Subcutaneous fungal infection is common in tropical and subtropical countries particularly in India. They occur following traumatic penetration of the causative fungi from the contaminated soil. The lesions are usually localised and present as non-tender nodular swelling. Hence clinically they are commonly mistaken for other benign lesions. Diagnosis is often by histopathology and culture sensitivity [1]. In this study, we have retrospectively analysed eight cases with subcutaneous cystic lesions which turned out to be fungal infections along with a brief review of subcutaneous fungal infections.
Materials and Methods
A retrospective study was done on subcutaneous fungal infections seen between January 2007 to July 2014 in the Department of Pathology, Pondicherry Institute of Medical Sciences, Puducherry, India. For the purpose of this study, all patients with biopsy proven subcutaneous fungal infection during the study period were included. We excluded duplication of data of the same patient who had repeated biopsies. The details of all these patients were obtained from computerised hospital information system.
Total of eight patients were diagnosed with subcutaneous fungal nodules. Patients’ demographic and clinical data was collected and analysed. For this study, we collected the following information - age, gender, site, clinical symptoms and predisposing factors mainly history of trauma (thorn prick). Details of fine needle aspiration cytology, fungal morphology, histopathology findings, special stainings used and culture sensitivity were also recorded. Fungal infection was identified based on Haematoxylin and Eosin stain (H&E) along with special stains like Periodic Acid Schiff (PAS), Gomori Methanamine silver (GMS) and Fontana-Masson (MF) staining. Diagnosis was based on the presence of characteristic tissue host response in histopathology.
Results
Among eight patients, six were male and two were female. The mean age was 47 years (Range: 21-70). All the eight patients presented with non-tender swelling. The size of the swellings varied from a minimum of 3 x 3 cm to maximum of 10 x 4 cm. None of them had discharging sinus. Four had history of thorn prick and one had preceding history of trauma. Out of eight, three had involvement of hand, one patient had involvement of the forearm, two had elbow involvement and one each of leg and foot. Among eight patients, two of them had diabetes mellitus. Clinically, all these lesions were suspected to be benign soft tissue lesions such as sebaceous cyst, dermoid cyst, lipoma, ganglion and bursitis.
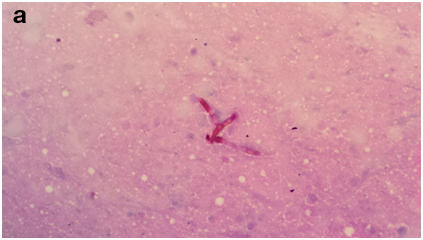
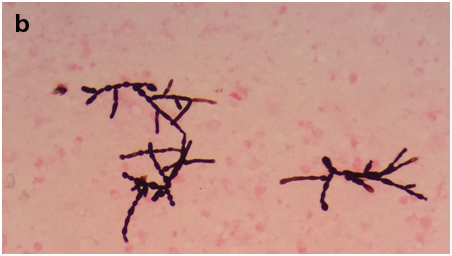
Out of eight patients, only two of them underwent prior fine needle aspiration cytology (FNAC) before definitive surgery. Fungal infection was identified on FNAC by the presence of fungal hyphae in the background of necrosis [Table/Fig-1a,b]. Only these two patients had culture sensitivity out of which one showed no growth and the other grew Exophiala oligosperma.
FNA showing pigmented fungal hyphae with acute angle branching and constrictions at septa on PAS stain (400X)
Mason-Fontana stains highlighting the pigmented hyphae (400X)
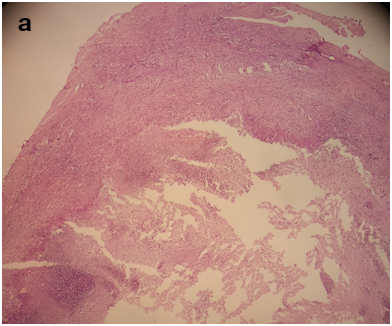
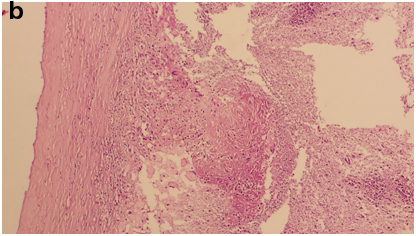
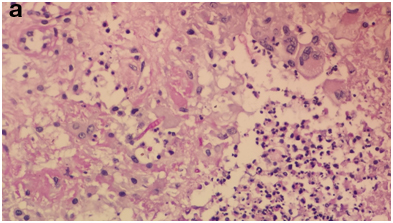
The histopathology and the fungal morphology findings are mentioned in [Table/Fig-2]. On H&E staining, all the eight cases showed fibrocollagenous cyst wall, lined by histiocytes, granulomatous reaction, foreign body type of giant cells with acute and chronic inflammatory infiltrate with fungal elements lying in the stroma or within the giant cells [Table/Fig-3a,b].
Table showing the patient demographics and histopathology features
| S. no | Age /Sex | Site | Clinical diagnosis | HPE | Fungal morphology | Diagnosis |
|---|
| 1 | 47/M | Left hand | Ganglion | Cyst wall is lined by chronic inflammatory cells and granulation tissue with foreign body giant cell reaction | Non pigmented, acute angle branching septate hyphae | Hyalohyphomycosis |
| 2 | 38/M | Right elbow | Lipoma | Cyst wall with foreign body giant cell & histiocytes | Pigmented, thin fibrous septate, acute angle branching with bulbous constrictions at septate. Thick walled spores present. | Phaeohyphomycotic cyst |
| 3 | 70/M | Left leg | Lipoma | Cyst wall with convoluted surface lined by histiocytes, epitheliod cells, foreign body giant cells | Non pigmented, septate hyphae with focal acute angle branching and bulbous constrictions at septate | Hyalohyphomycosis |
| 4 | 67/M | Right forearm | Dermoid cyst | Cyst wall is lined by foamy macrophages, foreign body type of giant cells | Pigmented, thin fibrous septate, acute angle branching with bulbous constrictions at septate. Thick walled spores present | Phaeohyphomycotic cyst |
| 5 | 40/F | Right hand | Sebaceous cyst | Convoluted polypoidal surface of cyst showing eosinophils, necrotic tissue, acute and chronic inflammatory cells, histiocytes & few multinucleate giant cells | Non pigmented, septate hyphae with acute angle branching, bulbous constrictions at septate. Thick walled round spores are noted | Hyalohyphomycosis |
| 6 | 36/M | Left elbow | Bursitis | Convoluted cyst wall lined by palisaded histiocytes, foci of necrosis, foreign body giant cells along with lymphocytes, plasma cells, polymorphs seen | Non pigmented, septate hyphae with focal acute angle branching and bulbous constrictions at septate | Hyalohyphomycosis |
| 7 | 21/M | Left foot | Ganglion | Cyst wall present with necrosis, granulation tissue, macrophages, foreign body type of giant cells, acute and chronic inflammatory cells | Non pigmented, acute angle branching septate hyphae | Hyalohyphomycosis |
| 8 | 57/F | Right finger | Dermoid cyst | Cyst wall present with necrosis, granulation tissue, macrophages, foreign body type of giant cells, acute and chronic inflammatory cells | Non pigmented, thin varicose septate with constrictions at septa. Thick walled spores present | Hyalohyphomycosis |
H&E stain showing the fibrocollagenous cyst wall with dense inflammatory response (100X)
H&E stain showing foreign body giant cell reaction (400X)
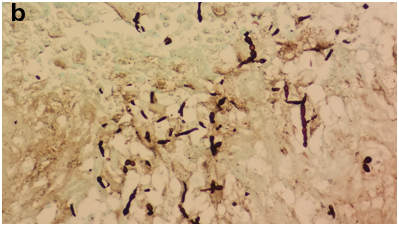
Out of eight cases, six were identified as hyalohyphomycosis and two were identified as Phaeohyphomycotic cysts based on pigmentation of hyphae. Among the special stains, all were positive for Periodic acid Schiff and Gomori Methanamine Silver staining [Table/Fig-4a,b]. Two were positive for Fontana-Mason stain, indicating presence of melanin pigment.
PAS stain showing fungal hyphae surrounded by dense inflammatory response (400X)
GMS stain showing fungal hyphae surrounded by dense inflammatory response (400X)
Discussion
Subcutaneous fungal infection or mycoses include fungal infections involving the dermis and the subcutaneous tissue. They usually occur following invasion of the fungi into the subcutaneous layer following accidental traumatic penetration of thorns or wooden stick. The common subcutaneous mycoses are zygomycosis, phaeohyphomycosis, hyalohyphomycosis, mycetoma, chromoblastomycosis, sporotrichosis, lobomycosis and rhinosporidiosis [1].
The various manifestations of subcutaneous fungal infections in literature are cyst, plaque, ulcer, scaly lesion, verrucous growth, warty plaque, abscess and keratotic macerated lesions [Table/Fig-5].
Comparative table from various studies about clinical presentation of subcutaneous fungal infection
| S.No | Author | No. of cases | Clinical presentation (No. of cases) |
|---|
| 1 | O’Donnell et al., [1] | 9 | Cyst (8) Recurrent ulcer (1) |
| 2 | Abraham et al., [2] | 7 | Subcutaneous nodules (7) |
| 3 | Sheikh et al., [3] | 21 | Cyst (21) |
| 4 | Sharma et al., [4] | 23(review) | Cyst (3)Abscess (2)Ulcer (7)Scaly lesion (3)Verrucous growth (1)Sinus (1)Warty plaques (1)Keratotic, macerated (2)Palpuloplaques (1)Nodule (2) |
| 5 | Present study | 8 | Cystic lesion (8) |
In the present study, six were diagnosed clinically as cystic lesions (sebaceous cyst, dermoid cyst, ganglion, bursitis) and two were diagnosed as lipoma. Our study showed two patients with pigmented pheohyphomycosis and six patients with non pigmented hyalohyphomycosis.
Hyalohyphomycosis is characterised by the presence of hyaline hyphae without the presence of pigment in the wall. It is a broad group which includes the following species namely Fusarium, Penicillium, Scedosporium, Acremonium, Paecilomyces, Aspergillus etc [5]. Clinical presentation varies from localised infection to disseminated infection based on the host’s immune status. Microscopically, hyalohyphomycosis is characterised by the presence of non pigmented hyaline hyphae with acute branching pattern [6]. Presence of adventitious sporulation in tissue section is characteristic of hyalohyphomycosis [6].
Sheikh et al., in their study described 21 cases of mycotic cysts [3]. Thirteen out of 21 were non-pigmented and eight were pigmented. The clinical suspicion in their series was lipoma, ganglion, sebaceous cyst and giant cell tumour of tendon sheath.
Pheohyphomycosis is caused by a wide group of pigmented dematiaceous fungi. These dematiaceous fungi are pigmented due to the presence of melanin in their cell wall. Subcutaneous phaeohyphomycosis is the most common type. Subcutaneous Pheohyphomycosis presents as localised cyst or abscess. These cysts are usually asymptomatic averaging about 2.5 cm in size. They are common in the extremities like foot, finger, leg, hand but are also seen in buttocks, face and scalp [7]. Sharma et al., in their study reviewed 23 patients with subcutaneous pheohyphomycosis in India [4]. In their study, out of 23 only one patient presented with cystic swelling and one presented with a nodule. Two other patients presented with a cyst associated with warty plaques. Other clinical presentations were ulcer, abscess, scaly lesion, papuloplaques, verrucous growth, keratotic lesion and sinus. Lower extremity was involved in eight of the cases followed by upper limb involvement in five. One of our patient showed Exophiala oligosperma which was published by Venkateshwar et al from our institute [8].
In a study by O’Donnell et al,. five out of nine patients presented with cystic lesion [1]. Recently Abraham et al., have described seven cases of subcutaneous pheohyphomycosis from India [2]. The details of these studies along with our study are mentioned in [Table/Fig-2,3a,b,4a,b and 5].
Histopathology of pheohyphomycosis shows inflammatory cells with multinucleated giant cells and epitheliod cells along with the presence of brown pigmented septate hyphae with acute angle branching [4]. Fontana- Masson staining demonstrates the presence of melanin. Gomori-Methanamine silver and Periodic acid Schiff stains also help in identifying the fungal wall. Jaiswal et al., in their study have described the role of Fine Needle Aspiration Cytology (FNAC) in subcutaneous fungal infection [9]. It is simple, safe, fast and cost effective method and helps in differentiating a fungal infection from neoplastic swellings.
In our study, all eight patients presented with non-tender nodule without any systemic features. The clinical diagnosis in most of the cases was sebaceous cyst or implantation dermoid. Hence most of these excised specimens were sent only for biopsy and culture was not done. This is probably because of the benign presentation of these lesions. Clinicians should always send tissues for culture and histopathology for all lesions even though clinically they do not suspect fungal infection. Tissue should always be sent for routine culture, acid fast bacilli and fungal culture. Though the incidence of fungal infection is rare, it would prove vital in the management of patients who are positive for the same and would avoid recurrence and repeat procedures. Treatment for all these lesions is surgical excision.
Limitations
The limitations of our study are its retrospective nature with small sample size and lack of fungal cultures.
Conclusion
Fungal infection presenting as subcutaneous cystic nodules is a diagnostic challenge. Prior FNAC should be done for these cases as it helps to suspect fungal infection and also helps in sending fungal culture during definitive surgery. A high index of suspicion is necessary for these lesions as early identification and appropriate treatment prevents recurrence and further complications.