The treatment options for invasive carcinoma cervix FIGO IA are simple hysterectomy or radiotherapy (RT) in the form of external beam radiotherapy (EBRT) and/or intracavitary brachytherapy (ICRT). Radical hysterectomy with bilateral pelvic lymphadenectomy or EBRT with concurrent chemotherapy (CT) followed by ICRT are the two standard options for patients with FIGO IB to IIA carcinoma cervix. Patients who choose to undergo radical surgery are categorized into three risk groups based on the histopathological factors based on Sedlis criteria [1]. Patients falling into low-risk group do not merit any adjuvant treatment whereas those with intermediate risk require adjuvant radiotherapy. Concurrent chemoradiation is advocated for high-risk category patients [2].
Approximately, 70% of Indian population lives in rural areas with limited health care facilities. As per UNESCO report 2014 India’s illiterate population is the largest in the world [3]. In general, most of the population living in rural India belongs to poor socioeconomic strata. Due to lack of awareness of disease coupled with financial strains and lack of sound surgical skill in primary health center, most of the patients of cancer cervix are referred to tertiary hospital after an inadvertent hysterectomy. Many a time, patients do not have any operative notes and histopathological details. Unfortunately, in several instances histopathological slides and blocks are not available for their review [4].
The risk of disease recurrence after optimum hysterectomy and pelvic lymph node dissection is as high as 60% if adjuvant treatment is not given [5]. Therefore, it seems logical that the probability of disease recurrence would be higher after an incomplete surgery. Subsequent to inadvertent surgery, these patients merit a revision surgery or adjuvant RT with or without chemotherapy.
The purpose of this study was to evaluate the survival outcome of induction chemotherapy followed by EBRT and ICRT in patients with cancer cervix subsequent to inadvertent surgery.
Materials and Methods
We chose to study only those patients who had a history of hysterectomy and tissue diagnosis of cervical carcinoma before being registered with us. The second important criteria for patient selection were clinical and radiological absence of residual or recurrent disease at the time of presentation to our OPD. Most of these patients were asymptomatic at presentation to us and were referred by the surgeons for adjuvant treatment. We chose to study the records of only those patients, who were registered with us between October 2011 and September 2014. Patient, tumour and treatment details were carefully studied. Every patient had thorough clinical examination and radiological assessment in the form of CECT whole abdomen and chest X-ray to rule out any residual or recurrent disease at the time of presentation. Complete haemogram, liver function test and renal function test was done to know the general well being of the patient. If necessary, blood transfusion was done to maintain the haemoglobin level at 10 gm%.
External beam radiotherapy
Patients were simulated in supine position with hands above the head and bladder full with either 2 field AP/PA or 4 field box technique. The upper border for both the AP & PA fields was placed at L5/S1 junction if pelvic lymph nodes were negative or at L4/L5 junction if the nodes were positive or unknown. The lower border was placed at the lower border of the obturator foramen. Lateral borders were placed 1.5 cm beyond the widest pelvic brim. The anterior and posterior fields of lateral fields were kept at the anterior part of symphysis pubis and S2/S3 junction.
Patients were treated on Telecobalt unit to a dose of 46 Gy- 50 Gy in 23-25 fractions over 4.5 to 5 weeks period. The dose was prescribed at the midplane if 2 fields were used and at isocentre if 4 field box techniques were used. Complete blood count along with clinical assessment was done once a week while the patients were on EBRT.
Brachytherapy
Patients were treated with low dose rate brachytherapy using vaginal cylinders to a dose of 15 Gy prescribed at 0.5 cm from the vaginal surface. Proximal 4-6 cm of vagina was treated. Patients were usually taken up ICRT after 10-15 days of completion of EBRT.
Chemotherapy
Prior to radiotherapy, patients were given three cycles of Inj. Paclitaxel (175 mg/m2) over 3 hours infusion and Inj. Carboplatin AUC 5 over 1 hour infusion every three week. Primary neutropenia prophylaxis using three doses of Inj. Filgrastim (300 mcg) from D5-D7 was given to all the patients receiving the above regimen.
Few patients received Inj. Carboplatin (AUC 5) before EBRT while some were treated with concurrent Inj. Cisplatin (40 mg/m2). Dose reduction of chemotherapeutic drugs was done in case of haematological toxicity.
Follow-up
Thorough clinical assessment of every patient was done once every month for consecutive three months and then two monthly for one year. Thereafter, patients were reviewed once in three months in the second year and six monthly in subsequent years. Radiological and PAP smear were done as and when required.
Ethics Committee approval: Since our study was a retrospective analysis of patients already treated in the department, the approval of ethical committee for conducting the analysis was not required.
Statistical Analysis
The primary end points were overall survival (OS) and disease free survival (DFS). OS was calculated from the date of registration to the date of event or date of last follow-up. Survival analysis was done based on the worst-case scenario where all the patients lost to follow-up were considered as an event. DFS was calculated from the date of diagnosis to the date of radiological evidence of relapse or date of last follow-up. OS and DFS were estimated using Kaplan-Meier method, and the differences in survival rates were compared using the log-rank test. Prognostic factors likely to influence the survival outcomes were estimated using univariate analyses. P-value of 0.05 or less was considered statistically significant.
Results
We could find 34 patients who met the eligibility criteria of our study. These patients had incomplete surgery, incomplete operative details and lacked proper histopathological findings of their surgical specimen. Status of resection margin was not known in any of the patient while three patients had parametrium positive disease. The patient and tumour characteristics are given in [Table/Fig-1] while treatment profiles are mentioned in [Table/Fig-2].
Patient characteristics in study population
| Characteristic | Value (n, %) |
|---|
| Age (years) |
| median | 48 |
| range | 30-72 |
| Tumor size |
| < 4 cm | 12 (35.3) |
| > 4 cm | 5 (14.7) |
| unknown | 17 (50) |
| Lymph node status |
| positive | 2 (5.9) |
| negative | 4 (11.8) |
| unknown | 28 (82.4) |
| Histologic findings |
| squamous cell carcinoma | 24 (70.6) |
| adenocarcinoma | 8 (23.5) |
| adenosquamous carcinoma | 2 (5.9) |
| Grade of tumor |
| WD | 14 (41.2) |
| MD | 7 (20.6) |
| PD | 3 (8.8) |
| unknown | 10 (29.4) |
| FIGO stage |
| IB1 | 6 (17.6) |
| IB2 | 3 (8.8) |
| IIA1 | 3 (8.8) |
| IIB | 3 (8.8) |
| unknown | 19 (55.9) |
| Characteristic | Value (n, %) |
|---|
| Surgery |
| simple hysterectomy | 2 (5.9) |
| total hysterectomy | 32 (94.1) |
| Chemotherapy |
| before EBRT | 25 (73.5) |
| concurrent with EBRT | 2 (5.9) |
| not given | 7 (20.6) |
| Chemotherapy regime |
| Paclitaxel + Carboplatin | 21 (77.8) |
| Carboplatin | 3 (11.1) |
| Cisplatin | 3 (11.1) |
| EBRT |
| < 46 Gy | 2 (5.8) |
| 46-50 Gy | 32 (94.2) |
| ICRT |
| done | 30 (88.2) |
| not done | 4 (11.8) |
The median time duration between surgery and registration in our department was 30 days (range, 9-261 days). Seven patients did not receive any CT. Taxane based CT was given to 21 (65%) patients. The median number of CT cycles was three. The gap between surgery and RT was 41-351 days (median, 97.5 days). Median EBRT dose was 46 Gy in 23 fractions. The median EBRT duration was 32 days. Two patients defaulted after few fractions of EBRT due to complications arising from RT. Of the 32 patients who completed the planned EBRT dose, two did not turn up for ICRT. The reason could not be traced out due to failure to contact those patients. Two patients were treated with high dose rate brachytherapy to a dose of 6 Gy per fraction for two fractions, one week apart. The remaining patients received 15 Gy with low dose rate brachytherapy over 20-24 hours. The median total radiotherapy duration was 50 days.
Analysis was done on 01.06.2015. Median follow-up (FU) period of patients who were alive was 16 months. At the time of analysis one patient had died due to disease. Twenty one patients were alive without disease while three were alive with disease. Eight patients had lost to FU without any evidence of disease while one patient was lost to FU with disease. The 3- year OS and DFS was 70% and 68%. Local recurrence was seen in four patients while local with distant failure was found in one patient. The time duration for relapse was three to six months after completion of treatment.
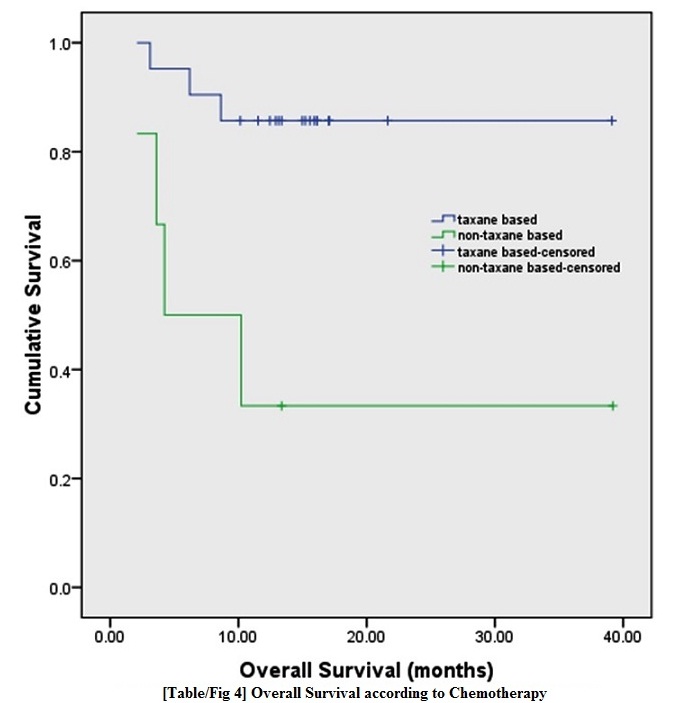
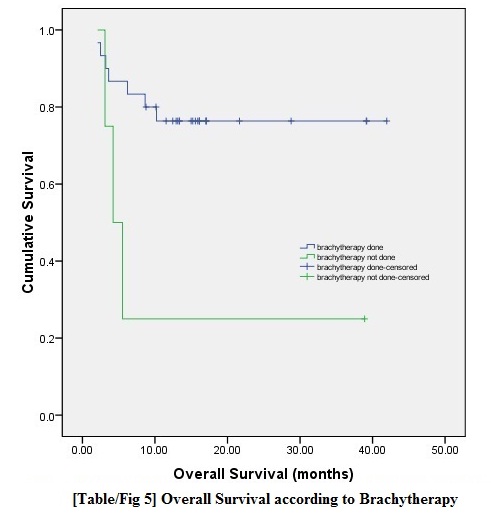
We looked into factors, which were likely to affect OS and DFS [Table/Fig-3]. We carried out univariate analysis using Kaplan-Meier method. It was observed that those who were treated with Taxane-based chemotherapy and those who completed the planned dose of RT (EBRT & ICRT) had significantly better overall survival as illustrated by Kaplan-Meier plots [Table/Fig-4,5]. The survival was more than double for patients in whom the adjuvant therapy was started within 56 days of surgery but had completed their planned RT course compared to similar group of patients in whom the same was delayed for more than eight weeks. The difference was not significant due to fewer numbers of patients in our study.
Univariate analysis of prognostic factors with survival outcome
| Factor | Mean OS (months) | p | Mean DFS (months) | p |
|---|
| Age (years) |
| < 49 (18) | 29.7 | 0.780 | 29.7 | 0.791 |
| > 49 (16) | 30.2 | 30.0 |
| Histology |
| Squamous (24) | 29.5 | 0.419 | 29.4 | 0.424 |
| Non-squamous (10) | 32.3 | 32.4 |
| CT regime |
| Taxane based (21) | 34.4 | 0.005 | 34.3 | 0.003 |
| Non-taxane based (6) | 16.4 | 15.9 |
| ICRT |
| Done (30) | 33.3 | 0.015 | 33.2 | 0.015 |
| Not done (4) | 12.9 | 12.9 |
| Gap between surgery and adjuvant treatment (days) in patients who had ICRT |
| < 56 (22) | 35.1 | 0.299 | 35.1 | 0.272 |
| >56 (8) | 15.9 | 15.5 |
Abbreviations: OS = overall survival; DFS = disease free survival; ICRT = intracavitary brachytherapy; CT = chemotherapy. Data in parentheses are numbers of patients
Overall survival based on type of chemotherapy
Overall survival based on brachytherapy
Compliance to CT was good in our patients as every patient received the planned number of CT cycles. Two patients defaulted after few fractions of EBRT; the exact cause could not be found out as we could not contact these patients. The EBRT median durations for patients receiving 50 Gy and 46 Gy were 36 days (range, 32-42 days) and 32 days (range, 30-43 days). The median gap between completion of external radiation and brachytherapy was 18 days.
Discussion
Though most of our patients had total hysterectomy, pelvic lymph node dissection was found only in five. We could not assess the histological grade in about 30% of patients. The size of the tumour was not known in 50% of patients. Due to lack of preoperative and operative details, stage of the disease could not be determined in about 56% of patients. The depths of stromal infiltration, status of lympho-vascular invasion and surgical resection margins were not mentioned in any of the histopathological reports of these patients. However, none of our patients had any clinical and radiological residual or recurrent disease at the time of presentation to our OPD.
We chose to treat most of these patients with chemoradiation because of several reasons; the most important one was that they had inadequate surgery i.e. total or simple hysterectomy without any lymph node dissection in majority of the cases. Preoperative stage was unknown in 19 patients and three had FIGO IIB disease. The last but very pertinent reason was the gap between surgery and treatment in 12 patients was more than six weeks, which could have adversely affected the prognosis of these patients.
Sedlis et al., based on a prospective randomized controlled trial in postoperative cervical patients with intermediate risk, had reported that adjuvant RT reduced local recurrence from 28% to 15% at 2 years after treatment [1]. Peters et al., prospectively compared RT with CCRT in postoperative cervical cancer patients with high risk features (node positive, positive resection margin or microscopic parametrium involvement) [2]. Patients received four cycles of three weekly cisplatin and 5-FU of which two cycles were given concurrently and another two cycles were given after completion of EBRT. ICRT was not used in the trial. The CCRT arm had significantly better OS and DFS. Distant metastasis in RT and CCRT was 15.5% and 11% respectively. The authors concluded that the beneficial effect of addition of CT could have been because of its radiosensitizing property or elimination of distant micrometastasis or both.
MP Schmid et al., did a retrospective study in 189 patients of cancer cervix FIGO IB-IVA, treated with RT alone or RT with concomitant cisplatin, to investigate the patterns of distant relapse [6]. Patients with any stage with positive lymph nodes were categorized into high-risk groups. It was noted that those patients at high risk had a 40% probability of distant metastasis within five years of treatment. They also observed that the risk of distant metastases increased with decreasing number of CT cycles. Despite adequate number of CT cycles, 23% of high-risk patients failed at distant sites.
We chose to retrospectively study patients at high risk of failure who had received induction CT followed by RT so as to see if the above treatment had favorable outcome in terms of OS, DFS and reduced distant failure.
Perez et al., had reported that most of the recurrences occur within three years of completion of radiotherapy [7]. The authors also made an observation that about 80% of failures were seen within 24 months of treatment. Since our maximum FU period was 42 months, we have reported 3-year OS and DFS. In our study, 3-year OS and DFS were 70% and 68% respectively. Our survival outcome is comparable with those reported in the recent trials dealing with inadvertent hysterectomy followed by postoperative radiotherapy where the 5-year OS ranges from 63.5% to 93% [8–12]. Four of five recurrences were observed in patients where the FIGO stage was not known, which probably indicate that those patients may be having a higher stage. Only one patient (2.9%) had extra-pelvic failure along with central disease recurrence which is very less as shown in the recent trial [2].
Based on univariate analysis our data, we do not suggest any significant difference between squamous and non-squamous histologies with regard to change in prognosis. Kasamatsu et al., [13] had reported no difference in prognosis when 123 patients with adenocarcinoma were compared with 455 patients with squamous cell histology. All these patients had radical hysterectomy followed by adjuvant treatment. After controlling for tumour size, lymph node involvement, depth of cervical stromal invasion, parametrial and vaginal invasion, the histological type had no significant difference in survival outcome.
The impact of time interval between hysterectomy and initiation of adjuvant treatment was reported by Saibishkumar et al., wherein patients in whom RT was started within 80 days of hysterectomy had fared better than their counterparts [14]. We found that when the gap between surgery and start of adjuvant treatment was over 56 days, the OS and DFS dropped to more than half compared to their counterparts. However, the difference was not significant in terms of statistics due to less number of patients in our study.
Paclitaxel and cisplatin combination was compared with cisplatin alone in stage IVB, recurrent or persistent squamous cell carcinoma of cervix in a phase III trial by David H Moore et al., [15]. The authors reported significant improvement in progression free survival, and response rates with these two drug regimes. CCRT with Paclitaxel and Carboplatin has been shown to be effective in achieving an excellent pelvic control when used as a definitive treatment for squamous cell carcinoma of the uterine cervix [16]. Paclitaxel-Carboplatin combination had significant positive impact on OS and DFS when compared to non-taxane chemotherapy drugs used in our study.
Patients who completed EBRT, and brachytherapy had definite better survival results than those who failed to complete EBRT and/or did not turn up for ICRT. Our study strongly advocates the need for completion of EBRT followed by vaginal cuff boost with brachytherapy in patients with inadequate hysterectomy. Our result is supported by the study conducted by Saibishkumar et al., [14].
Limitations
Our study had few caveats; the most important being that it was a retrospective analysis. The power of the study was not very strong, and we could not report the acute and late toxicities of our patients.
Conclusion
Inadequate hysterectomy with incomplete histopathological information is not uncommon for those patients who have improper primary health facility. It is important that these patients should be taken up for adjuvant treatment as early as possible so as to avoid inferior survival outcomes. These patients should be treated as high-risk group for failure and should receive chemotherapy and radical dose of EBRT and ICRT. Prospective randomized trial should be done so as to establish the role of induction chemotherapy with Paclitaxel and Carboplatin followed by EBRT and ICRT in such patients.
Abbreviations: OS = overall survival; DFS = disease free survival; ICRT = intracavitary brachytherapy; CT = chemotherapy. Data in parentheses are numbers of patients