Airways of normal persons show variability in caliber and this phenomenon gets exaggerated in case of asthmatic and chronic obstructive pulmonary disease (COPD) individuals [1–3]. Measurement of bronchial hyper-reactivity and airways variability has always posed a challenge for experimental purposes. Variability in peak expiratory flow (PEF) has been suggested as a marker for bronchial hyper-reactivity [4,5]. Several evidence suggest that airway variability exhibits a definite circadian pattern in which morning PEF levels are lower than daytime values, with a minimum in early morning and peak in evening [1,6]. The pattern of variability is exaggerated in smokers and in COPD and in asthmatic patients [1]. The various spirometric indices reflect airflow characteristics of different airways. Forced expiratory flow (FEF), at 25% FVC, i.e. FEF25 reflects small airways, at 75% FVC (FEF75) reflects large airways and at 50% FVC (FEF50) reflects mid/small airways. FEF from 25% to 75% FVC (FEF25-75), reflects mid/small airways and is also known as mid expiratory flow. Forced expiratory volume in one second (FEV1) reflects the caliber of both large and small airways, whereas PEF is more a reflection of the caliber of large airways [7]. In general FEV1 is a more reliable indicator of airflow limitation than PEF [8]. Unfortunately most studies that describe diurnal variability in airways caliber in asthmatics have used PEF rather than FEV1. Moreover, the diurnal variability of small, mid and large airways has not been studied systematically. This study was designed to assess diurnal variability in FEF25, FEF50, FEF75, FEF25-75, PEF and FEV1 measured simultaneously and to compare variations in these measurements in normal subjects.
Materials and Methods
Subjects
The study was conducted on 182 young male/female volunteers from university population having almost similar daily routine, selected randomly between the age group of 18-30 years. The study protocol was duly approved by institutional ethics committee. The subjects were explained about the study and informed consent was taken before participation.
A thorough clinical history was taken and anthropometric measurements (height and weight) were recorded. Exclusion criteria were history of smoking, history of severe chest trauma, with chest and spinal deformity, with personal/family history of asthma, chronic obstructive pulmonary diseases and other cardio-respiratory diseases. Brief clinical examination was done to rule out any obvious cardio-pulmonary compromise.
Devices
The Spirobank G (MIR; Rome, Italy) spirometer is an infrared interruption turbine based device. These device records spirometry parameters, including FEV1, PEF, forced vital capacity, forced expiratory flow, forced expiratory time and flow/volume curves. Flow range of this device is ± 16 L/s with maximal volume of 10 L. Flow accuracy of this device is 5% or 200 mL/s, and volume accuracy is 3% or 50 mL (whichever is greater). Spirobank G device met or exceeded the latest ATS accuracy standards.
Protocol
Subjects were asked to report in Pulmonary Function Laboratory at 8:00 AM and again at 5:00 PM for spirometery testing. Spirometery was performed with Spirobank G between 8:00-8:30 AM in morning and 5:00-5:30 PM in evening. In a day, spirometery was done from 8-10 subjects only. Subjects were instructed to come to laboratory with atleast 2 hours of fasting before spirometery testing. Spirometry was done by a trained technician with Spirobank G as per the ATS guidelines [9]. The test curve with the highest sum of the FVC and FEV1 were taken for further analysis. All recordings were performed in standing position and a nose clip was used to prevent nasal leakage.
Recorded data was scrutinized and any incomplete or inadequate test record was rejected. Finally, data from 161 subjects was found to be complete and appropriate and was taken for the analysis.
Statistical Analysis
Morning and evening values of FEV1, FEF25, FEF50, FEF25-75, FEF75 and FVC were compared using paired sample t-test. Diurnal variation (dv) of all parameters for the individual subject was calculated as the ratio of, the difference between morning and evening values, and their mean. The Diurnal variabilities of different parameters were compared using one way analysis of variance. All statistical tests were performed with SPSS 21. A p-value of less than 0.05 was considered as significant.
Results
A total of 161 subject’s data was analysed. The mean age of subjects was 23.6 ± 3.1 with male female ratio of 116:45. Mean height and mean weight of subjects was 167.1 ± 9.2 and 61.2 ± 11.1 respectively. All subjects were with normal lung functions, non smokers, without personal/family history of pulmonary and cardiovascular disease. Basal parameters data for males and females is presented in [Table/Fig-1].
Subject basal characteristics. Spirometeric parameters represent basal values measured at 8:00 AM. Data presented are mean ± SD
| Basal Parameters | Males | Females |
|---|
| Number (n) | 116 | 45 |
| Age | 23.74±3.10 | 23.24±3.16 |
| Height | 171.03±7.30 | 156.98±4.70 |
| Weight | 64.09±10.55 | 53.87±8.85 |
| FEF25 | 6.88±1.09 | 6.25±1.27 |
| FEF25-75 | 3.83±0.77 | 3.25±0.81 |
| FEF50 | 4.23±0.97 | 3.54±0.86 |
| FEF75 | 1.80±0.40 | 1.51±0.49 |
| FEV1 | 3.62±0.36 | 2.89±0.28 |
| FVC | 4.28±0.43 | 3.35±0.24 |
| FEV1% | 84.79±4.77 | 86.30±5.17 |
| PEF | 8.94±1.05 | 8.00±0.90 |
The comparison between morning and evening values of PEF, FEV1, FEF25, FEF50, FEF25-75, FEF75 and FVC and their diurnal variability as measured with the digital spirometer is given in [Table/Fig-2]. As evident from the data morning values are lower than in the evening (p<0.001), except FVC.
Spirometric parameters recorded in morning and evening and their diurnal variability
| Parameter | Morning values | Evening values | Diurnal Variability |
|---|
| FEF25 | 6.70±1.18 | 6.89±1.21* | 7.63±6.20 |
| FEF25-75 | 3.67±0.82 | 3.86±0.87* | 9.34±9.41 |
| FEF50 | 4.04±0.99 | 4.24±1.09* | 10.51±11.07 |
| FEF75 | 1.72±0.45 | 1.84±0.46* | 12.98±11.75 |
| FEV1 | 3.42±0.47 | 3.46±0.46# | 3.69±3.41 |
| FEV1% | 85.21±4.92 | 86.42±4.81* | 3.04±2.85 |
| FVC | 4.02±0.57 | 4.02±0.56 | 4.00±4.63 |
| PEF | 8.68±1.09 | 8.90±1.04* | 6.21±5.57 |
Total No. of subjects (n) = 161. Data presented are mean ± SD, # represents significant difference (p<0.05) using paired t-test,* represents highly significant difference (p<0.001) using paired t-test
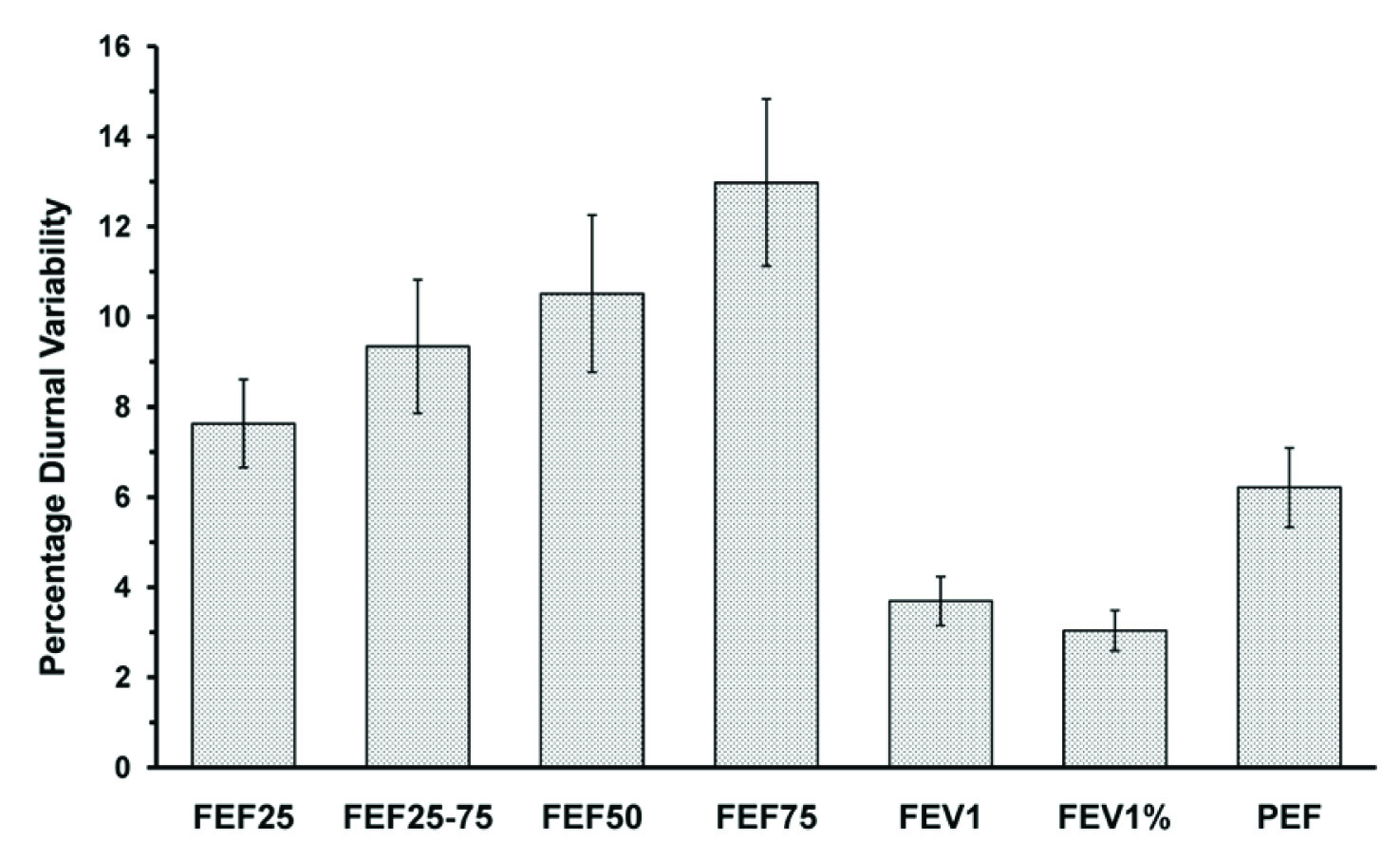
The diurnal variability in different parameters also differs significantly (ANOVA, p<0.05) as depicted in [Table/Fig-3]. The diurnal variability is highest in large airways as reflected by FEF75 and Lowest in smaller airways as reflected by FEF25. The diurnal variability was lowest for FEV1%.
Diurnal variability of spirometric parameters. Difference in diurnal variability are significant (ANOVA, p<0.05). Error bars represents ± 1 SE
Discussion
Variability in airways caliber exhibits a definite circadian pattern with values of PEF being lowest in the morning and assuming peak values in evening [1,6]. Only few studies with a limited number of subjects are available regarding the diurnal variability of FEV1 [10–12].
The morning and evening spirometric parameters including FEV1% and PEF shows a significant difference which is in accordance with already published data [10–12]. In addition present study has also made an attempt in characterizing the diurnal variability in proximal and distal airways using PEF and FEV1. Results suggest that diurnal variability in PEF is higher than in FEV1 in healthy subjects. Furthermore, intrinsic variability in a single session (both morning and evening) spirometry has been reported to be higher for PEF than FEV1, which is in agreement with results of previous studies [13].
PEF reflects primarily proximal airway caliber changes while FEV1 reflects the airway caliber of proximal and peripheral airways [7]. The greater variability of proximal airways may be interpreted as an effect of airway geometry. In large airways, same fractional reduction in airway caliber leads to greater decrease in flow as compared to that in smaller airways, in agreement with the general concept that flow rate or resistance being inversely proportional to the fourth power of radius. This further may be explained by the fact that the proximal and distal airways differ in smooth muscle content and nerve supply. As, we proceed from proximal to distal airways the density of nerve supply and smooth muscle mass decreases [14], which may account for lower diurnal variability in smaller airways.
The diurnal variability in PEF and FEV1 are found to be significantly correlated, representing that the changes in proximal airways caliber correspond to change in distal airways caliber. The mean FEV1 in the morning and in evening are significantly different representing that there exists a diurnal variability in FEV1. Furthermore, mean PEF in the morning and in evening are significantly different, which is in accordance with results of previous studies [1,6].
FEV1 total variability is lowest and maximum variability is less than 10%; therefore, it is clinically most suitable. Mid expiratory flow the variability is high; therefore, its clinical use may not be justified. The range of variability of FEV1 and PEF are in accordance with previous study also.
Conclusion
In summary, the diurnal variability in airways caliber is well reflected in FEV1, FEF and PEF. The scope of this study was to investigate the diurnal variability in spirometeric parameters with just two recordings in a day. To better characterize the circadian pattern of spirometeric parameters and exploring their physiological basis, further study with multiple recording in a day is warranted.
Total No. of subjects (n) = 161. Data presented are mean ± SD, # represents significant difference (p<0.05) using paired t-test,* represents highly significant difference (p<0.001) using paired t-test