The prevalence of Autism Spectrum Disorders (ASD) has increased substantially over recent decades, with a median global prevalence estimate of 62/10,000 [1]. There are several regional variations in the prevalence estimates and most data comes from United States of America and European nations [1]. The reported prevalence is generally lower in southeastern and other Asian countries, but one study from Sri Lanka estimated prevalence of 100/10,000, comparable to other studies [2]. Australia Bureau of Statistics reported an overall prevalence of ASDs at 0.5 percent in 2012, a 79% increase since 2009 [3].
The landscape of ASDs is changing and recently Diagnostic and Statistical Manual of Mental Disorders (DSM-5) have made changes in definition of these disorders [4]. The specific diagnostic categories of DSM-IV-TR have been combined into a single broad category of ASD and the three dimensions of DSM-IV-TR definition are collapsed into two symptom dimensions of Social Communication and Interaction (SCI) and Restricted Repetitive Behaviour (RRB). Thus it is vital for health professionals providing services to children, adolescents and adults with ASDs to engage in ongoing educational programs. This is relevant for a variety of primary health providers (GPs, Paediatricians and Nurses) as the responsibility to facilitate the process of referral to specialist services often rests with them. Several guidelines such as the National guidelines for health screening and surveillance of young children with Rourke Personal Health Record in Canada, Bright Futures guidelines in North America, four year old Healthy Kids check in Australia, and the evolving Child Health Promotion program in the United Kingdom are suggested to be used by these providers [5–8].
Although the increasing awareness of ASDs has resulted in a trend towards a younger age at diagnosis [9], often delays are also reported in diagnosis of these disorders [10]. More opportunities for enhancing the awareness of GPs for developmental disorders by ongoing structured educational activities are needed [10–14]. Presently there are no specific educational models for ASDs for GPs. However, it is known that educational programs for primary health care providers need to put emphasis on the referral process of using multidisciplinary services incorporating psychologists, paediatricians, psychiatrists, and other allied specialists for expediting diagnosis and management of ASDs. Generally the referral source for this process is from a GP to paediatricians and psychiatrists, who work collaboratively with psychologist, speech pathologists and occupational therapists [Table/Fig-1]. Therefore, GPs provide important primary care services for children with these disorders both pre and post diagnosis, especially as families often have longstanding trusting relationships with them, and make frequent primary care visits for guidance [15–17].
We have highlighted the perceptions, relevance and educational needs of GPs regarding ASDs using exploratory analysis of survey data of GPs in New South Wales (NSW) in Australia in this journal [18]. We also demonstrated in earlier report that there are two broad educational domains – general knowledge and surveillance – for ASDs for GPs [18]. In this paper, we provide further evidence of these two domains to focus on education, and develop a theoretical framework to guide the development of educational programs regarding ASDs for primary health care workforce.
Materials and Methods
(1) Confirmatory Factor Analysis
We conducted Confirmatory Factor Analysis (CFA) of the original survey data to test the reliability of dimensions. The original survey data set consisted of responses from 191 GPs to 14 True/False knowledge questions on ASDs. This state wide postal survey was conducted in NSW in 2011. Ethical approval for this survey was obtained from the Northern Sydney Central Coast Area Health Services Human Research Ethics Committee (NSCCAHS HREC-1102-076M). Two questions (Q3 and Q5) in the initial questionnaires were rogue items, and dropped as described in the earlier report [18]. Since many GPs did not attempt all twelve questions, for the purposes of CFA, list wise deletion of missing cases was done. The final data set from this 2011 survey consisted of responses from 152 GPs with answers to all the 12 questions. The true responses were coded 1 and wrong answer as 2 for analysis. CFA was used to reduce the number of observed variables (in our study the 12 questions) into a smaller number of latent variables (two broad domains) [19]. We checked the robustness of the two factor models using factor loadings and co-variances and the standard model fit indices such as Root Mean Square Error of Approximation (RMSEA,<0.06), Chi square (χ2), Akaike Information Criterion (AIC, smaller the better), etc. as described elsewhere [19,20]. IBM SPSS AMOS, Version 22.0, Armonk, New York was used for the analysis.
(2) Literature Review
We further support this framework with a systematic review of literature, and use a life cycle approach to provide guidance on the likely contents of educational programs regarding ASD’s. The “Life cycles approach” is used to avoid “problem shifting” across different stages of life and from present to future, incorporating various life cycle vulnerabilities [21]. In the context of ASDs, life cycle approach would mean identifying the signs of ASDs early and facilitate intervention during early childhood, supporting and empowering the providers and families for education of children during school years and vocational training during youth. The unique co-morbid medical conditions which can emerge with these disorders during the phases of toddler years, childhood, youth, adults and old age are also likely to be addressed using this approach. Life cycle approach for these disorders would provide continuity of care and longitudinal follow up of children, especially in a general practice and primary care setting. This approach has been proposed to be useful in other areas of health such as to improve perinatal health. Community based interventions integrating neonatal and maternal care using life cycle approach has been shown to reduce maternal morbidity (RR 0.75; 95% CI 0.61 to 0.92) and neonatal and perinatal mortality (RR 0.76; 95% CI 0.68 to 0.84; RR 0.80; 95% CI 0.71 to 0.91) [22].
A search of databases PubMed, Google scholar and PsychINFO was done up to week one of January 2014. Except for PsychINFO, no restrictions were placed on the initial date of data search. The search strategies for each database were achieved using an iterative process to give the maximum number of citations relevant to the study objectives. Abstracts related to ASDs and primary care, focusing on early identification, education, and management issues were extracted and read, until no new themes emerged. Practice guidelines for early identification of ASDs from professional organizations were also read. The lack of guidance on the best educational approach as well as the specific topics for educational purposes for GPs particularly role of GPs in ongoing management was evident in these guidelines. Thus articles for other neurodevelopmental disorders and intellectual disability, highlighting perceptions of stakeholders for enhancing knowledge, and articles describing educational approaches for primary health care providers, were included. Articles which specifically highlighted medical students and resident teaching on child development issues were also included. The search strategy and number of citations extracted from each database are presented in [Table/Fig-2]. A qualitative synthesis of the literature using a deductive approach, to identify contents of education for ASDs in the two domains of general knowledge and surveillance was conducted. Similarly contents relevant for education regarding ASD’s were synthesized for each life stage.
Search strategy used for review of literature.
| Database* | Search strategy | Citationsreceived | Total abstractsread (includedall databases) |
|---|
| Google scholar | Knowledge OR Education AND Autis* AND Pediatrician* OR GP OR “Family Physicians” | 1410 | 412 |
| PubMed | Education OR Knowledge ANDAutis* | 3288 | |
| PsycINFO(1987–week1 Jan 2014) | Education OR KnowledgeAND Autis* OR “Primay Care”OR “General Practitioners” OR“Family Physicians” OR Paediatricians and Child* | 3579 | |
*Except PsycI NFO, all other database search was conducted from database inception up to week one of January 2014
Results
Confirmatory Factor Analysis
The 12 questions developed for the initial GP survey are highlighted in [Table/Fig-3]. Overall, the two factor models had much better model fit indices, which lends supports to the two main domains to focus for education [Table/Fig-4]. An 8-items two factor model, had best model fit indices [Table/Fig-4].
True/False questions developed for the original survey with GPs in the two relevant domains.
| Question No. | Question |
|---|
| General knowledge dimension |
| Q1 | The prevalence of Autistic Disorder in Australia ranges from 8.5 to 15/10,000 for pre-school children. |
| Q2 | A diagnosis of Autistic Disorder can be made in a language impaired child. |
| Q4* | Toddlers with Autistic Disorders often have suspected deafness and delayed speech development. |
| Q6* | Modified Checklist for Autism in Toddlers (M-CHAT) is a useful screening tool for Autistic Disorders. |
| Q7 | Boys with Autistic Disorder should be explored for a possibility of Fragile X syndrome. |
| Q8 | The risk of Autistic Disorder in siblings is increased 20 to 40 fold to that of the general population. |
| Q10* | The only evidence based treatment for Autistic Disorders is an early individualized educational based program. |
| Q12 | MMR vaccine should be deferred in toddlers suspected to have Autistic Disorders. |
| Q13* | Use of visual cues should be discouraged to improve verbal communication in children with Autistic Disorders. |
| Surveillance dimension |
| Q9* | All children with Autistic Disorders have low IQ. |
| Q11* | Challenging behaviours in children with Autistic Disorders can be managed only with medications. |
| Q14 | More pre-schoolers than school aged children have Autistic Disorders. |
*Bayesian estimation method identified these as the most relevant items for the two factors
Model fit indices for one and two factor structures.
| Factor structure | χ2 | df | p-value | CFI | RMSEA | TLI | AIC | BCC | BIC | ECVI |
|---|
| 2-factor12 items | 55.86 | 53 | 0.37 | 0.95 | 0.019 | 0.94 | 105.9 | 110.6 | 181.5 | 0.7 |
| *2-factor8 items | 18.4 | 19 | 0.49 | 1.0 | 0.000 | 1.02 | 52.4 | 54.6 | 103.8 | 0.35 |
| $2-factor6 items | 8.9 | 8 | 0.35 | 0.96 | 0.03 | 0.93 | 34.9 | 36.2 | 74.2 | 0.23 |
| §One factor12 items (knowledge) | 54 | 72.5 | 0.047 | 0.70 | 0.048 | 0.64 | 120.5 | 125.1 | 193.1 | 0.8 |
Df-Degrees of freedom, CFI-Comparative Fit Index, RMSEA- Root Mean Square Error of Approximation, TLI-Tucker-Lewis Index, AIC- Akaike Information Criterion, BCC–Browne-Cudeck Criterion, BIC-Bayes Information Criterion, ECVI-Expected Cross-Validation Index
* Q 2 & Q12 were excluded from this model
$ Q4, 6, 9, 10, 11, 13 were included in this model
§ Only 1, one-factor model indices are presented
Contents for Education in Two Domains
The items on the general knowledge and surveillance domains from the literature review are highlighted in [Table/Fig-5]. Alerts and red flags for ASDs, knowledge of simple surveillance tools, communication of diagnosis with parents, referral pathways particularly to speech pathologists before a formal diagnosis is confirmed, and appreciation of vulnerabilities for identifying supports were important in the general knowledge domain, while supporting the families through transition points such as from pre-school to school entry, secondary school and adolescence, role of psychopharmacology such as medications for sleep issues, and for common co-morbidities of anxiety were important in the surveillance dimension.
Summary of main studies and emerging themes for education in the two domains
| Study reference | Themes |
|---|
| General knowledge | Surveillance |
|---|
| Barbaro and Dissanayake [35],Carbone [36] | Alerts and red flags for ASDsChild health surveillance tools within local contextsKnowledge and limitations of screening tools | Supporting parents in the time between presentation, referrals and intervention |
| Hardy et al., [37],Carbone [36], Buie [38], Bejerot [39] | Clear ability to communicate with parents and specialists regarding concerning features of ASDs, particularly, social communication deficits, language delays, imaginative play and repetitive behaviours | Addressing co-morbid medical and psychiatric conditionsGastrointestinal (constipation, diarrhoea, food allergies)Sleeping issues (role of melatonin)Feeding issues (often secondary to sensory sensitivities)Dental issuesAnxiety, depression |
| Sanders et al., [32], Hillman et al [40] | Links with paediatricians, psychologists, allied health professionals, and tertiary child development units guiding the initial referral process | Supporting challenging behavioursTriple-P Parenting programs |
| Sevilla-Dedieu [41],Sabo [42] | Knowledge of parent groups with ASDsAdvocacy groups, web based tools for parental education regarding ASDs | Role of psychopharmacologyIndicationsSide effectsMonitoring of medications prescribed by specialists |
| Umbarger [43] | Discussion of investigations (such as Fragile X), Family historyPotential role of genetic environment- interactionsReferral for Genetic counseling | Understanding role of Complementary and Alternative MedicationsTypesEvidenceBalancing evidence with costs and parental choices and wishes |
| Martinez [44]Volkmar et al., [45] | Vaccination advice, safety concerns addressed | Supporting positive coping strategies after diagnosis (hope, adjustments, positive discussions with families and friends)Identifying maternal depression and parental stressors in the context of ASD in childrenExploring stigmatisationExploring siblings and providing information on sibling support groups |
| Harmsen et al., [46]Van Wieringen et al., [28]Volkmar et al., [45]Ewart [26], Solish [47] | Appreciation of challenges for disparities in access and identification of vulnerabilities (such as immigrant families, economic vulnerabilities, parents with substance abuse, domestic violence and mental health concerns) | Supporting families make informed choices of interventionStrengthening the belief of the families in the early intensive behavioural programSupporting cultural barriers and enablers for intervention and progress |
| Hastings et al., [30] | Discuss issues about child safety | Collaborate with specialist teams for transition planning of services at critical points such as preschool to school, primary school to secondary schoolSupporting discussion of schooling options formulated by multidisciplinary teams and specialists |
| White et al., [48], Marriage et al., [49],Whitby [50] | | Discuss language outcome of preschoolers with ASD in school age, Changes in intellectual abilities of preschoolers in school aged children, Adult functioning of children diagnosed with ASD, Academic achievement of high functioning autism |
Contents for Education Across the Life Cycle
The relevant contents for education regarding ASDs across the life course are highlighted in [Table/Fig-6]. The important issues during life cycle approach which need to be emphasized include:
Educational contents across the life cycle
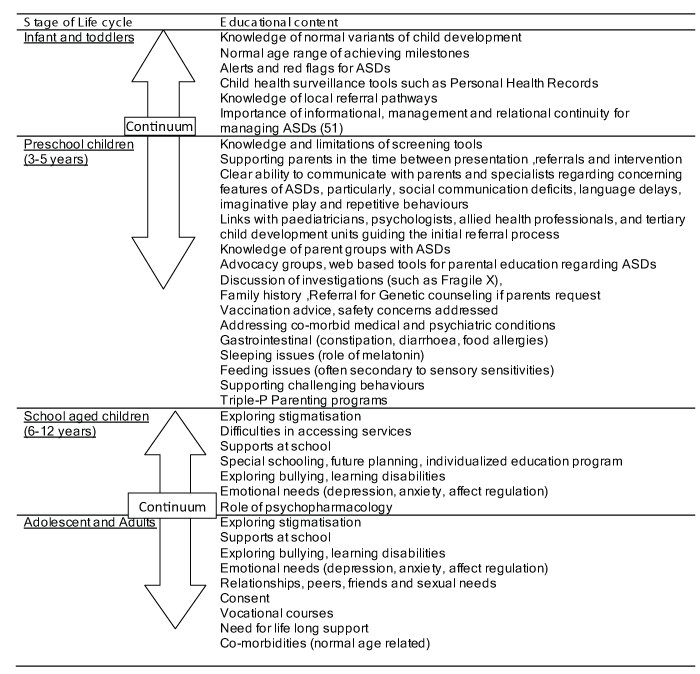
Early childhood (toddler years) – Screening and assessment including the importance of referrals to allied health professionals particularly speech and language pathologists as communication impairments is one of the main issue in these disorders. Generally a need for Melatonin for sleep disorders during this age group
School entry – Awareness of choice of special schools available, educational needs of children in collaborations with specialists to assist this transition for families
Transition to high school and the challenges particularly the exacerbation of challenging behaviours secondary to anxiety. The role of Selective Serotonin Reuptake Inhibitors (SSRI’s) for managing anxiety and atypical antipsychotics for managing aggression. Adolescent and youth- challenges of body image and sexuality
Adults and Old age – vulnerability and further social isolation
Discussion
This paper highlights the contents which are likely to be useful for education of primary health care workforce particularly GPs and child and family nurses, using two broad domains and a life cycle approach [Table/Fig-5,6]. This approach should be useful for educators of primary health workforce to develop more structured learning activities for ASDs. These could take the form of a case presenting for the first time with concerns of developmental disorders or a child with a known diagnosis of ASD and now being followed up in the general practice setting. The continuum of care scenarios could include various exacerbations related to Behaviour, family dynamics and medical problems [Table/Fig-7].
| Box 1: Examples of three case scenarios within domains of education highlighted in this paperCASE SCENARIO 1A 25 year old mother of three children, well known to you since last about 10 year’s presents to your practice with concerns regarding his youngest 3 year old son. Her main concern is that his son has only some single words in his vocabulary and does not seem to follow her instructions.
1. What further questions are most relevant to ask this mother within your 20 minute consult?
2. What further observations regarding mother and his son can you make in the clinic room?
3. You identify some concerns based on above two questions, how would you communicate your concerns to this anxious mother
4. What resources are available to you for managing this child?CASE SCENARIO 2
A 40 year old mother of Indonesian background, known to your practice presents with his four year old for immunizations. You note the child to have limited awareness of his environment. You flag your concerns with her mother, and she discloses that he has been recently diagnosed with an Autism Spectrum Disorder (ASD). She seeks further advice to you regarding his sleep.
1. How would you seek further information from his mother regarding ASD?
2. What are the relevant questions to ask regarding his sleep?
3. What medications could be help his sleep?CASE SCENARIO 3
A 33 year old single mother of five children, presents to you practice with his 10 year old son for the first time after recently moving into your area. She raises concern about his son’s increasing disruptive behavior at his new school. On further probing she reveals that his son was diagnosed with ASD at age of three years and was attending a special school before moving into this area. He now attends year 7 at a mainstream school.
1. How and where would you seek further information?
2. What are the likely causes of his disruptive behavior?
3. How would you support this single mother?
4. What other resources are available to you to manage this boy and family? |
Although the contents could be argued to be specialist knowledge, scenarios in the general practice are not different and a close collaboration with specialists would be expected for primary health providers for patients with these disorders.
Validity of Two Educational Domains from Literature
As evident from the literature the items in the General knowledge domain should focus on early identification, and emphasize the role of GPs in the initial phases of contact with the families, when concerns of ASDs in young children are raised [Table/Fig-5]. During this phase there is evidence for the providers to be aware of normal variations in child development and the red flags for these disorders such as does not respond to his name, does not use eye contact or gestures, does not point to show things and loss of language or social skills [23]. Robins demonstrated the utility of the Modified Checklist for Autism in Toddlers (M-CHAT) by screening 4797 toddlers and identified 61 children with ASDs in follow up [24].
The ability to communicate identified concerns effectively is equally vital, as these are often raised by parents as an important factor for satisfaction with their GPs. This is shown in a qualitative study of parent’s experiences with the diagnostic process regarding ASDs. Some parents suggested the need for greater professional training about ASDs, in particular, regarding more information to be provided on ASDs and better interpersonal skills of professionals [25].
The theoretical justifications of General Knowledge and Surveillance educational domains and a life cycle approach are elaborated in a qualitative study by Ewart, who has highlighted the process of six stages; a family with a child with an Autism Spectrum Disorder undergoes [26]. These include sequentially from pre-diagnosis and diagnosis, to reactions to diagnosis, adjustments following diagnosis (involving themes of interventions, schooling, and changes in family roles), reactions to these adjustments (involving themes of struggle to accept the diagnosis, stressors of parenting an autistic child, complexity of the disorder, balancing demands, effects on marriage, family, and stigmatization), parents’ increased knowledge, coping and acceptance, and finally concerns and hopes for the future. The items on the General Knowledge dimension are important in the first and second phase, while Surveillance dimension involves the other four phases [Table/Fig-5]. The literature review highlighted that the items in the surveillance domain would be useful once the diagnosis of ASD is made, and a plan for early intervention has been put into place by specialist teams. The needs of these children and families when they become adolescents and adults are also an important area in the surveillance domain.
The care to be delivered in both domains by GPs, often requires an appreciation of family centered model of care. Tisher et al., has identified the main learning objectives for family centered care for GPs, from the feedback sessions of participants in two family therapy courses. The eight identified topics included importance of stressors, genograms, problem clarification, options, involvement of patients, reflection on interventions, and recognition of an interactive cycle and review of treatment [27]. The first four of these topics are relevant in the General Knowledge domain for managing children with ASDs in primary care, while the later four are relevant in the Surveillance dimension. The need for strengthening skills in the delivery of family centered care and increasing collaboration between GPs and mental health professionals has also been shown in a number of other studies [28,29]. Hastings et al., has highlighted the need for GPs to understand the requirements for special education services for children with ASDs [30].
Approaches for Partnership Working Style for GPs
Layiou-Lignos et al., have used principles of adult learning models, a partnership approach to the helping process and combination of the parent adviser and promotional interviewing models for development of skills regarding assessing and supporting early parent-infant interactions. These skills are relevant for providers in their role for the care of children with ASDs [31]. The participation of GPs in a Triple P-Positive Parenting Program in Queensland have been shown to be associated with significant improvement in practitioners’ consultation skills, greater satisfaction with their consultations and high levels of participant satisfaction with the training provided [32].
The topics summarized in [Table/Fig-5,6] can be used to develop True/False, Multiple Choice Questions, Multiple Response Questions, and brief case vignette scenarios for educational and evaluation activities regarding ASDs. These activities will need to take into account the roles which primary care providers play within the broader health systems of their countries, and their local contexts of health service delivery.
Limitations and Implications for Future Research
The power of CFA for two factor solution with 12 items is limited by small sample size. McCallum and colleagues have suggested a sample size of 200 for degree of freedom of 55 to achieve a power of 0.80 [33]. Although our study is underpowered by small sample size and the removal of missing cases, the theoretical relationships between the general knowledge and surveillance dimensions have remained unaffected. The success and utility of the suggested approach need to be tested in further prospective studies with GPs.
In a survey, Heidgerken et al., has demonstrated differences in knowledge regarding ASDs among autism specific professionals to primary care providers including family physicians, pediatricians and neurologists [34]. Further research is needed to understand what differences exist between knowledge in the two domains described in this paper, among different type of health professionals. Although this paper provides a framework for developing curriculum for ASDs, it does not comprehensively cover aspects for contemporary medical education such as the process of curriculum development for GPs regarding education for ASDs. Further interventional research on the methods of delivery of educational programs or assessment aspects for ASD’s are also needed.
Conclusion
It is already known that there is an increased need for education for GPs to facilitate early identification and referral for children with Autism Spectrum disorders. The present study adds to the existing literature by highlighting the broad dimensions for knowledge as well as the likely items for development of educational activities specific for early identification of children with ASDs, and the ongoing need of surveillance of these children at primary care. This is important as specialist autism diagnostic units rarely provide routine follow up, after the diagnosis of ASD has been confirmed, and several barriers exists for accessing specialist Paediatricians and Psychiatrists such as costs, waiting times and vulnerabilities of many families. The educational programs around these two domains are likely to be transferable in a variety of local contexts and systems, and will hopefully result in improved knowledge of GPs, increased parental satisfaction and improved outcomes for children with ASDs.