Primary Retroperitoneal Inflammatory Myofibroblastic Tumour
Tarun Jindal1, Rajan Kumar Sinha2, Barun Saha3, Nilanjan Mitra4, Subhabrata Mukherjee5
1 Resident, Department of Urology, Calcutta National Medical College, Kolkata, India.
2 Resident, Department of Urology, Calcutta National Medical College, Kolkata, India.
3 Resident, Department of Urology, Calcutta National Medical College, Kolkata, India.
4 Resident, Department of Urology, Calcutta National Medical College, Kolkata, India.
5 Resident, Department of Urology, Calcutta National Medical College, Kolkata, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rajan Kumar Sinha, 11A/1C Mohendra Chatterjee Lane, Gobra, Near Bamunpara Bazar, Kolkata-700046, India.
E-mail: rajan_rims@yahoo.co.in
Neoplasms, Pseudo tumour, Retroperitoneum
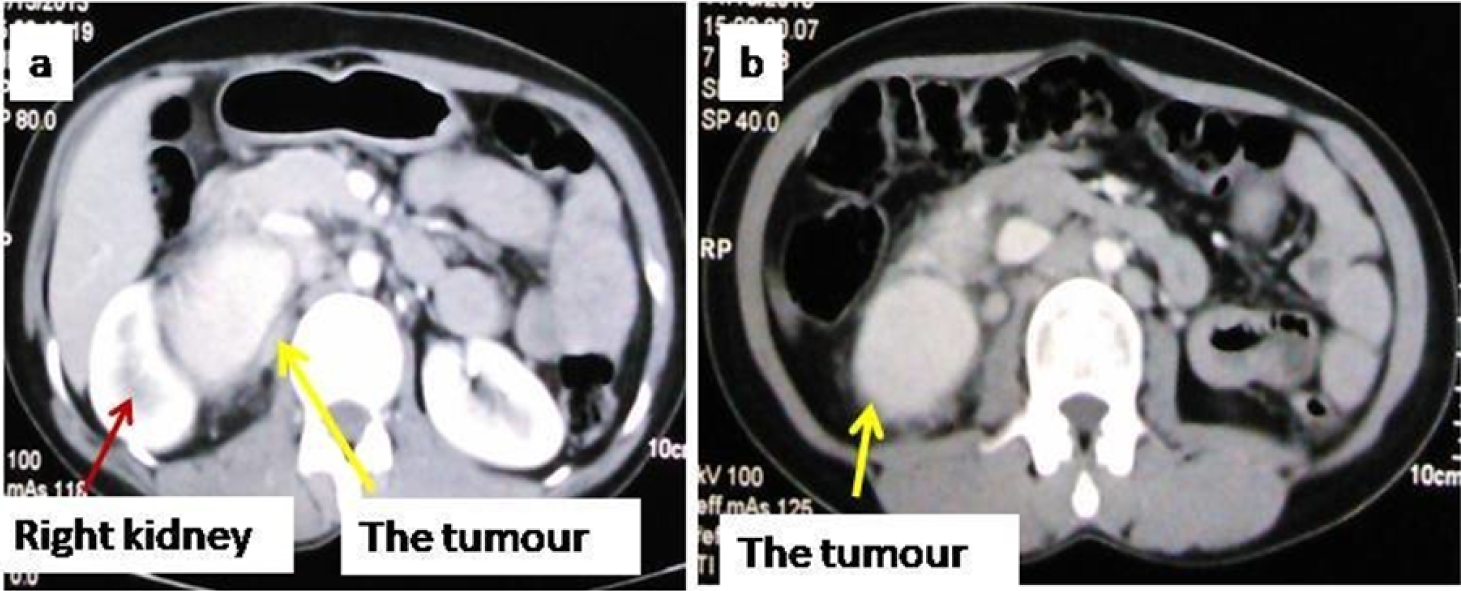
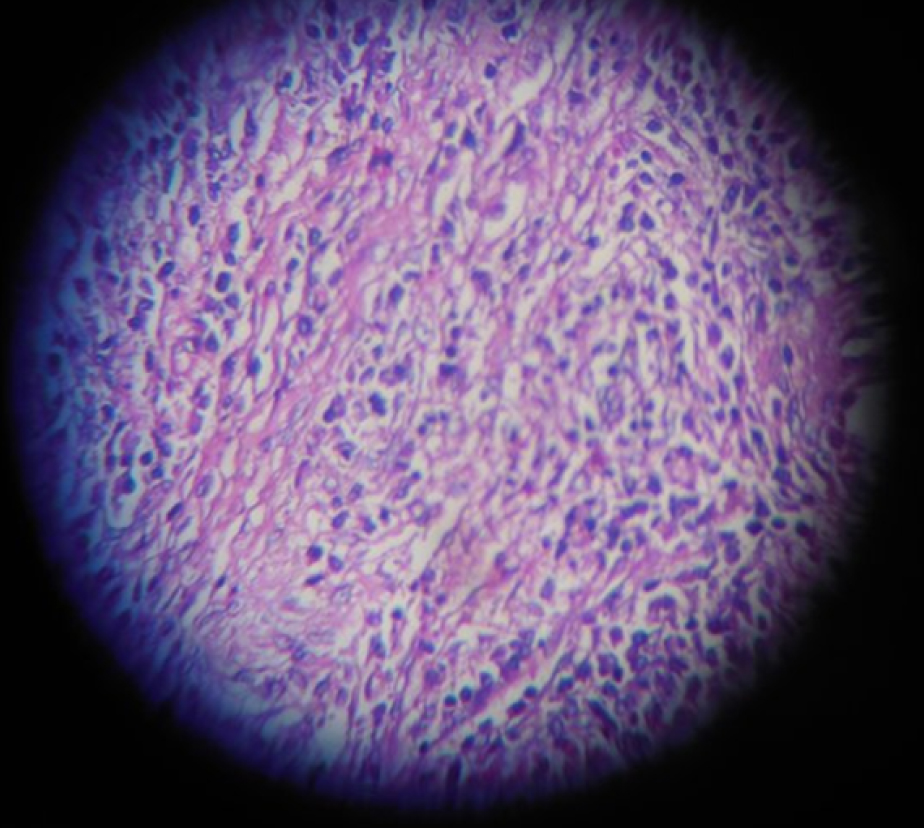
Inflammatory myofibroblastic tumours are uncommon neoplasms of unknown aetiology. They commonly involve the lung and their occurrence in the retroperitoneum can be considered anecdotal. A 30-year-old female presented with dull aching, intermittent pain in the right flank for six months. There was a history of weight loss of 4kg over six months. There was no history of any medical co-morbidity or past surgical intervention. The clinical examination was normal. Haemogram revealed increased erythrocyte sedimentation rate but the serum biochemistry was within normal limits. Ultrasound examination of the abdomen was suggestive of a heterogeneous mass in close relation to the lower pole of the right kidney. Contrast enhanced CT scan revealed a 5 cm x 6 cm mass in the retroperitoneum, anterior to the right psoas muscle and in close relation to the lower pole of the right kidney. The mass showed contrast enhancement in the arterial phase and the enhancement persisted even in the delayed scan. There was evidence of fat stranding around the mass [Table/Fig-1a&b]. The possibility of a retroperitoneal sarcoma, Castleman’s disease and an inflammatory mass were considered. As the diagnosis was not certain, a CT guided tru-cut biopsy from the mass was performed which suggestive of an inflammatory myofibroblastic tumour. The metastatic work-up was negative. The patient was taken up for open surgical excision of the mass via right flank approach. At surgery, the mass was well circumscribed and could be separated from the kidney and the inferior venacava by blunt and sharp dissection [Table/Fig-2a-d]. The histopathological examination shows polymorphic cells composed of lymphocytes and plasma cells along with plump spindle cells arranged in fasicular pattern which is consistent with the diagnosis of inflammatory myofibroblastic tumour [Table/Fig-3]. The patient made an uneventful recovery and is well at a follow up of six months.
(a) Contrast enhanced CT scan showing the enhancing tumour (yellow arrow) in close proximity to the lower pole of the right kidney (red arrow) and inferior venacava. There was evidence of fat stranding all around the tumour. (b) The lower part of the tumour is seen
(a) At surgery, the tumour could be separated from the kidney. (b) The tumour, after mobilisation following blunt and sharp dissection. (c) The tumour after excision. (d) The cut section of the tumour

The histopathological picture of the tumour revealing polymorphic cells composed of lymphocytes and plasma cells along with plump spindle cells arranged in fasicular pattern (Haematoxylin & Eosin, 100X)
Inflammatory myofibroblastic tumour, also known as pseudo tumour, plasma cell granuloma is a rare neoplasm. It is presumed to occur as a result of trauma, infection, previous surgical intervention, etc [1,2] and most often involves the bladder [3]. The patients usually present with non specific symptoms like pain abdomen, loss of weight, fever. Anaemia, elevated counts and erythrocyte sedimentation rate can also be seen. At imaging, the tumour usually shows heterogeneous enhancement but again, there are no specific features. Of late, Positron emission tomography has also been reported to be helpful. The tumour, by the virtue of associated inflammation, has been found to have high standardized uptake value on a 18F- fluorodeoxyglucose positron emission tomography. Though these findings support the diagnosis, histopathological examination along with immunohistochemistry remains the confirmatory investigation [4,5].
The retroperitoneal inflammatory myofibroblastic tumours are extremely rare neoplasms having non-specific symptoms and imaging findings. Surgical removal remains the mainstay of treatment.
[1]. Coffin CM, Watterson J, Priest JR, Extrapulmonary inflammatory myofibroblastic tumour (inflammatory pseudotumour). A clinicopathologic and immunohistochemical study of 84 casesAm J Surg Pathol 1995 19:859-72. [Google Scholar]
[2]. Su LD, Atayde-Perez A, Sheldon S, Inflammatory myofibroblastic tumour: cytogenetic evidence supporting clonal originMod Pathol 1998 11:364-68. [Google Scholar]
[3]. Attili SV, Chandra CR, Haemant DK, Retroperitoneal inflammatory myofibroblastic tumourWorld J Surg Oncol 2005 3:66 [Google Scholar]
[4]. Jindal T, Kumar A, Dutta R, Combination of (18)-FDG and (68)Ga-DOTATOC PET-CT to differentiate endobronchial carcinoids and inflammatory myofibroblastic tumoursJ Postgrad Med 2009 55:272-74. [Google Scholar]
[5]. Alongi F, Bolognesi A, Gajate AM, Inflammatory pseudotumour of mediastinum treated with tomotherapy and monitored with FDG-PET/CT: case report and literature reviewTumouri 2010 96(2):322-26. [Google Scholar]