Adenoid cystic carcinomas (ACC) of the lacrimal gland are rare tumours, accounting for 1.6% of all orbital tumours [1,2]. Despite the rarity, it is the most common malignant epithelial tumour of the lacrimal gland and accounts for 25-40% of all epithelial tumours [3]. Histological characteristics of lacrimal gland ACC are similar to salivary gland ACC but carry a poorer prognosis.
Lacrimal gland ACC is a therapeutic challenge due to their aggressive behaviour and complex orbital anatomy limiting complete surgical resection. Delayed diagnosis, tendency for peri-neural invasion, infiltration to periosteum and local recurrence are factors resulting in poor outcome. The survival rates are dismal with less than 50% at 5 years and 20% at 10 years [4].
Surgery has remained the cornerstone of therapy. However, the majority of these tumours extend outside the capsule making surgical resection difficult and incomplete that could result in poor cosmetic and functional outcome. Mortality is most commonly due to perineural invasion and intracranial spread and survival is dismal [5]. Favourable outcome limited to local control has been reported with adjuvant radiotherapy [6,7]. Based on these reports we have designed a protocol based postoperative radiotherapy that could be applied in cases of incomplete tumour resection, positive margins, bone infiltration and perineural invasion. Given the rarity of lacrimal gland ACC, level I evidence for treatment recommendations are limited [4].
To the best of our knowledge, no comparative study is available to establish the standard of care. In this communication we have reported the role of conformal radiotherapy as adjuvant therapy in ACC of lacrimal gland with review of literature. We believe our observations will contribute to the management of this rare clinical entity.
The study was aimed at evaluating the role of adjuvant three dimensional conformal radiotherapy (3D-CRT) in cases of incomplete (R1) resection along with review of literature pertaining to management of lacrimal ACC.
Materials and Methods
Patient characteristics
This is a retrospective analysis of patients registered in Radiotherapy clinic at Institute Rotary Cancer Hospital, All India Institute of Medical Sciences, New Delhi between December 2006 and June 2013. Ten patients of biopsy proven ACC of lacrimal gland were treated with radiotherapy following biopsy or incomplete resection. Pre-treatment evaluation included detailed history and physical examination, routine haematological and biochemical investigations, computed tomography of orbit. Distant metastatic workup was limited to a chest radiograph and ultrasonography of abdomen. All patients underwent a contrast enhanced computed tomography of head and neck prior to radiotherapy planning to assess the local extension and lymph node involvement.
Patient records were reviewed for demographic profile, presenting symptoms, imaging, histopathological findings, size of tumour, and presence of peri-neural invasion, bone infiltration, surgical resection, adjuvant or palliative treatment delivered.
American joint committee on cancer (AJCC 6th edition) guidelines for ACC of lacrimal gland were followed to ascertain the clinical stage of the disease [8]. (Currently AJCC 7th Edition 2010 is followed but this being retrospective data from 2006 we had followed AJCC 6th Edition).
Treatment details: Radiotherapy consisted of Linac based 3-dimensional conformal radiotherapy (Elekta Medical Systems Crawley, UK) in adjuvant setting for 8 patients. Three dimensional (3-D) treatment planning allows accurate delineation of target, and surrounding critical structures. Dose distribution is therefore optimum with verification of treatment volume.
The surrounding critical structures also known as organs at risk included in our study were opposite eye, optic nerve, optic chiasm, temporal lobes, and brainstem.
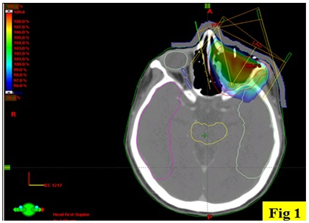
Adjuvant radiotherapy consisted of 60 Gray (Gy) in 30 fractions over 6 weeks. Two patients with advanced disease received palliative radiotherapy 30 Gy in 10 fractions over 2 weeks in Theratron 780C (Best Theratronics, Ottawa, Canada). All patients underwent CT simulation, Brilliance Big Bore CT simulator (Phillips Medical System Cleveland, OH, USA) with dummy markers and a CT scan of the face and neck using 3 mm slices. The images were transferred to ECLIPSE (Varian Medical Systems, Palo Alto, CA version 6.5) treatment planning system. Gross tumour volume (GTV) and clinical target volume (CTV) was generated according to initial radiological extension of the disease. The lateral orbital wall, superior orbital fissure and orbital roof were included in the CTV. Planning target volume (PTV) was generated with 5 mm margin for daily setup variation. Radiation portals included two anterior oblique beams [Table/Fig-1].
Three-dimensional radiotherapy planning showing radiation portals and target volume
Evaluation of treatment response: Patients were monitored during the course of radiotherapy weekly with haematological investigations and clinical examination for acute treatment related morbidities.
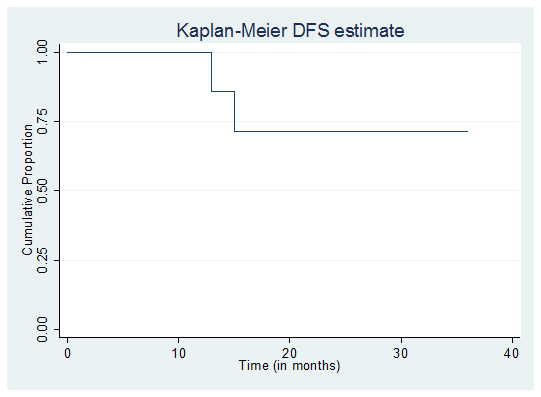
Acute toxicities for skin, conjunctiva and cornea were recorded. We practice regular clinical examination every 3 months and with CT imaging at 6 months after completion of treatment for the first 2 years and subsequently clinical examination with imaging every 6 months or earlier in the presence of clinical suspicion till 5 years The Kaplan Meier Disease free survival at 15 months was 71% (CI 0.2582 -0.9198) [Table/Fig-2].
Kaplan Meier Disease free survival at 15 months was 71% (CI 0.2582 -0.9198)
Ethical clearance and informed consent: This is a retrospective data. The study was approved by Institute Ethics Committee Ref. No: IEC/NP-288/01-08-2014.
Results
The demographics and treatment characteristics are summarized [Table/Fig-3]. The median age was 32 years (Range: 12-56 years). The female to male ratio was 1:1. Median duration of symptoms was 7 months. The commonest presentation was proptosis in 8 followed by diminished vision in 2 patients. The diagnosis in all 10 patients was established by histopathological examination of tumour. The AJCC classification at initial diagnosis ascertained 6 patients as T3N0M0 and 4 patients as T4N0M0. Distribution of tumour histologic subtype was cribriform type in 5 patients, sclerosing type in 2 and predominantly basaloid (solid) in 2 patients. Subtype could not be ascertained in one patient. Peri-neural invasion was observed in 5 patients at presentation. Eight patients underwent orbitotomy and tumour excision. Two patients with extensive disease underwent an incisional biopsy to establish the tumour diagnosis. Postoperative adjuvant radiotherapy was planned for 8 cases and 2 patients underwent palliative radiotherapy.
| Characteristics | | Percentage |
|---|
| Age(years) | (12-56) | |
| Median | 32 | |
| Sex |
| Male | 5 | 50% |
| Female | 5 | 50% |
| Clinical presentation |
| Proptosis | 8 | 80% |
| Loss of vision | 2 | 20% |
| Duration of symptoms Range | 2-60 months | |
| (Median) | 7 | |
| Surgery |
| Orbitotomy | 8 | 80% |
| Biopsy | 2 | 20% |
| Stage |
| T3N0M0 | 6 | 60% |
| T4N0M0 | 4 | 40% |
The interval between surgery and radiotherapy ranged from 2-18 months (median 3 months). Adjuvant radiotherapy was planned in one patient after re-excision following recurrent disease hence the gap between initial surgery and adjuvant radiotherapy. Normally adjuvant radiotherapy is planned between 6-8 weeks if wound has healed and is suitable for radiotherapy. It sometimes gets delayed for various reasons including long waiting time in our institute and patient compliance Radiotherapy dose ranged from 30-60Gy. A median postoperative radiotherapy dose was 60 Gy. During radiotherapy all patients developed grade 1-2 skin reaction. Four patients developed grade 2 conjunctival reactions as per RTOG (Radiotherapy Oncology Group) toxicity criteria. All patients were managed with conservative treatment. Median follow up was 21 months. At the last follow up 8 of 10 patients had complete response, and 2 patients developed progressive disease. This progression was noted in patients treated with palliative intent. One patient had systemic failure with bone metastasis and the other had local progression only. Treatment details of all patients have been summarized in [Table/Fig-4].
| S. No | Gender | Age | Stage | Histology | Type | Treatment | | Status at last follow up |
|---|
| 1 | M | 26 | T3N0M0 | ACC | Sclerosing | surgery | RT | 13 Months No recurrence |
| 2 | M | 28 | T3N0M0 | ACC | Sclerosing | surgery | RT | 5 months No recurrence |
| 3 | F | 30 | T4N0M0 | ACC | Cribriform | surgery | RT | 4 Months No recurrence |
| 4 | F | 39 | T4N0M0 | ACC | Solid | Pall RT | Pall CT | 15 Months Bone Mets |
| 5 | M | 51 | T3N0M0 | ACC | Cribriform | surgery | RT | 16 months No recurrence |
| 6 | F | 32 | T3N0M0 | ACC | Solid | surgery | RT | 21 months No recurrence |
| 7 | M | 56 | T4N0M0 | ACC | Cribriform | Pall RT | RT | 11 months Local progression |
| 8 | M | 50 | T3N0M0 | ACC | Cribriform | surgery | RT | 36 months No recurrence |
| 9 | F | 30 | T4N0M0 | ACC | Cribriform | surgery | RT | 21 months No recurrence |
| 10 | F | 12 | T3N0M0 | ACC | NA | surgery | RT | 20 months No recurrence |
M: Male, F: Female, RT: Radiotherapy, CT: chemotherapy, ACC: Adenoid Cystic Carcinoma, Pall: Palliative T, N, M: TNM staging as per AJCC staging system
Discussion
This report is an attempt to study the role of adjuvant radiotherapy on the outcome of locally advanced ACC of lacrimal gland. The present study clearly demonstrates the beneficial role of adjuvant radiotherapy in loco-regional control of ACC of lacrimal gland even in advanced stage (T3/T4) of the disease. The delay in diagnosis or referral is not unique in our case. Ni et al., have reported that fewer than 15% patients were diagnosed within 2 months and in 72% patient’s treatment were started after one year because of delay in diagnosis [9]. Radiological imaging and high clinical suspicion for unilateral mass in the upper temporal quadrant is mandatory given the late presentation and diagnosis.
Ahmad et al., have observed that many ophthalmologists do not stage lacrimal gland tumours according to the AJCC criteria; thus, there is heterogeneity in tumour classification that affects the outcome analysis [7]. In our series, 6 patients had stage T3N0M0 and the remaining 4 had stage T4N0M0. Several studies have suggested the solid variant as the most aggressive form which is associated with poor prognosis [5,6]. The present study had only two patients of such subtype and did not validate such a correlation.
The treatment of primary lacrimal gland ACC demands a multidisciplinary approach. Complete surgical resection in lacrimal gland tumours is rarely obtained due to adjacent critical structures such as opposite eye, optic nerve, optic chiasm, temporal lobes, brain stem.
Huber et al., retrospectively compared radiotherapy with neutrons, photons, and a photon/neutron mixed beam in patients with advanced ACC of the head and neck; fast neutron radiotherapy provided higher local control rates than a mixed beam and photons in advanced, recurrent, or incompletely resected ACC [10]. However, the type of radiation did not impact survival, which is dominated by the high number of distant metastases in adenoid cystic carcinoma. In the present study, all patients for adjuvant radiotherapy were planned by 3-D conformal radiotherapy and at median follow up of 21 months none of the 8 patients who had complete response had any evidence of local recurrences or metastasis.
Limitations
The study has limitations of small number, retrospective analysis, lack of randomization and short follow up due to poor patient compliance. However, randomized control trial is not ideal for such a rare condition.
Conclusion
Adjuvant radiotherapy delivered by 3D conformal technique in locally advanced ACC of lacrimal gland with incomplete resection, close or positive margins, residual disease, peri-neural spread showed improved loco-regional control with acceptable morbidity.
M: Male, F: Female, RT: Radiotherapy, CT: chemotherapy, ACC: Adenoid Cystic Carcinoma, Pall: Palliative T, N, M: TNM staging as per AJCC staging system