Morning Glory Disc Anomaly, A Report of a Successfully Treated Case of Functional Amblyopia
Humberto Cavazos-Adame1, Abraham Olvera-Barrios2, Alejandro Martinez-Lopez-Portillo3, Jesus Mohamed-Hamsho4
1 Professor and Head of the Pediatric Ophthalmology and Strabismus Clinic, Department of Ophthalmology, University Hospital “Dr. Jose Eleuterio Gonzalez”, Faculty of Medicine. Universidad Autonoma de Nuevo Leon, Mexico.
2 Opthalmology Resident, Department of Ophthalmology, University Hospital “Dr. Jose Eleuterio Gonzalez”, Faculty of Medicine. Universidad Autonoma de Nuevo Leon.
3 Professor, Glaucoma and Optic Nerve Diseases Clinic, Department of Ophthalmology, University Hospital “Dr. Jose Eleuterio Gonzalez”, Faculty of Medicine. Universidad Autonoma de Nuevo Leon, Mexico.
4 Chief of the Department, Professor and Head of the Glaucoma and Optic Nerve Diseases Clinic, Department of Ophthalmology, University Hospital “Dr. Jose Eleuterio Gonzalez”, Faculty of Medicine. Universidad Autonoma de Nuevo Leon, Mexico.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Humberto Cavazos-Adame, Departamento de Oftalmologia, Hospital Universitario “Dr. Jose Eleuterio Gonzalez”, Universidad Autonoma de Nuevo Leon, Ave. Francisco I. Madero and Gonzalitos s/n, Colonia Mitras Centro, Monterrey, Nuevo Leon, Mexico C.P. 64460.
E-mail: drhcavazos@gmail.com
Morning Glory Disc Anomaly (MGDA) is a congenital malformation of the optic nerve characterized by the presence of a funnel-shaped macropapilla with neuroglial remnants in its center surrounded by an elevated and pigmented chorioretinal ring. Its incidence is rare and no gender predisposition has been found. Associated conditions like strabismus lead to an early diagnosis.
We report the case of a 3.8-year-old boy with amblyopia of the right eye (count fingers 0.3 meters) due to MGDA. Correction of the refractive error with glasses, along with occlusive therapy resulted in a visual acuity of 20/100 after a five-year follow up.
The presence of amblyopia in these cases demands an early management oriented to improve the visual acuity. Every patient with an anatomical malformation diagnosed during the period of sensory maturation should be treated with occlusive therapy and followed on a regular basis to diagnose associated conditions such as retinal detachment.
We recommend occlusive therapy in every patient diagnosed with MGDA or in any patient with unilateral or asymmetric structural abnormalities that could lead to amblyopia. This 5-year case follow-up provides additional evidence of the importance of treatment during the period of amblyopia reversibility.
Morning glory disc syndrome, Optic nerve dysplasia, Organic amblyopia, Relative amblyopia, Strabismus
Case Report
A 3.8-year-old male Hispanic premature newborn of 34 weeks of gestation of a primigravida with a birth weight of 2.260 kg was brought by his mother to the outpatient ophthalmology clinic with a 3 year-history of a deviated right eye. There was no relevant family history.
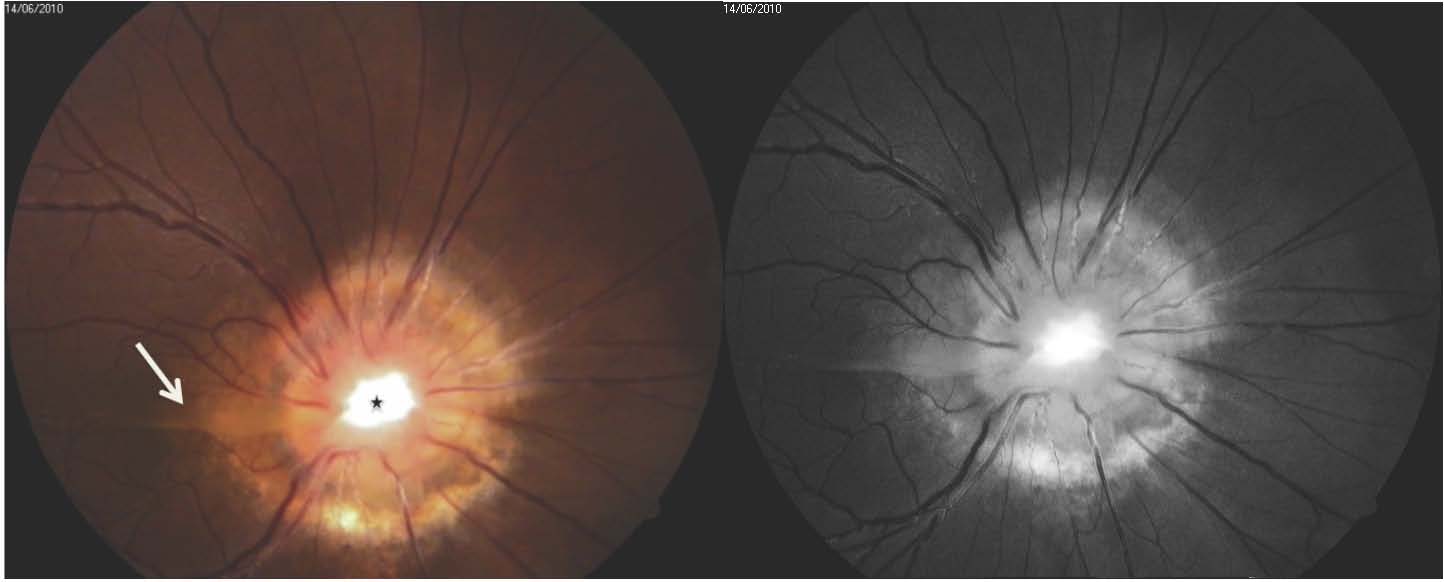
Visual acuity evaluated with figures was count fingers (CF) at 30 cm in the right eye (OD) and 20/30 in the left eye (OS). Cycloplegic refraction with cyclopentolate revealed OD: E +1.50 C -1.75 x 05 and OS: E +1.50 C -0.50 x 175. The Hirschberg corneal reflex test showed an exotropia of the right eye. Pupillary reflex testing showed a relative afferent pupillary defect on the right eye. Anterior segment biomicroscopy was normal for both eyes and an intraocular pressure of 11mmHg was recorded for each eye. Fundoscopic examination under mydriasis revealed a pallid and enlarged right optic disc with a funnel-like excavation that included rests of fibroglial tissue in its center. Retinal vessels abnormally augmented in number that emerged radially from the peripheral papilla like bicycle wheel spokes. A peripapillary chorioretinal pigmented ring with macular capture was also identified [Table/Fig-1]. No data of retinal detachment were found on the peripheral retina. Fundoscopic exam of the left eye was unremarkable. Neither facial abnormalities, nor signs or symptoms that could orient to the diagnosis of basal encephalocele or any other neurological disorder were found.
A Colour (left) and red free (right) photograph of the right optic nerve. The distinctive characteristics of MGDA can be seen: a prominently excavated macropapilla with a glial tuft in its center (asterisk), peripapillar chorioretinal pigmentation and the presence of macular capture temporal to the optic disc (arrow).
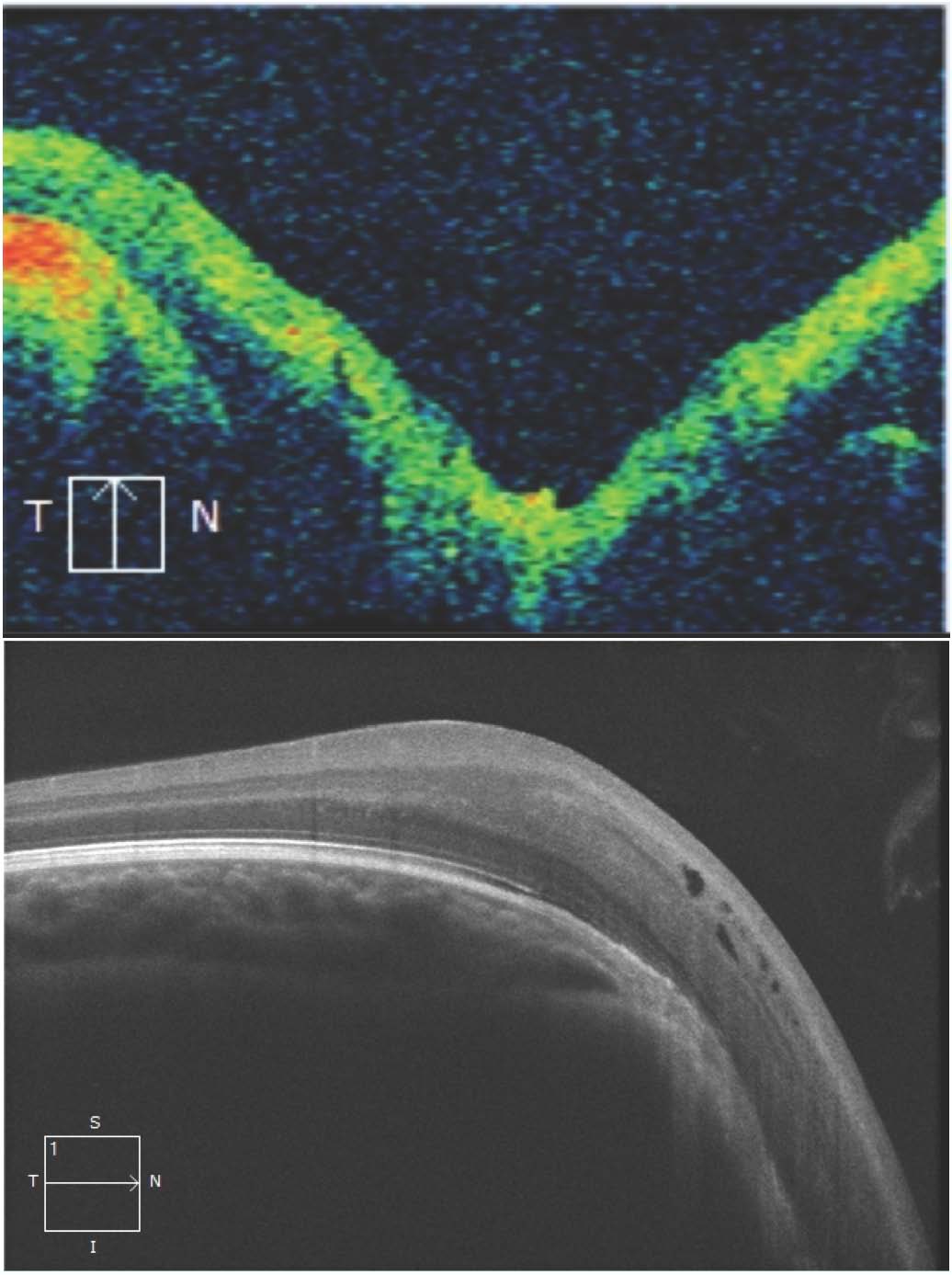
An MRI of the brain without contrast was normal and visually evoked potentials showed no abnormalities for the age group. Evaluation of the optic nerve and macula by means of Optical Coherence Tomography Imaging recorded the funnel shape configuration of the optic disc, a uniform retinal pigment epithelial layer, foveal aplasia and no signs of retinal detachment [Table/Fig-2]. During follow up, kinetic perimetry testing at age 8 demonstrated an enlarged blind spot of the right visual field [Table/Fig-3]. Correction of the refractive error with glasses (OD: E+1.50 C-1.50 x 5, OS: E+1.00 C-0.50 x 175) as well as occlusion therapy for 1 month with close follow-up were prescribed to our patient. Occlusion rhythm was adjusted according to the evolution. Gradual improvement of vision was evidenced, with best-corrected visual acuity (BCVA) of CF at 2 meters at age 5, 20/400 at age 6, 20/200 at age 7 and 20/100 on his latest visit at age 9. A small right 15 prism diopter exotropia remained.
Optical coherence tomography (OCT) of the optic nerve (Up) confirms the increased dimensions of the optic nerve, its funnel-shaped excavation and an increased retinal nerve fiber layer that does not follow the typical ISNT pattern. Macular OCT (Down) showing foveal aplasia and pericystic spaces near the excavation of the optic nerve
Goldmann perimetry of the right eye demonstrating an enlarged blind spot and the abscence of isopters 1, 2 and 3.

Discussion
The current report presents the five-year follow-up results in BCVA of a patient with organic amblyopia due to Morning Glory Disc Anomaly (MGDA) that improved with occlusive therapy. The MGDA is an optic nerve dysplasia that characteristically consists of the presence of an enlarged papilla with a central funnel shaped excavation, retinal blood vessels that abandon the papilla in a radial fashion to continue in a straight course and a variable degree of peripapillary pigmentation [1]. Kindler integrated the morphological characteristics of the anomaly into a syndrome, which he named after the morning glory flower due to its resemblance with the optic papilla. The pathogenesis is unknown. A hypothesis is that the anomaly is due to a poor development of the lamina cribrosa and the posterior sclera. Mutations in the PAX 6 gene have recently been identified in these patients [2].
As a result of refractive errors, poor visual acuity and/or comitant strabismus that usually accompany MGDA, the diagnosis is usually made early. A prevalence of 2.6/100 000 has recently been reported [3]. It usually presents as a non-hereitable unilateral malformation, with no gender predisposition and a median age of diagnosis of 2 years [4]. It is common to find relative afferent pupillary defects, such as the Marcus Gunn Pupil [5], and visual field defects like an enlarged blind spot (both present in our patient) as well as central or paracentral scotomas, or hemianopsia [1]. Serous retinal detachments, palpebral haemangioma, cataract, and myopia magna can also be seen [6–9]. Strabismus is present in up to 90% of the patients [1]. The visual acuity can range from CF to 20/200 in the affected eye with just about 30% of the patients reaching a visual acuity of 20/40 or better [4]. Only the presence of a big posterior scleral staphyloma, calcifications, or both, has been associated with poor visual acuity [4]. Neither of which was found in our patient.
The high prevalence of amblyopia in these cases can significantly worsen the vision and by cause of the also frequent refractive errors; cycloplegic refraction should be carried out in every patient with MGDA.
Organic amblyopia refers to the decrease of visual acuity in one or both eyes that is associated with an anatomical abnormality [10]. It has been classically described that organic amblyopia is irreversible, but a superimposition of irreversible and reversible amblyopia can be found in these patients; the so-called relative amblyopia of Bangerter or functional amblyopia [11]. Although standard visual acuity cannot be restored in patients with both types of amblyopia, occlusive therapy still plays an important role in the visual rehabilitation [6]. Evidence has shown that occlusion therapy for patients with unilateral, asymmetrical or severe structural abnormalities of the optic nerve results beneficial to the visual acuity [3,12,13]. In a recent study that included 12 patients with MGDA, a median improvement of 0.03 (range 0.025-0.090 decimal notation) in the BCVA in 3 of 6 patients that were treated with occlusion therapy was demonstrated [3]. Similarly, Loudot et al., reported a case of a 2.5-year-old girl who improved her visual acuity after 1 year of occlusive therapy from 1/10 Rossano 1/20 to 7/10 Rossano 1/2 [12].
Our case differs to what has been classically described in the literature of organic amblyopia showing a noticeable improvement in the BCVA of this patient from CF at 30cm (20/8000) to 20/100 in a 5-year follow-up period. As this case illustrates, the existence of an optic nerve malformation, afferent pupillary defect or foveal aplasia should never discourage the amblyopia treatment. A previous report showed that patients with MGDA and foveal aplasia can reach better BCVA than patients with MGDA and normal maculae [3]. A specialization of cones in the absence of a foveal pit could be the responsible for this [14]. Our report supports and highlights the importance of occlusive therapy along with optical correction in patients with MGDA. Additional data to the long term BCVA of these patients is provided. Systemic associations such as craniofacial midline defects (hypertelorism, cleft lip, basal encephalocele, corpus callosum agenesis), endocrine abnormalities with compromise of the pituitary gland as well as cerebrovascular anomalies are also relevant [1,5,15]. Therefore, proper vascular imaging studies along with a multidisciplinary management of the patients have to be considered.
Conclusion
The MGDA is a relatively rare optic disc malformation that can often be associated with severe visual disturbances. Because the condition manifests almost always unilaterally and the mean age of diagnosis is in the sensitive period of visual maturation, we recommend optical correction and occlusion therapy, as supported by our BCVA result. A correct diagnosis is also of a paramount importance due to many systemic associations that call for a multidisciplinary evaluation. Despite the absence of specific treatment for the anomaly, the correct intervention in these patients age group can make a difference in their future.
[1]. Lee BJ, Traboulsi EI, Update on the morning glory disc anomalyOphthalmic Genet 2008 29(2):47-52. [Google Scholar]
[2]. Azuma N, Yamaguchi Y, Handa H, Mutations of the PAX6 gene detected in patients with a variety of optic-nerve malformationsAm J Hum Genet 2003 72(6):1565-70. [Google Scholar]
[3]. Ceynowa DJ, Wickström R, Olsson M, Morning Glory Disc Anomaly in childhood - a population-based studyActa Ophthalmol 2015 :1-9. [Google Scholar]
[4]. Harasymowycz P, Chevrette L, Décarie JC, Morning glory syndrome: clinical, computerized tomographic, and ultrasonographic findingsJ Pediatr Ophthalmol Strabismus 2005 42(5):290-95. [Google Scholar]
[5]. Quah BL, Hamilton J, Blaser S, Morning glory disc anomaly, midline cranial defects and abnormal carotid circulation: an association worth looking forPediatr Radiol 2005 35(5):525-28. [Google Scholar]
[6]. Brodsky MC, Congenital optic disk anomaliesSurv Ophthalmol 1994 39(2):89-112. [Google Scholar]
[7]. Brodsky MC, Wilson RS, Retinal arteriovenous communications in the morning glory disc anomalyArch Ophthalmol 1995 113(4):410-11. [Google Scholar]
[8]. Leitch RJ, Winter RM, Midline craniofacial defects and morning glory disc anomaly. A distinct clinical entityActa Ophthalmol Scand Suppl 1996 (219):16-19. [Google Scholar]
[9]. Cañete Campos C, Gili Manzanaro P, Yangüela Rodilla J, Retinal detachment associated with morning glory syndromeArch Soc Esp Oftalmol 2011 86(9):295-99. [Google Scholar]
[10]. Noorden GK, Mechanisms of amblyopiaAdv Ophthalmol 1977 34:93-115. [Google Scholar]
[11]. Mimura O, Inui T, Kani K, Retinal sensitivity and spatial summation in amblyopiaJpn J Ophthalmol 1984 28(4):389-400. [Google Scholar]
[12]. Loudot C, Fogliarini C, Mancini J, Rehabilitation on functional amblyopia in Morning Glory SyndromeJ Fr Ophtalmol 2007 30(10):998-1001. [Google Scholar]
[13]. Lengyel D, Klainguti G, Mojon DS, Does amblyopia therapy make sense in eyes with severe organic defects?Klin Monbl Augenheilkd 2004 221(5):386-89. [Google Scholar]
[14]. Marmor MF, Choi SS, Zawadzki RJ, Visual insignificance of the foveal pit: reassessment of foveal hypoplasia as fovea planaArch Ophthalmol 2008 126(7):907-13. [Google Scholar]
[15]. Lenhart PD, Lambert SR, Newman NJ, Intracranial vascular anomalies in patients with morning glory disk anomalyAm J Ophthalmol 2006 142(4):644-50. [Google Scholar]