Facilitated Eruption of an Impacted Premolar 8 Years Post-eruption Timing- Think before You Treat!!!
Neha1, Tulika Tripathi2, Priyank Rai3, Navneet Singh4
1 Senior Research Associate, Department of Orthodontics, Maulana Azad Institute of Dental Sciences, Delhi, India.
2 Professor and Head, Department of Orthodontics, Maulana Azad Institute of Dental Sciences, Delhi, India.
3 Professor, Department of Orthodontics and Dentofacial Orthopedics, Maulana Azad institute of Dental Sciences, Delhi, India.
4 Senior Resident, Department of Orthodontics, Maulana Azad Institute of Dental Sciences, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Neha, AK-30 Shalimar Bagh, New Delhi-110088, India. E-mail : augustneha@yahoo.com
The treatment planning of impacted teeth usually involves surgical intervention for bringing about its eruption with traction. But a thoughtful analysis in such cases looking at the possible aetiology may save the complexity of therapy. The present case demonstrates the importance of correct diagnosis in resolving impaction wherein an impacted mandibular second premolar was made to erupt using a simple removable appliance 8 years after its normal range of eruption timing.
Impaction, Mandibular second premolar, Non surgical disimpaction, Removable appliance
Case Report
A 20-year-old female was referred to the Department of Orthodontics with the concern about missing mandibular second premolar on the left side. The patient had a history of trauma in which she had lost her lower incisors and was undergoing implant therapy for the replacement of the same. There was no other significant medical history.
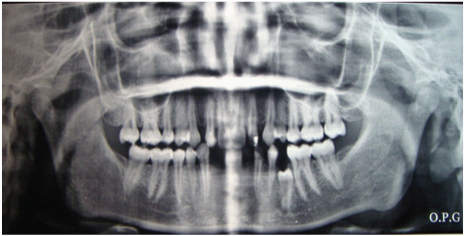
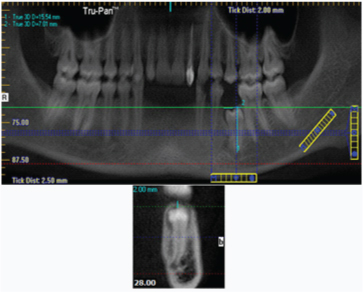
Clinical examination of the patient revealed bilateral class II molars (end on) with spacing present between the upper lateral incisors and canines on both sides [Table/Fig-1]. The upper lateral incisor and the lower canine on the left side were carious exposed. There was no orthodontic concern other than the missing lower left second premolar. The OPG of the patient was available for examination and it revealed that the lower left second premolar was impacted [Table/Fig-2]. A careful examination of the radiograph was done and it was found that the tooth was locked under the bulge of the first molar.
Pre treatment photograph showing missing mandibular second premolar on left side

Pre treatment OPG showing impacted left mandibular second premolar being locked under the mesial bulge of permanent first molar
Further, the Denta Scan of the patient was also available as the patient’s bone level had to be assessed for implant placement. A slice was taken with the help of the software at the distal aspect of the impacted Premolar [Table/Fig-3]. The mesial molar bulge was clearly evident over the occlusal aspect of the impacted premolar impeding its eruption. The impacted tooth was rotated by 90° but it had a favourable axial inclination. The root formation of the premolar was adequate though the apical closure had not taken place. The distance for unlocking the tooth from under the mesial contour of first molar was also assessed through the software to be 2 mm. Thus, in order to allow the premolar to erupt the first molar had to be distally inclined by 2 mm. Also, the impacted tooth had a favourable depth of impaction and clinically adequate space was available for its alignment. Hence, it was decided to allow tooth eruption by unlocking it from below the molar bulge by changing the inclination of the lower first molar. As the amount of tooth movement required was not much and the patient was unwilling for a fixed mechanotherapy, a removable expansion appliance was chosen for the purpose.
CT slice showing the left mandibular first molar obstructing the second premolar
An appliance was designed for the lower left quadrant with clasps on the first premolar and first molar to be separated by expansion screw [Table/Fig-4].
The removable appliance in place for distal tipping of the first molar. (Note- the prominence of second premolar under gingiva as the expansion appliance has been activated. The arrow points to the jackson’s expansion screw in the appliance which is slightly lifted due to wide opening of the mouth for taking the photograh)
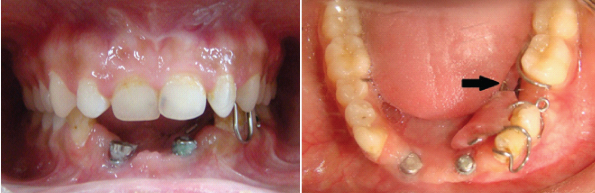
The patient was instructed to activate the screw by half a turn every third day. After 2 months a prominent bulge was evident in the region of the impacted tooth with only gingiva covering the crown of the tooth [Table/Fig-5].
The impacted tooth merely covered by soft tissue with adequate space in the arch for eruption
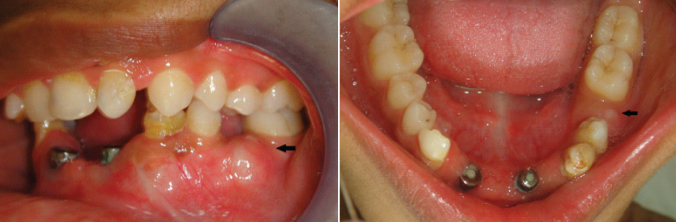
Hence, as the first molar tipped distally (along with mesial movement of the first premolar) with the activation of the expansion screw, the underlying impacted tooth was relieved from the obstruction in the path of its eruption. At this stage it was decided to remove the soft tissue covering the tooth with help of laser for bonding an attachment to hasten its eruption [Table/Fig-6].
Use of laser for removal of soft tissue covering the impacted tooth and bonding of attachment for traction

Due to rotation of the tooth the mesial surface was approachable for bonding of an attachment. Another appliance was designed with a helix at occlusal aspect of the impacted tooth for the attachment of elastics for applying traction to the premolar [Table/Fig-7].
Removable appliance with a helix for attachment of elastic

The appliance covered the occlusal aspect of the remaining dentition which not only enhanced the stability of the appliance but also maintained the corrected inclination of the molar. As the distance from the helix on the lower appliance to the tooth reduced with the eruption of the tooth, a helix made in stainless steel wire was bonded to opposing upper premolars [Table/Fig-8].
Traction through the bonded helix in the opposite arch

Elastic traction was applied to lower premolar by means of this bonded attachment for a short duration of 15 days till the buccal cusp of the lower first premolar erupted to occlude with its opposing tooth [Table/Fig-9].
Buccal cusp of the impacted premolar reaching the occlusal plane

However, though the rotation was severe, the patient was unwilling for any fixed appliance. The alternative was to either fabricate a crown or simply alter the morphology of the disimpacted tooth by means of composite build up. The patient chose the second option of minimal reduction/alteration of the tooth structure as she already had undergone elaborate prosthetic procedure. Hence, the composite build up of the tooth was done to simulate the normal morphology of a mandibular second Premolar [Table/Fig-10]. The total treatment time was 4 months and as no derotation of the tooth was done, there was no need for any long term retention of the corrected tooth.
The disimpacted tooth after alteration of morphology by composite build up

The patient simultaneously got the missing teeth replaced affixed to the implants in the Department of Periodontics. However, a revision was requested for improvement in the prosthesis due to metal show, poor morphology and shade of the prosthesis.
Discussion
An impacted tooth is one that is embedded in the alveolus so that its eruption is prevented or the tooth is locked in position by bone or the adjacent tooth/teeth [1]. Lower second premolars account for approximately 24% of impactions, excluding third molars [2]. The prevalence of premolar impaction has been reported to be 0.1% to 0.3% for maxillary and 0.2% to 0.3% for mandibular premolars [3].
Premolar impactions may be due to local factors such as mesial drift of teeth arising from premature loss of primary molars; ectopic positioning of the developing premolar tooth buds; or pathology such as inflammatory or dentigerous cyst [4]. The treatment modalities for an impacted tooth include observation, intervention, relocation and extraction [5]. The usual approach in resolution of impaction involves surgical exposure followed by orthodontic therapy for its alignment [6]. The decision regarding the choice of therapy for impacted premolar depends upon the aetiological factors, space requirements, need for extractions of primary molars, degree of impaction and root formation of the impacted premolar [7,8].
In the present case the most significant observation was the need to locate the cause of impaction which was the mesial inclination of the lower first permanent molar. This could have been due to pre mature loss of the deciduous second molar. A proper diagnosis, thus, averted the need for the surgical exposure of the site and led to simplification of the therapy by involving removable appliances and minimal soft tissue exposure. Another case of resolution of premolar impaction by a conservative approach has been described by Collett in which removal of a deciduous second molar was followed by the eruption of an unfavourably inclined premolar located deep within the alveolus [7]. The only intervention carried out was the extraction of the deciduous tooth after which 16 months long observation period was allowed for the impacted tooth to erupt to the occlusal plane.
Aizenbud et al., have described a case of impacted mandibular second premolar with a tilt of 90o which was surgically exposed after extraction of overlying deciduous tooth followed by its orthodontic extrusion and alignment [9]. McNamara & McNamara have described two cases of mandibular Premolar impactions, one in 33-year-old female where surgical intervention was essential to allow for orthodontic alignment of the tooth [5]. Cases like these present the other extreme of therapy for alignment of impacted premolars. Also, in the current case, the rotation was so severe that its correction and long term retention was also extremely challenging. Thus, mere recontouring of the tooth morphology could restore both the function and aesthetics without jeopardizing the vitality of the tooth or long term success of the therapy.
The current case demonstrates the importance of judicious planning after a thoughtful analysis of the diagnostic records and stresses the individualistic approach in management of any case. The correct diagnosis greatly simplified the mechanics and an impacted tooth was allowed to erupt just by relieving it from under the bulge of the adjacent molar. The case is also unique as it proves that even the impacted teeth have eruption potential provided the impediment to their natural eruption is identified and managed successfully. Even after 8 years of the normal eruption timing, the tooth demonstrated eruptive movement as soon as the molar that obstructed its path was corrected. An orthodontic force was added just to reduce the time taken by it to take its occlusal position after it was visible under the gingiva.
Conclusion
The diagnostic records should be carefully assessed prior to beginning of any case so that successful management can be done with the most conservative mechanics as a seemingly complex case of impaction was simplified with help of a simple removable appliance without subjecting the patient to any elaborate surgical or orthodontic procedures.
[1]. Friel JP, Dorland’s llustrated Medical Dictionary 1974 25th edPhiladelphia, Pa, USAWB Saunders [Google Scholar]
[2]. Alling CC, Catone GA, Management of impacted teethJ Oral Maxillofac Surg 1993 51(Suppl 1):3-6. [Google Scholar]
[3]. Thilander BN, Myrberg N, The prevalence of malocclusion in Swedish school childrenScand J Dent Res 1973 81(1):12-21. [Google Scholar]
[4]. Rubin DM, Vedrenne D, Portnof JE, Orthodontically guided eruption of mandibular second premolar following enucleation of an inflammatory cyst: Case ReportThe Journal of Clinical Pediatric Dentistry 2002 27(1):19-23. [Google Scholar]
[5]. McNamara C, McNamara TG, Mandibular premolar impaction: 2 case reportsJ Can Dent Assoc 2005 71(11):859-63. [Google Scholar]
[6]. Becker A, The orthodontic treatment of impacted teeth 1998 LondonMartin Dunitz [Google Scholar]
[7]. Collett AR, Conservative management of lower second premolar impactionAust Dent J 2000 45(4):279-81. [Google Scholar]
[8]. Kalia V, Aneja M, Mandibular premolar impactionScholarly Research Exchangedoi:10.3814/2009/821857 [Google Scholar]
[9]. Aizenbud D, Levin L, Lin S, Michtei EE, A multidisciplinary approach to the treatment of a horizontally impacted mandibular second premolar: 10-year follow-upOrthodontics : the art and practice of dentofacial enhancement 2011 12(1):48-59. [Google Scholar]