Oral submucous fibrosis (OSMF) is a chronic progressive, insidious disease characterized by blanching, stiffness, trismus and burning sensation affecting the oral, oropharyngeal and sometimes the oesophageal mucosa causing changes similar to those of systemic sclerosis (scleroderma) but limited to oral tissues [1]. The disease is seen among people who chew areca nut and affects population mainly from the Indian subcontinent and from many parts of South-East Asian countries such as Pakistan, Bangladesh, China, Taiwan [1,2]. This chewing habit has become a compulsive act, in spite of known association with oral cancer and no nutritional status. The ease of commercial availability and wide media advertisements has led to its popularity among the youth and consequently, manifestations of OSF are on the rise [3]. The disease is accompanied with juxta-epithelial inflammatory reaction and fibroelastic changes in the lamina propria, sometimes followed by and/or associated with vesicle formation, with epithelial atrophy that causes stiffness in the oral mucosa, leading to trismus and patient becomes unable to eat which influences the general health of the individual [4]. Nutrition and oral health are interrelated. Nutrition is a major factor in infection, inflammation and prognosis of a disease [5]. Body mass index (BMI) is a simple, inexpensive and non invasive surrogate measure of body fat. In contrast to other methods, BMI relies solely on height and weight and with access to the proper equipment, individuals can have their BMI routinely measured and calculated with reasonable accuracy [6]. Thus, the present study was conceded in Dental College, to evaluate the correlation of duration and frequency of habits on clinicopathological manifestations of OSMF, site analysis and relation with BMI in Sri Ganganagar, Rajasthan, India.
Materials and Methods
The present prospective study comprised of 50 patients, 37 males and 13 females of OSMF who were diagnosed clinically with confirmation of diagnosis through histopathological examination. The study was undertaken during the period of December 2013 to January 2015 in the Department of Oral Medicine and Radiology and the patients aged 10 to 60 years were selected randomly among the outpatients visiting the department. A formal ethical clearance to conduct this study was obtained by the ethical committee of Maharaja Ganga Singh Dental College and Research Institute. A detailed case history of the patients along with information regarding their habits (nature, duration, frequency of chewing or placement of betel nut, smoking, alcohol, etc) was taken and habit index (gutkha index) was calculated by multiplying duration and frequency. BMI was calculated by dividing weight in kilograms and height in centimetres of the patient and was recorded on standard proforma. Patients selected for this study were explained in detail about the condition affecting their oral cavity and procedure that they are subjected to. A formal informed written consent was obtained from all of them. Inclusion criteria of the study were patients with definitive diagnosis of OSMF, both clinically and histopathologically. Exclusion criteria was patients with history of diabetes, hypertension, anaemia, jaundice, liver or kidney disorders or other systemic diseases and carcinoma elsewhere in the body.
In patients with OSMF, site of involvement (buccal mucosa, labial mucosa, tongue, palate and uvula) and distribution of the vertical fibrous bands were recorded. The distance between the incisal edge of upper and lower central incisors with the mouth fully open was measured using a graduated ruler and geometric divider. Patients were categorized into three clinical stages of OSMF on the basis of mouth opening [Table/Fig-1] according to classification given by Kiran Kumar et al., [7,8]:
Method of measuring mouth opening

Stage I: Mouth opening >45 mm.
Stage II: Restricted mouth opening 20 to 44 mm.
Stage III: Mouth opening <20 mm.
After establishing the clinical diagnosis of OSMF, the patients were subjected to routine haemogram (HB%, TLC, DLC, CT, BT and ESR) to rule out any systemic ailment. This was followed by a histopathological confirmation of diagnosis by performing an incisional biopsy of the lesion. The patient was seated comfortably on the dental chair. Patient was advised to swish the mouth with water and 0.2% chlorhexidine mouthwash for 1-2 minutes. Biopsy was taken from the most representative area of the lesion [Table/Fig-2]. A topical antiseptic (betadine-iodine solution) was applied on the site of biopsy followed by topical anaesthetic at the site of injection. Local anaesthesia was achieved by infiltration of 1.5ml of 2% of lignocaine hydrochloride solution at least 1cm away from the lesion, taking care not to deposit it directly into the area to be biopsied. The specimen was removed from the mouth with closed scissor blade and placed in the fixing solution (Formalin 10%). The specimen was processed and haematoxylin and eosin sections were studied under microscope. Histopathological grading was done according to classification given by Pindborg JJ and Sirsat SM into very early, early, moderately advanced and advanced stage [8]. After the diagnosis was established, the patient was enlightened about the precancerous nature of the disease and was then counselled to discontinue the use of areca nut in all preparations available in different forms in the market. The patients with OSMF were divided into clinical and histopathological groups according to grading and staging of the disease.

Statistical Analysis
All the variables in the study were statistically analysed using SPSS-16. p-value <0.05 was considered as significant value and chi-square test was used to determine the level of significance.
Results
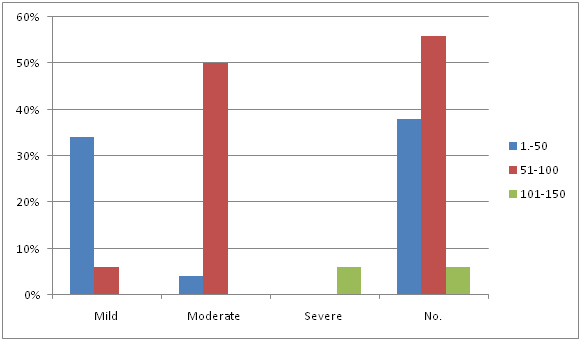
All patients in the present study had a positive history of areca nut chewing either in raw form as a quid or in a commercial preparation such as gutkha and pan masala. Demographic data revealed [Table/Fig-3], maximum number of patients were in age group 20-34 years and minimum were in age group 10-19 years. Seventy four percent of the patients were male and 26% were females. Clinical grading increased with increase in gutkha index [Table/Fig-4,5], out of 19 patients with gutkha index 1-50, 17 were in mild stage, 2 in moderate; out of 28 patients with gutkha index 51-100, 3 were in mild stage, 25 in moderate; out of 3 patients with gutkha index 101-150, all 3 were in severe stage. The severity of stage increased with increase in gutkha index. P-value showed significance of gutkha index with severity (p <0.05).
Demographic data of OSMF patients
| Age group (In Yrs) | Sex | Total |
|---|
| Male | Female |
|---|
| 10-19 | 3 | 1 | 4 |
| 20-34 | 21 | 8 | 29 |
| 35-49 | 5 | 2 | 7 |
| 50+ | 8 | 2 | 10 |
| Total | 37 | 13 | 50 |
Distribution of gutkha index of the OSMF patients with clinical staging
| Clinical staging | Gutka index |
|---|
| 1-50 | 51-100 | 101-150 | Mean ± SD | Total |
|---|
| Mild | 34% | 6% | nil | 7.02±3.04 | 40% |
| Moderate | 4% | 50% | nil | 9.10±3.50 | 54% |
| Severe | nil | nil | 6% | 11.4±3.43 | 6% |
| No. | 38% | 56% | 6% | | 100% |
| % | 38% | 56% | 6% | | 100% |
| p-value | | | | < .05 | |
Distribution of Gutkha index of patients of study group with clinical staging
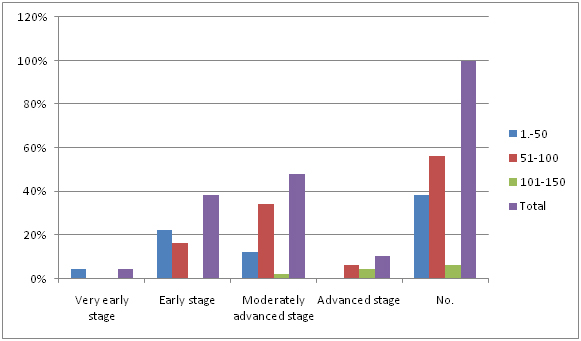
Histological staging showed direct correlation with gutkha index, it increased with increase in gutkha index [Table/Fig-6,7] out of 19 patients with gutkha index 1-50, 2 were in very early stage, 11 in early stage and 6 in moderately advanced stage; out of 28 patients with gutkha index 51-100, 8 were in early stage, 17 in moderately advanced stage and 3 in advanced stage; out of 3 patients with gutkha index 101-150, 1 was in moderately advanced stage and 2 in severe stage. The severity of stage increased with increase in gutkha index. P-value showed significance of gutkha index with severity (p <0.05).
Distribution of gutkha index of OSMF patients with histological staging
| Histological staging | Gutka index |
|---|
| 1-50 | 51-100 | 101-150 | Total |
|---|
| Very early stage | 4% | nil | nil | 4% |
| Early stage | 22% | 16% | nil | 38% |
| Moderately advanced stage | 12% | 34% | 2% | 48% |
| Advanced stage | nil | 6% | 4% | 10% |
| No. | 38% | 56% | 6% | 100% |
Distribution of gutkha index of patients of study group and histological staging
Site analysis showed that buccal mucosa and retromolar area were involved in all the patients, labial mucosa in 88%, soft palate in 80%, uvula in 92%, tongue in 76% and floor of mouth in 46% of patients [Table/Fig-8]. It was found that more than one site was involved in all the patients.
Site analysis in OSMF patients
| Site involved | Number of patients | % |
|---|
| Buccal mucosa | 50 | 100% |
| Labial mucosa | 44 | 88% |
| Soft palate | 40 | 80% |
| Uvula | 46 | 92% |
| Tongue | 38 | 76% |
| Floor of mouth | 23 | 46% |
| Retromolar area | 50 | 100% |
Body mass index analysis revealed that 20 patients with mild clinical staging had normal BMI; out of 27 with moderate clinical staging, 24 had normal BMI, 3 was underweight; out of 3 with severe clinical staging, 1 had normal BMI and 2 was underweight [Table/Fig-9]. BMI and clinical staging of patients with OSMF showed insignificant correlation, however out of 3 patients with severe clinical staging, 2 were underweight.
Distribution of BMI of patients having OSMF with clinical staging
| Clinical staging | Underweight < 18.5 | Normal : 18.5–249 | Overweight25.0–299 | Total |
|---|
| 18.5-21.5 | 21.6-24.9 | |
|---|
| Mild | | 13 | 7 | Nil | 20 |
| Moderate | 3 | 19 | 5 | Nil | 27 |
| Severe | 2 | 1 | | Nil | 3 |
Discussion
OSMF distressing and debilitating disease with malignant potential [1]. Demographic data revealed that maximum number of patients, 29 out of 50 subjects were in the age group of 20-34 years which shows the younger generation is more affected by OSMF. This decade of life can be considered as the stressful period because the people select their career goals and struggle for the establishment at this phase of life. The fast growth of industrialization and urbanization has subjected to physical and mental stress. Humans react to this stress by taking stress-relieving habits such as smoking, alcohol, betel nut chewing, pan chewing, etc. These habits are more hazardous to mankind and leads to detrimental effects on human body other than being addictive [9]. The study exposed that youngsters in the age group of 10-19 years are also being attracted to this deadly habit that could be attributed to lack of awareness, peer pressure, violent marketing policies of these products, failure to provide primary preventive measures and alertness of its association with oral cancer [10].
Seventy four percent of the patients were male and 26% were females. The male to female ratio was 2.8:1 which is quite similar to study carried out Ahmad SM et al., in Patna who reported 2.7:1, Whereas Goel S et al., in a study carried out in Southern Rajasthan reported a male to female ratio of 5:1, Pandya S et al., reported 6.8:1 in Allahabad, Uttar Pradesh [11–13].
Tang JG et al., carried out study in China and also reported male predominance [14]. Similarly in the present study, males were found to be dominating, as they were using gutkha and other related products more because of easy availability in all the places where as females being more conscious about their health and aesthetic value, probably felt uncomfortable to ask the vendors in getting the gutkha products. This is one of the reasons, which may be responsible for a high male to female ratio [11].
In the present study, all subjects presented with a positive history of areca nut chewing such as gutkha and pan masala which is considered as a major causative agent for OSMF. The areca nut (betel nut) component of gutkha or pan masala, especially an alkaloid called arecoline, plays a major role in the pathogenesis of OSF by causing an abnormal increase in the collagen production. This alkaloids undergoes nitrosation reaction and give rise to N-nitrosamine, which is known to have cytotoxic effect [15]. Only small proportion of subjects were indulging in other habits like alcohol and smoking, but they were not showing any significant change in clinical presentation and severity of the disease, which is supported by a study carried out by Gupta PC [16]. Dose-response relationships were observed for tobacco chewing in terms of duration and frequency as clinical grading and histological staging increased with increase in gutkha index. Out of 50 patients 2 patients were having mouth opening <20mm and these 2 patients were in severe clinical staging and advanced histological staging. Bose T et al., carried out a similar study which concluded that habitual users of commercially available areca nut products are associated with an earlier presentation of OSMF than conventional betel quid chewers [17]. Ali FM et al., Reddy V et al., Aher V et al., carried out a similar studies and concluded that the duration and frequency of areca nut product use and type effects incidence and severity of OSMF [2,4,9].
In the present study histological staging showed direct correlation with gutkha index, it increased with increase in gutkha index. The fibroelastic changes are almost entirely due to abnormal accumulation of collagen in the sub epithelial layers, resulting in dense fibrous bands in the mouth. The important histopathological characteristic of OSF is the deposition of collagen in the oral submucosa [15]. Histopathology showed thinned out mucosa and thickened avascular subepithelial connective tissue in most of the cases. Debnath S et al., carried out a study and found that histological stages directly correlated with clinical severity of trismus [18]. On the contrary Pandya S et al., Kumar K et al., Goel S et al., found no correlation between clinical symptoms and degree of fibrosis [7,12,13].
In the present study BMI and clinical staging of patients with OSMF revealed statistically insignificant correlation, however data showed that none of the patient was overweight and those found with normal BMI were more towards lower quartile of the range and 2 out of 3 patients who were categorised in severe clinical grade was malnourished. Thus according to authors the number was very less to predict the statistically significant results which possibly is the limitation of the study. Lower BMI may be associated with lower socioeconomic status and malnutrition due to lower socioeconomic status [6]. However, in the present study all the subjects belong to the same socioeconomic status. In a study carried out by Hashibe M et al., in OSMF patients it was found that BMI was towards lower quartile and inverse relationship was established [19]. Similarly Yallamraju SR et al., carried out a study to evaluate the nutritional status of OSMF patients using mid upper arm circumference (MUAC) as a useful tool and found an inverse relation between MUAC and clinical staging and concluded that patients with OSMF becomes unable to eat due to burning, ulcers, and inability to open mouth, which affects the health of the individual [5].
Site analysis revealed that buccal mucosa and retromolar area were involved sites in all the 50 patients whereas floor of the mouth was the least involved site whereas Pandya S et al., carried out a similar analysis and reported that buccal mucosa was the most common site involved in 66(20.8%) patients followed by palate in 37(17.7%) patients [13]. Buccal mucosa with the retro molar area involvement was found in 27 (3.1%) patients; on the contrary in the present study buccal mucosa along with retromolar area was involved in all the patients. Variation in site involvement is attributed to the habit of the individual as chewing habit varies among individuals, but usually the gutkha or pan masala is placed in the buccal vestibule for about 15 min to an hour and repeated five to six times a day. There occurs a regular contact between the mixture and oral mucosa which results in absorption and metabolism of alkaloids and flavonoids from the stuff. These constituents and their metabolites are a source of constant chemical and mechanical irritation to the oral mucosa [15]. Perara S et al., noted fibrosis-promoting activity of areca nut in mice and reported that the scores on cellularity, inflammation and muscle atrophy were significantly different to the control group [20]. The oral epithelium exposed to areca nut insults showed progressive changes in epithelial thickness resulting in atrophy, increased cellularity of fibroblasts, fibrosis of connective tissue, focal infiltration of inflammatory cells and muscular atrophy.
Dentists play a key role to help the patients become aware of harmful effects of tobacco usage and nicotine addiction. The effects range from mild conditions such as halitosis to life threatening ailments such as oral and pharyngeal cancers. Routine screening camps by dentists along with counselling of patients, tobacco cessation programmes are of utmost importance to protect the society from the grab of this harmful habit and its addiction Dentist during motivation and counselling of patient should take into guidelines of IDA i.e. 5A’s i.e. ask, assess, advise, assist and arrange for habit cessation [21].
Conclusion
The duration and frequency of areca nut product use effects the incidence and severity of OSMF. As the habit index of the patient increases, it affects the clinical staging and histopathological grading of the disease resulting in burning, ulcers, pain and inability to open mouth. Patient becomes unable to eat which affects the overall health of the individual resulting in poor nutritional status and decreased body mass index of the patient. Thus it is important to access the nutritional status to improve the survival rate of patients.