Fractures are one of the most common causes of morbidity. Clinical suspicion is an important prerequisite for the study as transient oedema syndromes may also occur and hence clear history of trauma increases the accuracy by localizing the suspected location of injury and imaging of the specific part concerned has to be done [1]. Developing a short and specific trauma protocol would be ideal for reducing the time for performance of scan and for a cost effective approach. Patients with high clinical suspicion of fracture but no injury demonstrated on plain radiograph were subjected to MR Imaging because of the ability of MRI changes related to acute injury and its ability to differentiate acute from chronic injury [2]. MRI has become imaging modality of choice for identifying occult fractures for which correct early diagnosis is essential such as femoral neck fractures, scaphoid fractures and paediatric elbow injuries [2].
To determine the MRI imaging patterns in recent bone injuries (less than 4 weeks) following negative or inconclusive plain radiographs and to demonstrate the efficacy of MRI over conventional radiography in the detection of occult fractures.
Materials and Methods
MRI 1.5 TESLA PHILIPS ACHIEVA 16 channel machine equipped with FLEX, Torso XL and spine coils provided by manufacturer were used. Prospective cross-sectional study with descriptive analysis was done on 75 patients with clinical suspicion of fracture but could not be diagnosed by conventional radiography. Both men and women of all age groups with recent injuries of less than 4 weeks duration were included. However, patients with obvious conventional radiographic evidence of fracture or injuries of more than 4 weeks duration were excluded from the study. Also patients with splinter injuries, metallic implants and cardiac pacemakers were excluded as these were contraindications to MRI. The following sequences were taken : (1) T1 SE: repetition time (TR) - 450 ms; echo time (TE) - 20 ms; slice thickness - 3 mm; (2) STIR/PD FATSAT : repetition time (TR) - 4560 ms; echo time (TE) - 80 ms; slice thickness - 3 mm. Field of view (FOV) and Matrix are adjusted for the part to be scanned. Time for acquisition: (3-4 minutes). Both the sequences were taken in the same plane either coronal or sagittal or axial. Additional sequences in the other plane were taken if necessary. Data analysis was done using Rates, Ratios and Percentages.
Results
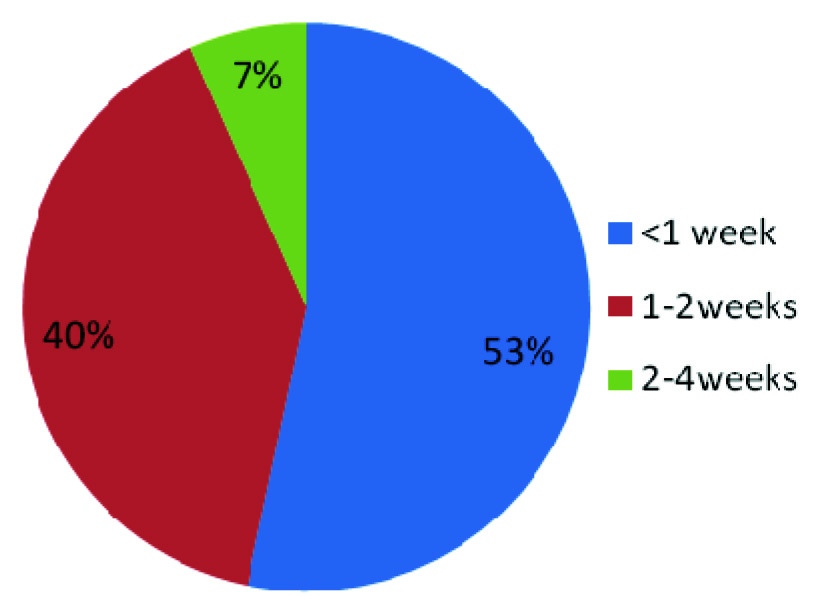
In the present study the youngest person was of age 8 years and the eldest was of age 83 years. Mean age was 33 years (Range, 8 – 83years). [Table/Fig-1] shows sex distribution of the study group. Thus an overall male predominance of 54(72%) was noted. [Table/Fig-2] shows distribution of study group by duration of injury.
Sex distribution of study group
| Sex | Number of Cases(n = 75) | Percentage |
|---|
| Male | 54 | 72% |
| Female | 21 | 28% |
Pie-Chart showing distribution of study group by duration from injury
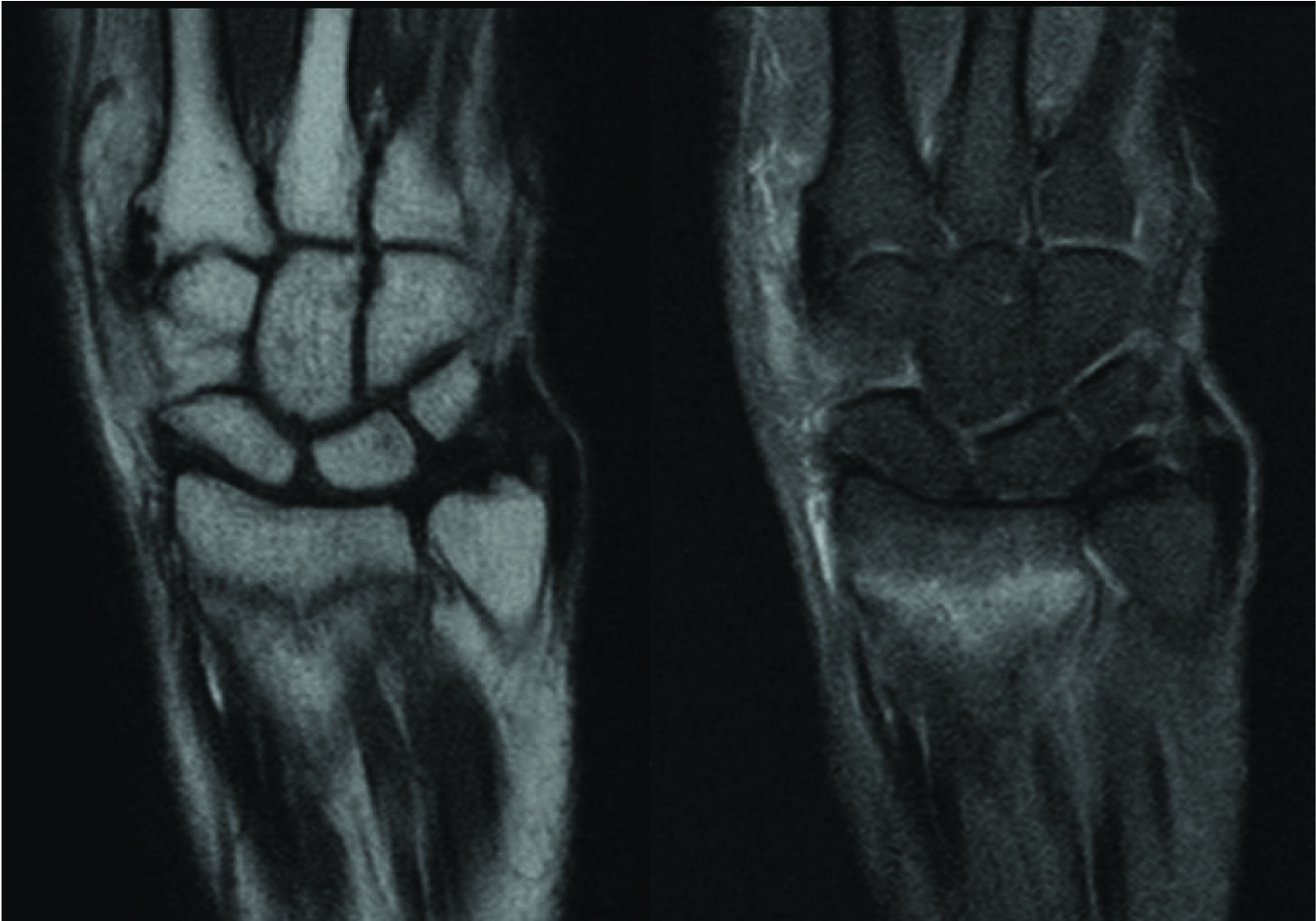
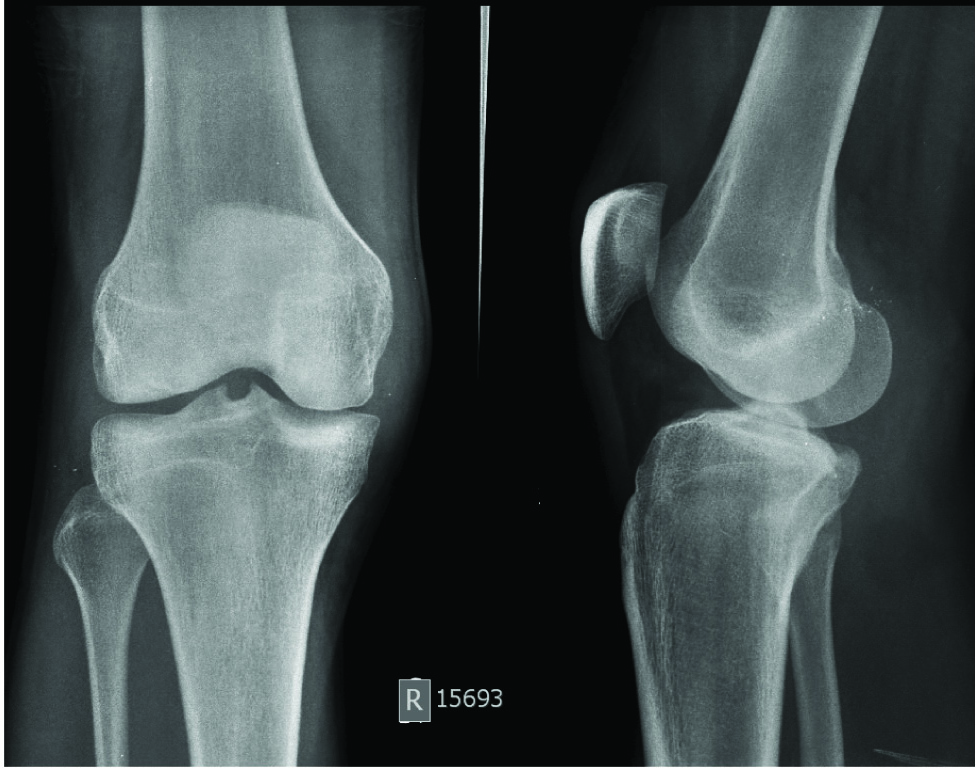
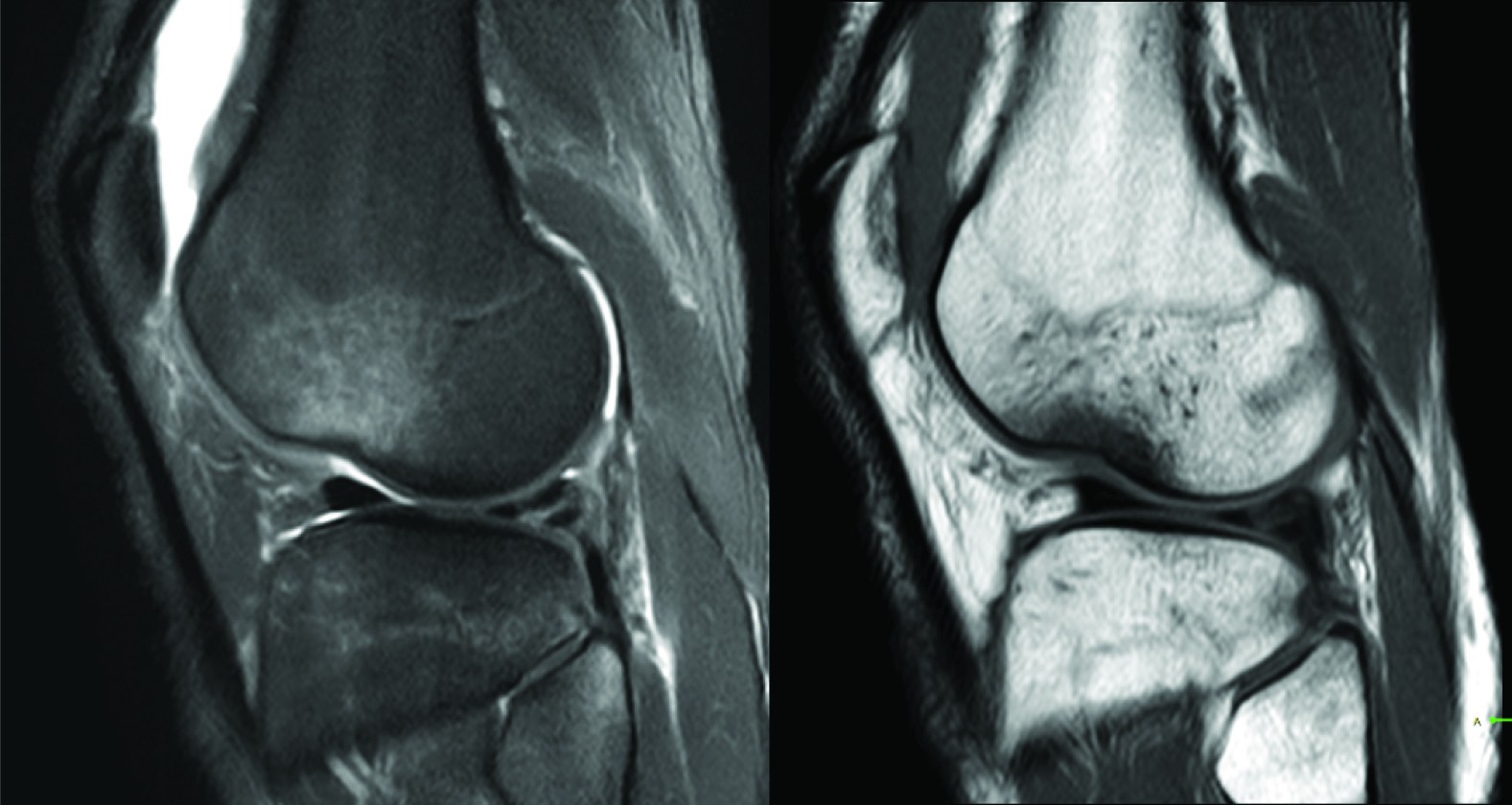
Distribution of cases by bony injury is represented in [Table/Fig-3] which demonstrates that knee is most common joint to be involved followed by wrist and ankle. Bony contusions were noted in about half the cases (52%). This was the commonest abnormality detected in our study. [Table/Fig-4] shows different injury patterns observed in the study. Fracture line was demonstrated in 16 patients (21%). Thus fractures were missed in a significant number of patients on radiography (about 1 in 5). [Table/Fig-5] shows occult fracture in radius bone which was identified on MRI scan. Similar occult fracture in forth metatarsal can be noted in [Table/Fig-6]. [Table/Fig-7] shows an MRI with bony contusion which was missed in radiography. The remaining 20 patients (27%) did not show any obvious injury to the bone on even MR imaging, however soft tissue injury could be demonstrated in 12 (16%) patients which shows that the extent of soft tissue injury was relatively well demonstrated by MR imaging. Soft tissue injury in the form of ligamentous injury was commoner in knee and ankle whereas muscular injury was more common in shoulder, hip, elbow and wrist. However, this was not statistically significant. We also observed that specific areas of bony contusions and fractures were commoner in particular ligamentous injury as for example contusion/fracture in lateral tibial plateau associated with Anterior Cruciate Ligament (ACL) tear which is a well known fact. Association of fracture/contusion of posterior tibial articular surface and Posterior Cruciate Ligament (PCL), postero lateral corner of tibia and arcuate ligament was noted. However, large studies dedicated to knee joint in particular are further required before forming a hypothesis. A normal MRI with no obvious injuries either of bones or soft tissues was seen in only 8 cases (11%). Such low number of normal MRI suggests that although radiographically negative, clinical symptoms should form a basis for referring patients to further imaging like MRI.
Distribution of cases by bony injury
| Part | No of Cases | Bone InjuryDemonstrated onMRI (Fracture Lineor Marrow Oedema) | No Bony InjuryDemonstrated onMRI |
|---|
| KNEE | 17 (23%) | 15 | 2 |
| WRIST | 15 (20%) | 10 | 5 |
| ANKLE | 15 (20%) | 10 | 5 |
| FOOT | 7 (9%) | 6 | 1 |
| ELBOW | 6 (8%) | 5 | 1 |
| LEG | 5 (7%) | 2 | 3 |
| HAND | 4 (5%) | 2 | 2 |
| HIP | 3 (4%) | 3 | 0 |
| SPINE | 3 (4%) | 2 | 1 |
| TOTAL | 75 (100%) | 55 | 20 |
Distribution of cases by injury pattern
| Total no of cases | Fracture | Bone contusion(+/- Fracture) | No bony injury |
|---|
| 75 | 16 (21%) | 39(52%) | 20(27%) |
| Soft tissue injury without Bony injury | Normal MRI |
| 12(16%) | 08(11%) |
(a) Plain radiographs of a 55 year old patient with trauma to right wrist lateral and PA views showing no obvious bone injury. (b) T1 WI and PD SPIR MR images in coronal plane demonstrate a linear hypointense signal with surrounding oedema at the distal right radius suggestive of fracture

(a) Plain radiographs of a 42 year old patient with trauma to right foot, AP and Oblique views showing no obvious bone injury. (b) T1 WI and PD Fat Sat MR images in coronal plane demonstrate a linear hypointense signal at the base of fourth metatarsal with surrounding oedema suggestive of fracture


(a) Plain radiographs of an 18 year old patient with trauma to right knee AP and Lateral views showing no obvious bone injury. (b) T1 WI and PD Fat Sat MR images in sagittal plane demonstrates bone marrow oedema involving lateral condyles of both right femur and tibia and proximal end of fibula suggestive of contusions. No obvious fracture is demonstrated. Suprapatellar joint effusion is demonstrated well
Discussion
It has been recognized that CT and MR imaging are useful diagnostic tools for the evaluation of patients who have experienced trauma, and these imaging modalities are frequently used before surgical interventions [3].
“Occult fracture” is used for a fracture that is either radiographically unapparent or demonstrates subtle abnormalities that are missed at initial interpretation [4]. These fractures also are hidden from view on direct observation during arthroscopy. Occult bone injuries are heterogeneous group ranging from diffuse trabecular involvement to localized injury contiguous with subchondral plate or articular surface. Fractures are identified when a low signal linear lesion in spin echo T1 weighted images is surrounded by a large area, of poorly defined, bone marrow oedema is present [5].
“Bone contusions” are injuries of traumatic origin which include bleeding, infarction, and oedema caused by microscopic compression fractures of cancellous bone [1]. Fat suppression in PD FATSAT and STIR images allows homogenous background suppression of fat signals and displays changes like bone marrow oedema very clearly which can be easily interpreted [3].
As the patients included in the study had a clear history of trauma, the diagnosis of stress fractures is excluded which by definition do not involve significant trauma and result from unusual physical activity or only repetitive mechanical forces.
Multidetector row CT offers excellent spatial resolution and multiplanar reformation capabilities [6–9]. The advantages of multidetector CT include short imaging time, isotropic data sets, and the ability to reconstruct multiplanar reformatted images retrospectively in any arbitrary plane [8]. Its advantages over conventional radiology include a more precise depiction of fracture lines and depressed or distracted articular surfaces and better assessment of bone loss [10]. However, the ability of even CT has been debatable as it cannot identify bone marrow contusions and soft tissue injuries accurately. Also, CT involves high doses of radiation and thus cannot be used for serial follow ups. Hence search for a better alternative has brought MRI to the forefront and its advantages over the former two have been a topic of research.
The multiplanar imaging capability, improved contrast resolution and ability to discriminate different types of tissue [11] afforded by MR imaging make it ideal for the detection of fractures undetected by radiographs [3]. Furthermore, MR imaging is the most sensitive direct imaging technique for depicting injury to the microtrabeculae and their environs [5,12]. This diagnostic method is indicated for stress fractures, avulsion or hidden fractures [13]. The ability of MRI to delineate the soft tissues and its better resolution is a proven fact. It is easily tolerated even in the older patients and its absent radiation dosage are some of its potential advantages. Its cost effectiveness is well appreciated when compared to the unnecessary health care costs and morbidity the patient has to undergo due to delayed diagnosis and helps in early institution of treatment. Magnetic resonance (MR) imaging is thus an excellent means of evaluating the musculoskeletal system for the presence of soft-tissue and bone abnormalities after trauma [14]. However, the limitations of MRI with respect to contraindications in patients with splinter injuries, metallic implants and cardiac pacemakers should be considered.
In the setting of trauma, radiographically occult osseous injuries are frequently identified at MR imaging as areas of poorly marginated signal intensity alteration (decreased signal intensity with T1-weighted sequences increased signal intensity with T2- weighted sequences, or both) in the cancellous bone and marrow. This appearance is thought to represent areas of haemorrhage, oedema, or hyperaemia secondary to trabecular injury [15,16]. There is increased bone marrow oedema resulting in intraosseous STIR hyperintensity in acute fractures [17]. Cortical changes are however more obvious on fat suppressed PD, T2 weighted or STIR sequences, MRI of the musculoskeletal system [18].
These osseous injuries may result from a direct blow to the bone, compressive forces of adjacent bones impacting one another, or traction forces that occur during an avulsion injury [19].
In addition, while examining the clinical MR images of different joints for internal derangement, radiologists may encounter unsuspected fractures [4]. These fractures could be radiographically unapparent or demonstrate subtle abnormalities that are overlooked easily.
The pattern of bone marrow oedema is like a footprint left behind at injury [20]. By studying the distribution of the oedema, one can understand the mechanism of injury that occurred and thereby predict with accuracy the associated soft-tissue abnormalities that may be present.
The present study is comparable to Pierre-Jerome et al., Gufler H et al., Bretlau et al., Where fracture and contusion percentages were almost similar as noted in [Table/Fig-8] [21–23].
Present study is compared to Pierre-Jerome et al., Gufler H et al., Bretlau et al., [20–22]
| Pierre-Jeromeet al., (2010)[21] | Gufler Het al., (2013)[22] | Bretlauet al.,(2002) [23] | Present study |
|---|
| Fracture | 37.1 % | 34.8% | — | 21 % |
| Contusions | 63 % | 82.6% | 56 % | 52 % |
At present, there are few studies describing the role of MRI in traumatic injuries, particularly the soft tissues. Many such studies are localized to a specific part or joint of the body. The present study was undertaken to assess the efficacy of MRI at various parts of the body, to observe the pattern of bony injury, to determine the locations at which bony injuries may be occult on conventional radiography and to identify frequency of lesions at individual parts.
Clinical significance of occult bone injuries is that they may be the only abnormalities explaining patient’s symptoms without need for surgical procedures [24]. Weight bearing should be avoided to prevent compressions of bone in areas of trabecular fractures and collapse of damaged overlying articular cartilage that may then lead to pain or premature osteoarthritis [24,25]. Associated soft tissue injuries can also be assessed [24].
One of the major advantages of MRI is the excellent ability to depict associated soft tissue injuries. The soft tissue injuries can be characterized as injuries to the muscles, tendons and ligaments and graded as per the lesions. These include muscle oedema, haematoma, partial muscle tear, or complete muscle tear.
Acute muscle injuries have associated oedema and haemorrhage that cause prolongation of the T1 and T2 relaxation times of the injured tissue.
Any confined area of altered signal within or outside the muscle fibers can be identified as a haematoma. A haematoma may show varying signal intensities on both T1- and T2-weighted images, depending on the evolving state of haemoglobin.
There are two major MR findings in an acute muscle tear: 1) deformity of the muscle; and 2) presence of high signal intensity on oedema-sensitive series due to blood and oedema. When muscle strain occurs, there is bleeding and oedema at the site of the injury. In an incomplete tear, blood and oedema often infiltrate between muscle bundles and produce a feathery appearance.
The location of the injuries at the musculo-tendinous junction is defined by the “feather-like” pattern of oedema. This pattern of oedema is characteristic of a muscle strain. Partial tears at the musculo-tendinous junction are more common than complete tears, which tend to occur at the tendon-bone interface.
Ligament injuries can be graded into 3 grades [18].
Grade 1 - Microscopic tears
Grade 2 - Partial tears
Grade 3 - Complete tears.
Conclusion
Thus we conclude that such high number of abnormalities found in radiologically occult patients can be explained by the fact that only those patients who were presenting with clinical symptoms like pain, tenderness and restriction of movements etc. were subjected to MRI.
The typical MR imaging findings of occult fracture are intraosseous speckled or linear regions of low signal intensity on T1-weighted MR images and irregular areas of high signal intensity in corresponding areas on fluid-sensitive MR imaging sequences. Emphasis is also made on the joints where the bony injuries are frequently occult on plain radiographs and where MR imaging is helpful, i.e. particularly the knee, wrist, ankle, and foot.
Its cost effectiveness is well appreciated when compared to the unnecessary health care costs and morbidity the patient has to undergo due to delayed or in accurate/alternative diagnosis. The findings of the present study guided the change in treatment plan of the patient.
MR imaging has high sensitivity and specificity in detecting occult fractures and remains the reference standard for early diagnosis of occult fractures.