5(10):665-68. [Google Scholar]
[12]. Doss BJ, Wanek SM, Jacques SM, Qureshi F, Ramirez NC, Lawrence WD, Ovarian leiomyomas: clinicopathologic features in fifteen casesInt J Gynecol Pathol 1999 18:63-68. [Google Scholar]
[13]. Kataria SP, Chawla N, Singh G, Kum S, Ovarian leiomyoma associated with serous cystadenoma – a case report of an uncommon entityGlobal J Pathol Microbiol 2014 14(4):38-42. [Google Scholar]
[14]. Lerwill MF, Sung R, Oliva E, Prat J, Young RH, Smooth muscle tumours of the ovary: A clinicopathologic study of 54 cases emphasizing prognostic criteria, histologic variants, and differential diagnosisAm J Surg Pathol 2004 28:1436-51. [Google Scholar]
[15]. RamalakshmiPullela V B, Das S, Chunduru B, Dua S, A case of ovarian leiomyoma with cystic degenerationIndian J Pathol Microbiol 2009 52:592-94. [Google Scholar]