SNAPPE-II (Score for Neonatal Acute Physiology with Perinatal Extension-II) in Predicting Mortality and Morbidity in NICU
Shivanna Sree Harsha1, Banur Raju Archana2
1 Assistant Professor, Department of Paediatrics, Sri Siddhartha Medical College, Tumkur, Karnataka, India.
2 Assistant Professor, Department of Microbiology, Sri Siddhartha Medical College, Tumkur, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shivanna Sree Harsha, Assistant Professor, Department of Pediatrics, Sri Siddhartha Medical College, Tumkur, Karnataka-527107, India. Email: drsriharsha@gmail.com
Introduction
A number of illness severity scores have evolved which would predict mortality and morbidity in intensive care units. One such scoring system developed by Richardson was SNAPPE-II (Score for Neonatal Acute Physiology with Perinatal extension-II).
Aim
The present study was conducted to assess the validity of SNAPPE-II score as a predictor of mortality and morbidity.
Materials and Methods
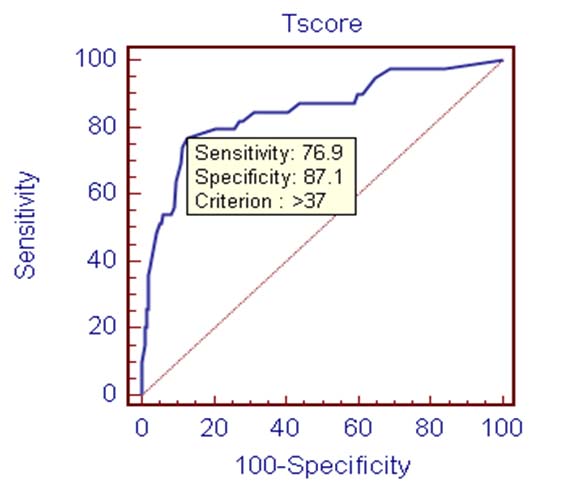
A total of 248 neonates who met the inclusion criteria were included in the study and SNAPPE-II score was calculated. Receiver Operating Characteristic (ROC) curve was constructed to derive the best cut-off score and SPSS package (Statistical Package for the Social Sciences) was used for statistical analysis.
Results
SNAPPE-II score was higher among expired neonates compared to survived ones. A mean score of 37 was associated with higher mortality. However, it didn’t accurately predict the length of stay.
Conclusion
SNAPPE II score is a better predictor of mortality irrespective of gestational ages and it is not a good predictor of morbidity.
Illness severity, Length of stay, Neonate, Scoring systems
Introduction
Advances in the neonatal intensive care have significantly increased survival and decreased mortality and morbidity among neonates admitted to the Neonatal Intensive Care Unit (NICU). There are however, significant variations in practices and outcomes among NICUs [1–3]. Routinely available markers of risk such as birth weight, gestational age, and sex do not adequately capture dimensions of illness severity and do not explain such a variation. In Pediatric ICUs and NICUs this problem has been addressed by the use of prognostication scoring systems. The Score for Neonatal Acute Physiology (SNAP) developed by Richardson et al., in 1993 for babies of all birth weights and validated as a predictor of mortality, morbidity, is a physiology-based score that uses 34 routinely available vital signs and laboratory test results [3–5]. As a first generation newborn illness severity score SNAP was cumbersome to use because of number and complexity of items. In 1998, Richardson et al., validated a second generation SNAP score- SNAP II. This score was made simpler by reducing the number of items to six and the duration for first 12 hours of admission in order to minimize the effects of early treatments. To this score were added three more perinatal variables namely birth weight, Apgar scores, and small for gestational age [6] and was known as SNAP II with Perinatal extension (SNAPPE-II) [7].
Objectives of the Study
This study was done to determine the validity of SNAPPE-II (Score for Neonatal Acute Physiology with Perinatal extension-II) in predicting the outcome in terms of mortality and duration of hospital stay at NICU of Indira Gandhi Institute of Child Health, India.
Materials and Methods
A prospective, observational study was carried out on 248 newborns admitted to NICU within 48 hours of birth. This study was conducted at NICU of Indira Gandhi Institute of Child Health, Bangalore from January 2012 to July 2013 for duration of one and half years. Neonates within 48 hours of birth were included and those with congenital malformations incompatible with life, home deliveries where APGARs were not known, infants admitted for observational purposes and those discharged against medical advice within 24 hours of admission were excluded from the study. Informed consent from parents was taken prior to the study. The neonates admitted were first stabilized and resuscitated. Variables for SNAPPE-II were collected prospectively, by doctors as well as trained nurses with in the first 12 hours of admission [8]. Variables other than the scores analyzed were birth weight, gestational age, sex, APGAR Scores at 1 min and 5 min, place and type of parturition, postnatal age at admission and intrauterine growth restriction. Final score was computed as arithmetic sum of points assigned to each item [Table/Fig-1].
| Parameter Range | Score Points |
|---|
| Mean blood pressure (mm Hg) |
| >30 | 0 |
| 20-29 | 9 |
| <20 | 19 |
| Lowest temperature (oF) |
| >96 | 0 |
| 95-96 | 8 |
| <95 | 15 |
| Po2/Fio2 ratio |
| >2.5 | 0 |
| 1-2.49 | 5 |
| 0.3-0.99 | 16 |
| <0.3 | 28 |
| Lowest serum pH |
| >7.2 | 0 |
| 7.1-7.19 | 7 |
| <7.1 | 16 |
| Multiple seizures |
| No | 0 |
| Yes | 19 |
| Urine output (ml/kg/hr) |
| >1 | 0 |
| 0.1- 0.9 | 5 |
| <0.1 | 18 |
| APGAR score |
| >7 | 0 |
| <7 | 18 |
| Birth weight (gm) |
| >1000 | 0 |
| 750-999 | 10 |
| <750 | 17 |
| Small for gestational age |
| <3rd percentile | 12 |
Score was awarded zero for a particular variable when the investigation was not ordered based on clinical assessment
Ethical considerations: The study was approved by ethical committee of the hospital.
Statistical Analysis
The following methods of statistical analysis have been used in this study. To assess the optimal cut off scores, relative operating characteristics (ROC) curve was plotted for the SNAPPE-II Score (expired versus survived) to compare the sensitivity and specificity of score [9]. The area under curve (AUC) was used as an indicator of the ability of the scales to differentiate the mortality in neonates. Univariate analyses of the dichotomous variables encoded were performed by means of the Chi square test with Yates correction if required. One way Analysis of Variance (ANOVA) were used to test the difference between groups. In the entire above tests p-value less than 0.05 were taken to be statistically significant. The data was analysed using SPSS package (Statistical Package for the Social Sciences).
Results
248 newborns met inclusion criteria out of which 39 babies succumbed. Crude NICU mortality rate was 15.7%. Out of 248 babies, 85 were preterm (34.2%), with an average of 34 weeks and range of (31-36 weeks), 152(61.2%) were term and 11(4.4%) were post term babies with an average of 44 weeks (43-44 weeks).
The mean SNAPPE-II score among expired babies was 45.72±18.68 compared to survived babies who had a score of 21.04±15.418 [Table/Fig-2]. In our study SNAPPE-II score of 37 and above had a positive predictive value of 95.3%, sensitivity 76.9% and specificity of 87.1% in predicting death. Area under the curve by using the ROC for SNAPPE-II was found to be 0.849 (95%CI 0.79-0.97) which is classified as good [Table/Fig-3].
SNAPPE-II in predicting mortality
| Outcome | N | Mean SNAPPE-II Score | SD ± | Minimum | Maximum | ‘t’ value | ‘p’ value |
|---|
| Discharged | 209 | 21.04 | 15.418 | 0 | 69 | 78.489 | <0.001 |
| Expired | 39 | 45.72 | 18.689 | 0 | 87 |
| Total | 248 | 24.92 | 18.301 | 0 | 87 |
AUC cut-off value, sensitivity and specificity
In term babies, the mean SNAPPE-II score was 24.1± 15 in case of survived and 52.8±15 in case of expired children whereas in preterms the score was 14.87±13 and 31.7±16 in the survived and expired group respectively [Table/Fig-4]. The mean length of stay was found to increase from SNAPPE-II score of 11-40 and mean LOS for children with score of more than 40 was found to decrease.
SNAPPE-II with gestational age
| Outcome | Gestational Age (Weeks) | N | Mean SNAPPE-II Score | SD ± | Min. | Max. |
|---|
| Discharged | <37 | 71 | 14.87 | 13.909 | 0 | 51 |
| >=37 | 138 | 24.16 | 15.081 | 0 | 62 |
| Total | 209 | 21.00 | 15.308 | 0 | 62 |
| Expired | <37 | 14 | 31.71 | 16.831 | 0 | 55 |
| >=37 | 25 | 52.88 | 15.325 | 16 | 87 |
| Total | 39 | 45.28 | 18.736 | 0 | 87 |
Discussion
SNAPPE-II showed good correlation with outcome in terms of mortality irrespective of gestational ages. The mean SNAPPE-II score among expired babies was 45.72±18.68 compared to survived ones who had a score of 21.04±15.418. In a study conducted by Mia RA et al., [10] score of expired vs. survived babies were 42.75±18.59 vs. 17.4±14.05.
In the present study SNAPPE-II score of 37 and above were associated with higher mortality. In a study conducted by Mia RA et al., [10] a score of 30 and above, Study by Suksham Jain and Anuradha Bansal [11] scores of 40 and above, Ramirez et al., score of 40 [12] and above, study done by Ucar et al., [13] scores of 33 and above, study by Olaf Dammann et al., [14] a score of 30 and above, study by James Thimoty et al., [15] 51 and above were associated with higher mortality. A similar study conducted by Kadivar M et al., concludes that SNAPPE-II score can be used to predict mortality among the NICU patients [16].
Higher the SNAPPE-II score higher the mortality rate [Table/Fig-5] except in the score range of 21- 30 which showed poor correlation in terms of mortality. This can be explained by the fact that these neonates were stable at the time admission when scoring was carried out i.e. within first 12 hours, but later deteriorated due to changing hemodynamics and some of them, especially preterm babies, acquired nosocomial infections.
Frequency distribution of SNAPPE II
| SNAPPE-II Score | Outcome | Total |
|---|
| Discharged | Expired |
|---|
| 0-10 | 65(98.5%) | 1(1.5%) | 66 |
| 11- 20 | 49(92.5%) | 4(7.54%) | 53 |
| 21-30 | 30(96.8%) | 1(3.22%) | 31 |
| 31-40 | 45(84.9%) | 8(15.1%) | 53 |
| 41-50 | 14(61%) | 9(39%) | 23 |
| 51-60 | 4(35.72%) | 9(64.28%) | 14 |
| 61-70 | 2(20%) | 4(80%) | 5 |
| 71-80 | 0(0%) | 2(100%) | 2 |
| >80 | 0(0%) | 1(100%) | 1 |
| Total | 209 | 39 | 248 |
Chi-square value : 74.913
‘p’ value : <0.001
The mean length of stay [Table/Fig-6] was found to increase from score of 11-40 but this was not statistically significant. Mean LOS for children with score of more than 40 was found to decrease suggesting that these neonates were sick at admission and succumbed to disease early.
Length of hospital stay according to SNAPPE II
| SNAPPE-II Score | N | Mean D.O.S(Days) | Std. Deviation (±) | Minimum | Maximum | ‘F’ value | ‘p’ value |
|---|
| 0-10 | 66 | 10.62 | 8.598 | 1 | 35 | 1.279 | 0.255 |
| 11-20 | 53 | 8.87 | 6.959 | 2 | 45 |
| 21-30 | 31 | 9.13 | 7.553 | 2 | 45 |
| 31-40 | 53 | 12.58 | 6.932 | 1 | 30 |
| 41-50 | 23 | 10.17 | 6.893 | 1 | 27 |
| 51-60 | 14 | 9.89 | 13.304 | 2 | 50 |
| 61-70 | 5 | 9.80 | 11.077 | 1 | 28 |
| 71-80 | 2 | 2.50 | .707 | 2 | 3 |
| >80 | 1 | 1.00 | – | 1 | 1 |
| Total | 248 | 10.24 | 8.056 | 1 | 50 |
Limitations of Study
As SNAPPE II score is an admission score, it doesn’t correctly predict the outcome in neonates whose internal milieu is undergoing dynamic changes and in those preterm neonates who are going to develop nosocomial infections.
Conclusion
SNAPPE II score is a good predictor of mortality irrespective of gestational ages. It assists the clinician in identifying very sick neonates and prioritizing treatment to these neonates. It also helps in counseling the parents regarding the severity of illness and the probable treatment cost involved. SNAPPE II does not accurately predict the length of stay.
Score was awarded zero for a particular variable when the investigation was not ordered based on clinical assessment
Chi-square value : 74.913
‘p’ value : <0.001
[1]. Lee SK, McMillan DD, Ohlsson A, Pendray M, Synnes A, Whyte R, Variations in practice and outcomes in the Canadian NICU network: 1996-1997Pediatrics 2000 106(5):1070-79. [Google Scholar]
[2]. Sankaran K, Chien LY, Walker R, Seshia M, Ohlsson A, Lee SK, Variation in mortality rates among Canadian neonatal intensive care unitsCMAJ 2002 166(2):173-78. [Google Scholar]
[3]. Richardson DK, Gray JE, McCormick MC, Workman K, Goldman DA, Score for neonatal acute physiology: a physiology severity index for neonatal intensive carePediatrics 1993 91(3):617-23. [Google Scholar]
[4]. Escobar GJ, Fischer A, Li DK, Kremers R, Armstrong MA, Score for neonatal acute physiology: validation in three kaiser permanente neonatal intensive care unitsPediatrics 1995 96(5 Pt 1):918-22. [Google Scholar]
[5]. Petridou E, Richardson DK, Dessypris N, Malamitsi Puchner A, Mantagos S, Nicolopoulos D, Outcome prediction in Greek neonatal intensive care units using a score for neonatal acute physiology (SNAP)Pediatrics 1998 101(6):1037-44. [Google Scholar]
[6]. Richardson DK, Phibbs CS, Gray JE, McCormick MC, Workman-Daniels K, Glodman DA, Birthweight and illness severity: Independent predictors of neonatal mortalityPediatrics 1993 91(5):969-75. [Google Scholar]
[7]. Richardson DK, Corcoran JD, Escobar GJ, Lee SK, SNAP-II and SNAPPE-II: simplified newborn illness severity and mortality risk scoresJ Pediatr 2001 138(1):92-100. [Google Scholar]
[8]. Beal J, Richardson DK, Dembinskisi S, Hipp KO, McCourt M, szlachetka D, Responsibilities, roles and staffing patterns of nurse practitioners in the neonatal intensive care unitMCN Am J Matern Child Nurs 1999 24(4):168-75. [Google Scholar]
[9]. Hanley JA, Mcneil BJ, The meaning and use of the area under a receiver operating charecterstics(ROC) curveRadiology 1982 143(1):29-36. [Google Scholar]
[10]. Mia RA, Etika R, Harianto A, Indarso F, Damanik SM, The use of score for neonatal acute physiology perinatal extention II (SNAPPE II) in predicting neonatal outcome in neonatal intensive care unitPaediatrica Indonesiana 2005 45:241-45. [Google Scholar]
[11]. Jain S, Bansal A, SNAPPE II score for predicting mortality in a level II neonatal intensive care unitDicle Med J Cilt 2009 36(4):333-35. [Google Scholar]
[12]. Ramirez MNM, Godoy LE, Barrientos EA, SNAP II and SNAPPE II as Predictors of Neonatal Mortality in Pediatric Intensive care unit: Does postnatal age play a role?International Journal of Pediatrics 2014 Article ID 298198. http://dx.doi.org/10.1155/2014/298198 [Google Scholar]
[13]. Ucar S, Varma M, Ethemoglu MI, Acar NK, The Efficacy of SNAPPE. II-II in Predicting morbidity and mortality in Extremely Low Birth Weight InfantsArch Dis Child 2014 99(suppl 2):A468 [Google Scholar]
[14]. Dammann O, Shah B, Naples M, Bednarek F, Zupancic J, Allred EN, SNAP-II and SNAPPE-II as predictors of death among infants born before the 28th week of gestation. Inter-institutional variationsPediatrics 2009 124(5):e1001-06. [Google Scholar]
[15]. Thimoty J, Hilmanto D, Yuniati T, Score for neonatal acute physiology perinatal extension II (SNAPPE II) as the predictor of neonatal mortality hospitalized in neonatal intensive care unitPaediatrica Indonesiana 2009 49(3):155-59. [Google Scholar]
[16]. Kadivar M, Sagheb S, Bavafa F, Moghadam L, Eshrati B, Neonatal mortality risk assessment in a neonatal intensive care unit (NICU)Iranian Journal of Pediatrics 2007 17(4):325-32. [Google Scholar]