Schwanomma From Cervical Sympathetic Chain Ganglion – A Rare Presentation
A. Affee Asma1, E. Kannah2
1 Professor, Department of General Surgery, Rajiv Gandhi Government General Hospital, Chennai, India.
2 Junior Resident, Department of General Surgery, Rajiv Gandhi Government General Hospital, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. E. Kannah, 28, Nallanna Street, Royapettah, Chennai-600014, India. E-mail : kannahmmc@gmail.com
Schwanommas arising from cervical sympathetic chain are tumours that are rare in occurrence. These lesions are usually difficult to differentiate from a vagal schwanomma and a carotid body tumour during the initial workup. In this report, a rarely seen huge cervical sympathetic chain schwanomma case with partial Horner’s syndrome is being presented in detail, which to our known knowledge, is one of the few cases reported in literature.
Horner’s syndrome, Magnetic resonance angiogram, Ptosis, Splaying
Case Report
A 31-year-old male patient presented with complaints of swelling in the neck for the past 7 months which was insidious in onset gradually progressive in nature associated with dysphagia and otalgia. Patient had no other known history of co-morbid illness. He was a smoker and alcoholic for 20 years. On examination patient had a firm mobile 9 x 7 cm ellipsoidal swelling situated in the left side of neck extending from lower border of mandible to 3cm above clavicle with the lower border made out [Table/Fig-1a-c]. Medially the swelling extended 2cm from midline into the posterior triangle deep to sternocleidomastoid with the carotid pulsations felt superficially over the swelling. Examination of the eyes showed ptosis of eyelid.
(a) posterior extent of the swelling; (b) anterior extent of the swelling; (c) lateral view of the swelling

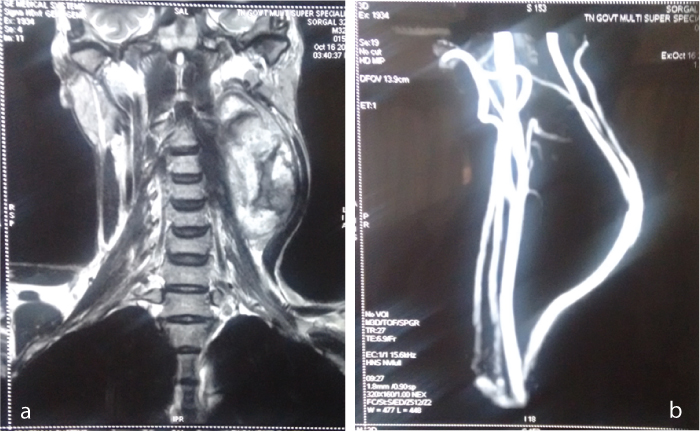
Initial workup of blood and radiological investigations were carried out. Magnetic Resonance Imaging (MRI) neck revealed a large lobular mixed intense space occupying lesion in left upper neck extending from retropharyngeal space to thyroid level indenting over posterior left submandibular gland and displacing the sternocleidomastoid laterally as shown in [Table/Fig-2a]. Magnetic Resonance Angiogram (MRA) revealed anterolateral displacement and splaying of internal and external carotid arteries involving mild compression with a discernible feeder from superior thyroid artery as shown in [Table/Fig-2b]. Fine needle aspiration cytology (FNAC) and the core cut results were inconclusive. Video directed laryngoscopy was normal except for a small soft buldge in the lateral pharyngeal wall on the left side.
MRI and MRA picture of the patient: a) 5.2x6.4 cm heterogeneously enhancing soft tissue density lesion with central non-enhancing areas noted in the left carotid space extending into the parapharyngeal space, b) swelling in the left carotid space pushing the carotids anterolaterally
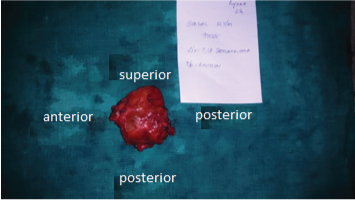
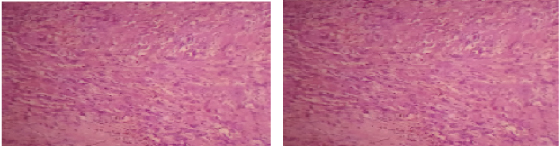
After explaining the risks of surgery patient was taken up for excision of the mass. Under general anaesthesia sjogren’s cervical neck incision was made and subplatysmal flaps raised. After preserving the marginal mandibular nerve carotid sheath on the left side was identified. The contents of the carotid sheath were splayed by the swelling. After careful meticulous dissection these structures were preserved and the swelling was excised completely [Table/Fig-3]. Swelling was found to be densely adherent to the left pyriform sinus and pharynx which was overcome with careful dissection. Then the wound was closed in layers after keeping a suction drainage. Postoperative period was uneventful. Ptosis of eyelid in the postoperative period is shown in [Table/Fig-4] and the histopathology suggested a benign schwanomma with cystic degeneration as shown in [Table/Fig-5].
Gross specimen showing the schwanomma excised completely with the capsule
Patient with ptosis of eyelid in the postoperative period

Histopathology showing features of schwanomma
Discussion
Schwanommas are painless, benign and slow growing tumours. It was first described by Verocay in the year 1908 followed by Antoni in the year 1920 who gave classical histopathological description of these tumours. Schwanommas are uncommon tumours that arise from any peripheral, cranial or autonomic nerves. Though they have a wide distribution, approximately 45% are located in the head and neck region. Cervical schwanommas being an uncommon lesion, those arising from cervical sympathetic chain are very rare, only 60 cases being reported in literature until now. Similar complaints were noted in a 42-year-old Italian male in 2005 who developed ptosis only postoperatively. Schwanommas of cervical sympathetic chain occur in the age group of 5-77 years with no sex predilection. No predisposing factors have been identified till date. Though they are asymptomatic about 10 cases have been reported with Horner’s syndrome before excision [1–6]. Here in this case the patient presented with partial Horner’s syndrome i.e. ptosis of eyelid.
It is very important and difficult to differentiate various swellings arising from the parapharyngeal space from a schwanomma arising from the cervical sympathetic chain. These swellings are classified depending on the site of origin from pre-styloid and post-styloid compartments. Differential diagnosis of masses arising in the pre- styloid compartment includes lipomas, parotid tumours, lymphadenopathy and certain neurogenic tumours. Post-styloid compartment pathologies include carotid artery aneurysms, neurogenic tumours involving cranial nerves IX through XII, as well as the sympathetic chain and paragangliomas arising from the vagus nerve or carotid body [4,7,8]. Fine needle aspiration, while conclusive in many cases of neck masses, is much less valuable for the compact neural tumours [9,10].
Imaging studies play a major role in differentiating these tumours. Computed Tomography (CT) which was initially the gold standard is now replaced by MRI. It is essential to differentiate carotid body tumour, cervical sympathetic chain ganglion schwanomma and a vagal schwanomma. Splaying of carotid bifurcation with hypervascularity usually denotes a carotid body tumour. Cervical sympathetic chain ganglion splays carotid bifurcation without hypervascularity. On the other hand a vagal schwanomma doesn’t cause any splaying and do not splay the internal and external carotid arteries like a cervical sympathetic chain ganglion schwanomma [2,3,11–13].
Surgical resection is recommended for cervical sympathetic chain ganglion. It gives excellent result with no local recurrence. It is well tolerated but the patient is forced to develop partial or complete Horner’s syndrome [14,15]. There has been no conclusive evidence to show that neural grafting is an efficacious procedure [16].
Conclusion
To sum up cervical sympathetic ganglion schwanommas are rarely encountered in clinical practice and such lesions may present as an asymptomatic neck mass or with Horner’s syndrome as in our case. These schwanommas require surgical excision with the patient developing partial or complete Horner’s syndrome which must be explained before surgery.
[1]. Das Gupta TK, Brassfield RD, Strong EW, Hadju SI, Benign solitary Schwannomas (neurilemomas)Cancer 1969 24:355-66. [Google Scholar]
[2]. Souza JW, Williams JT, Dalton ML, Solis MM, Schwannoma of the cervical sympathetic chain: It’s not a carotid body tumourAm Surg 2000 66:52-5. [Google Scholar]
[3]. Ganesan S, Harar RP, Owen RA, Dawkins RS, Prior AJ, Horner’s syndrome: a rare presentation of cervical sympathetic chain schwannomaJ Laryngol Otol 1997 111(5):493-95. [Google Scholar]
[4]. Callum EN, Neurinoma of cervical sympathetic chainBr J Surg 1950 37(1):17 [Google Scholar]
[5]. Politi M, Toro C, Cian R, Costa F, Robiony M, Horner’s syndrome due to a large schwannoma of the cervical sympathetic chain: report of a caseJ Oral Maxillofac Surg 2005 63:707-10. [Google Scholar]
[6]. Bocciolini C, Dall’olio D, Cavazza S, Laudadio P, Schwannoma of cervical sympathetic chain: assessment and managementActa Otolaryngeal Ital 2005 25(3):191-94. [Google Scholar]
[7]. Cullen TH, Monro RS, Cervical neurofibroma in the differential diagnosis of carotid body tumourBr J Surg 1952 39:454-57. [Google Scholar]
[8]. Rogers L, Neurinomas of the cervical sympathetic system with report of a caseBr J Surg 1953 40:579-80. [Google Scholar]
[9]. Wang CP, Hsiao JK, Ko JY, Splaying of the carotid bifurcation caused by a cervical sympathetic chain schwannomaAnn Otol Rhinol Laryngol 2004 113(9):696-99. [Google Scholar]
[10]. Colreavy MP, Lacy PD, Hughes J, Bouchier-Hayes D, Brennan P, O’Dwyer AJ, Head and neck schwannomas—a 10 year reviewJ Laryngol Otol 2000 114(2):119-24. [Google Scholar]
[11]. Myssiorek DJ, Silver CE, Valdes ME, Schwannoma of the cervical sympathetic chainJ Laryngol Otol 1988 102:962-65. [Google Scholar]
[12]. Rosner M, Fisher W, Mulligan L, Cervical sympathetic schwannoma: case reportNeurosurgery 2001 49(6):1452-54. [Google Scholar]
[13]. Takimoto T, Katoh H, Umeda R, Parapharyngeal schwannoma of the cervical sympathetic chain in a childInt J Pediatr Otorhinolaryngol 1989 18:53-58. [Google Scholar]
[14]. Valentino J, Boggess MA, Ellis JL, Hester TO, Jones RO, Expected neurologic outcomes for surgical treatment of cervical neurilemomasLaryngoscope 1998 108:1009-13. [Google Scholar]
[15]. Panneton JM, Rusnak BW, Cervical sympathetic chain schwannomas masquerading as carotid body tumoursAnn Vasc Surg 2000 14(5):519-24. [Google Scholar]
[16]. Wax MK, Shiley SG, Robinson JL, Weissman JL, Cervical sympathetic chain SchwannomaLaryngoscope 2004 114:2210-13. [Google Scholar]