Microfilaria Coexistent with Fibroadenoma – An Unusual Association
Kavita Chandrahas Sane1, Sandhya Unmesh Bholay2, Vaibhav Bhika Bari3, Manoj Narayan Kulkarni4
1 Associate Professor, Deparment of Pathology, Rajiv Gandhi Medical College, Kalwa, Thane, Maharashtra, India.
2 Associate Professor, Deparment of Pathology, Rajiv Gandhi Medical College, Kalwa, Thane, Maharashtra, India.
3 Assistant Professor, Deparment of Pathology, Rajiv Gandhi Medical College, Kalwa, Thane, Maharashtra, India.
4 Assistant Lecturer, Deparment of Pathology, Rajiv Gandhi Medical College, Kalwa, Thane, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vaibhav Bhika Bari, 314, Nav Alankar Apt, Third Floor, Old Mumbai Pune Road, Kalwa, Thane-400605, Maharashtra, India. E-mail : vbbari@gmail.com
Filariasis is an endemic problem in India. Involvement of breast by filariasis is uncommon, but known to occur in endemic areas. However, microfilaria co-existing with neoplastic lesions is very rare. Here we report an unusual finding of microfilaria co-existing with fibroadenoma in a 20-year-old female patient.
Breast, Filariasis, Nematodes
Case Report
A 20-year-old female patient, hailing from Sultanpur, Uttar Pradesh presented with a gradually increasing lump in left breast since 8 months. Patient gave history of low grade, recurrent fever without chills since 2 months. On clinical examination a well defined, non tender, freely mobile lump of 2.5x 2.5 cm was palpable in upper and outer quadrants of the breast. The overlying skin was normal. The lump was not fixed to the skin and pectoralis muscle. No lymph nodes were palpable in axilla. Clinical diagnosis of fibroadenoma was made and Fine Needle Aspiration Cytology (FNAC) was advised.
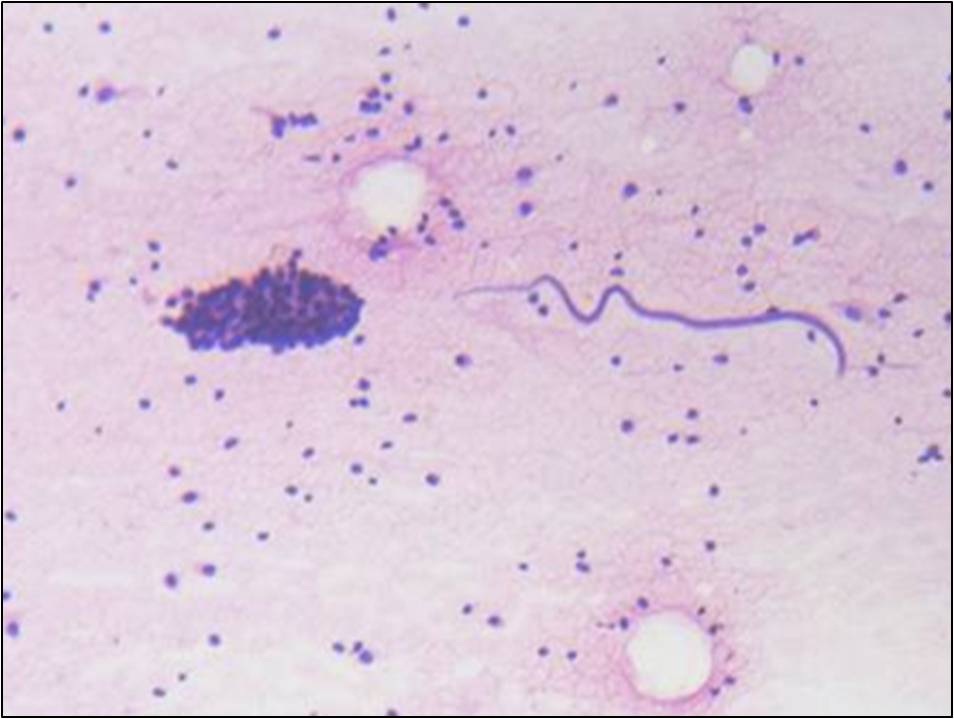
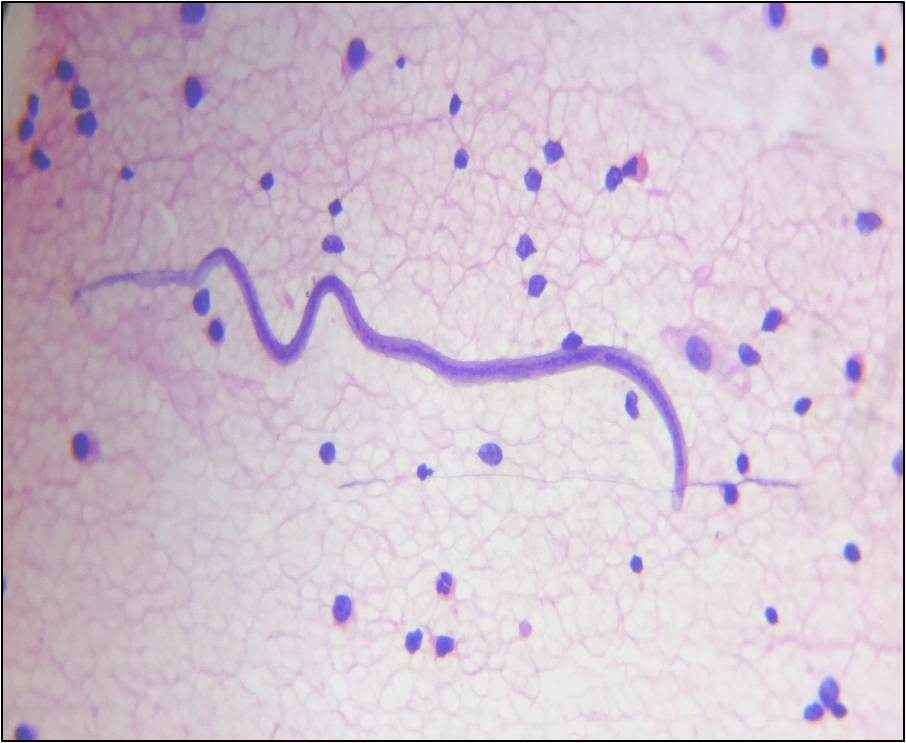
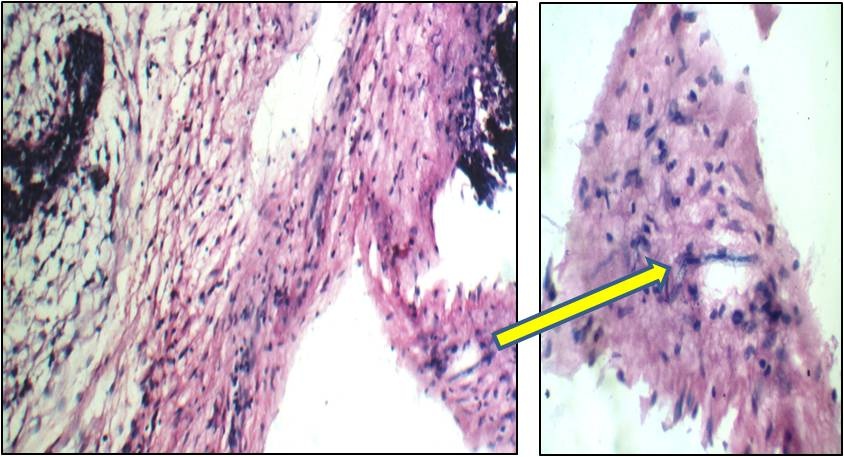
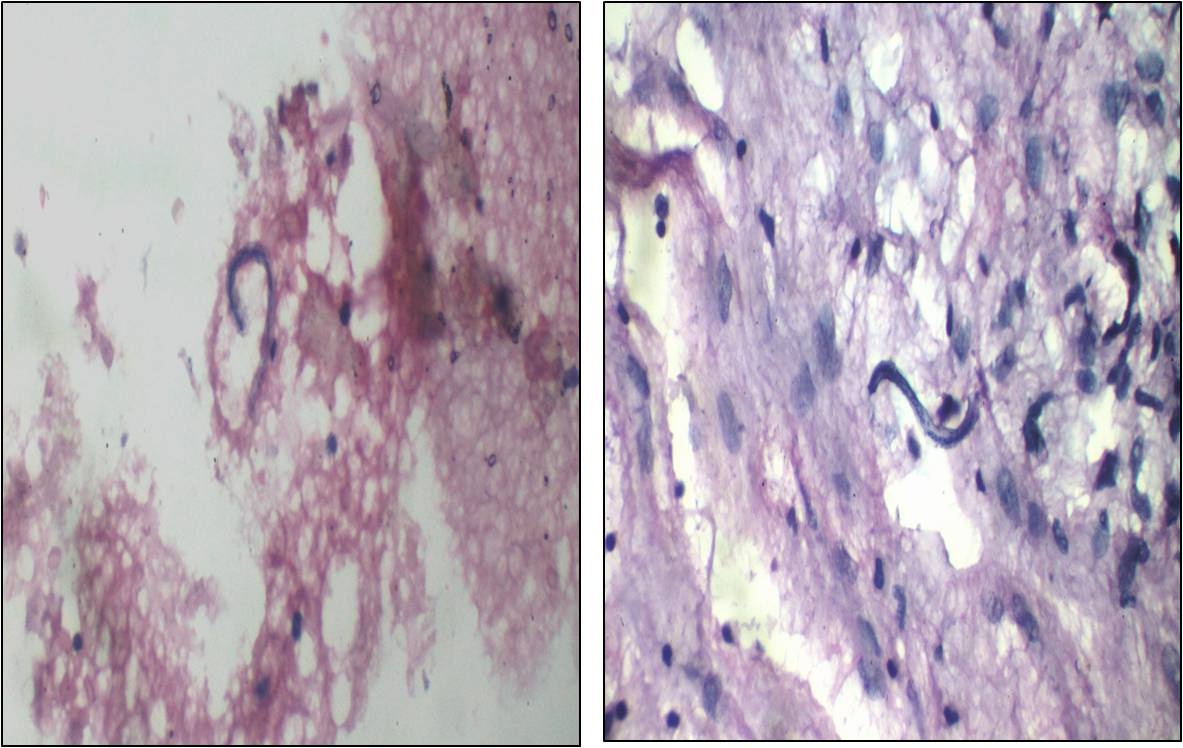
FNAC smears were cellular and showed monolayered sheets and clusters of benign ductal epithelial cells, bare nuclei, myoepithelial cells, few stromal fragments and scattered inflammatory cells comprising of eosinophils, neutrophils and lymphocytes [Table/Fig-1]. Also, noted were sheathed microfilariae, with tail tips free from nuclei [Table/Fig-2]. A diagnosis of fibroadenoma with filarial infestation by Wuchereria bancrofti was rendered on cytology smears. Complete blood count (CBC) revealed mild eosinophilia with absolute eosinophil count of 720/cmm. Peripheral smear did not show presence of microfilaria. Three daytime and two nocturnal samples were tested for microfilariae. Patient was treated with diethylcarbamazine for 21 days. Repeat CBC revealed the decrease in the absolute eosinophil count to 170/cmm. She subsequently underwent lumpectomy. Grossly the specimen measured 4x 3x2.5 cm. The cut surface was grey–white and myxoid with slit like spaces. Histopathology confirmed the diagnosis of fibroadenoma with cellular stroma with presence of microfilarial parasites in the interlobular stroma. Sparse lymphocytic infiltrate with occasional eosinophils was seen. However, granulomatous reaction was not seen [Table/Fig-3,4].
FNAC breast showing monolayered sheets and clusters of benign ductal epithelial cells with filarial parasite (H&E,40X)
FNAC breast showing sheathed microfilariae (Wuchereria bancrofti), with tail tip free from nuclei.(H&E,400X)
Histopathology section showing fibroadenoma with cellular stroma and presence of microfilarial parasite.(H&E,100X and 400X)
Histopathology section showing presence of microfilarial parasites.(H&E,400X)
Discussion
Filariasis is a significant global health problem and has been identified as a leading cause of permanent and long term disability, by WHO. The disease is endemic in India with heavily infected areas found in Uttar Pradesh, Bihar, Jharkhand, Andhra Pradesh, Orissa, Tamil Nadu, Kerala and Gujarat. In India, filariasis is caused by 2 closely related nematodes, Wuchereria bancrofti & Brugia malayi with Bancroftian filariasis being responsible for 98% of the infection in endemic countries [1].
Filariasis mainly involves the lymphatic system of lower limbs, spermatic cord, epididymis, retroperitoneal tissues and glands [2]. Extranodal filariasis is rare and has been reported in uncommon sites including skin and soft tissue swelling, breast, thyroid nodule, salivary gland, cervicovaginal smear, ovarian cyst, effusion fluids, urine, bronchial, laryngeal & pharyngeal brushings [3–6].
Mammary filariasis is rare. In the breast, most common site of involvement is upper outer quadrant [6]. In our case, patient presented with a lump in upper and outer quadrant of left breast.
In the filariasis of breast, lymphatic obstruction is caused by lymphangitis and fibrosis. Enlargement of axillary lymph nodes and hyperaemia of the overlying skin with peau d’ orange appearance has also been reported, thus mimicking malignancy [5,6]. In our case, no such findings were present. In breast FNAC, in a case of filariasis, smear reveal adult filarial worms or microfilariae, epithelioid cell granulomas and eosinophilic infiltrate [7]. The tissue response to parasite is variable, ranging from minimal response to marked inflammatory cell infiltration and formation of epithelioid cell granulomas [6]. In the present case, smears revealed cytomorphology of fibroadenoma with presence of microfilariae and scanty inflammatory infiltrate. Granulomatous reaction was not seen. Histopathology revealed similar features. In their case report of filarial granuloma in the breast, Patrikar et al., found adult filarial parasite with granulomatous reaction in a lumpectomy specimen. They emphasized that when unexplained granulomas are found in the breast, adult worms and microfilariae should be searched, especially in endemic areas [6,8].
In our case, CBC revealed mild eosinophilia. Microfilariae were not detected on smear examination. Many authors have reported that filariasis can exist without microfilaraemia [6]. In their report of 22 cases of microfilariae in fine needle aspirates from various sites, Yenkeshwar et al., found eosinophilia in 5 cases and microfilaraemia in only 3 cases [3]. Mitra et al., in their FNAC study of 250, found filariasis in 24 cases at various sites including 8 cases in the breast, Out of these, eosinophilia was present in 8 cases and microfilaraemia in 3 cases only [4]. Our findings are consistent with those of other authors.
In endemic areas, infection is acquired early in life with peak incidence between 15–20 years and infected individuals are often asymptomatic [3,4]. Our patient came from Sultanpur in Uttar Pradesh, an endemic area. She was 20-year-old and did not have any clinical evidence of filariasis except for fever.
Microfilariae very rarely co-exist with neoplastic lesions. They have been reported in association with malignancies; however association with benign neoplasms is extremely rare. Yenkeshwar et al., in their report of 22 cases, found microfilariae in breast in 3 cases, associated with infiltrating duct carcinoma in one case [3]. Pantola et al., in their series of 7 cases reported microfilariae co-existing with 6 malignant lesions including 1 case of adenocarcinoma of breast and only one benign lesion, pleomorphic adenoma of parotid gland [9]. Nalini et al., have reported a case of filariasis of breast masquerading a fibroadenoma clinically [5].
In our case microfilariae were seen against a background of fibroadenoma, which is an extremely rare association. The presence of microfilaria in aspirate from a neoplastic lesion is an incidental association. Some authors have suggested their presence in the neoplasms being due to increased vascularity associated with neoplastic lesions [9]. Filariasis does not alter the clinical presentation of the tumour and the patient possibly harbours subclinical filariasis already when the tumour develops [3,6]. This is likely to have occurred in our patient also as she hailed from an endemic area. Filariasis was not considered as a diagnostic possibility in our case.
Conclusion
To summarize, filariasis may be incidentally detected in FNAC smears in clinically unsuspected cases with absence of microfilariae in peripheral blood. The present case emphasizes the need to consider filariasis as one of the differential diagnoses of a breast lump in patients living in endemic areas. Careful screening of cytology smears can detect microfilaria even in asymptomatic patients so that specific treatment can be administered to avoid complications associated with lymphatic filariasis.
[1]. Park K, Epidemiology of communicable diseases. In: Park, editorText book of Preventive and Social Medicine 2005 18th edJabalpurBanarsidas Bhanot Publishers:211-16. [Google Scholar]
[2]. Shastry S, Detection of microfilaria on needle aspiration from breast mass: An uncommon findingTrop Parasitol 2014 4(1):58-59. [Google Scholar]
[3]. Yenkeshwar PN, Kumbhalkar DT, Bobhate SK, Microfilariae in fine needle aspirates: a report of 22 casesIndian J Pathol Microbiol 2006 49(3):365-69. [Google Scholar]
[4]. Mitra SK, Mishra RK, Verma P, Cytological diagnosis of microfilariae in filariasis endemic areas of eastern Uttar PradeshJ Cytol 2009 26(1):11-14. [Google Scholar]
[5]. Nalini G, Anu C, Adult filarial worm of breast masquerading fibroadenoma: A case reportInt J Res Health Sci 2014 2(1):366-68. [Google Scholar]
[6]. Gole S, Satyanarayana V, Gole G, Unusual cytological findings in breast aspirates: case studies of microfilariae with review of literatureThe Internet Journal of Pathology 2013 14(1):1-7. [Google Scholar]
[7]. Rosen PP, Specific infections. In: Rosen PP, editorRosen’s Breast pathology 2001 2nd edPhiladelphiaLippincott, Williams and Wikkins:65-75. [Google Scholar]
[8]. Patrikar A, Maimoon S, Mahore S, Filarial granuloma in breastIndian J Pathol Microbiol 2008 51:85-86. [Google Scholar]
[9]. Pantola C, Kala S, Agarwal A, Khan L, Microfilaria in cytological smears at rare sites co-existing with unusual pathology: A series of seven casesTrop Parasitol 2012 2:61-63. [Google Scholar]