Osteoporosis is a progressive disorder of the bones which is characterized by reduction in bone mass and increased risk of fractures. Until it is complicated by fractures, which can occur after trivial trauma, the condition remains asymptomatic. These fractures represent upto 80% of all fractures in menopausal women over 50 years of age [1]. Osteoporosis results in a huge medical burden on elderly individuals and results in a major economic toll on the healthcare system [2].
Fractures due to osteoporosis can be prevented after early diagnosis. Further, even after the first fracture has occurred, risk of further fractures can be decreased by appropriate treatment [3].
We designed this survey to analyse the epidemiology, approach to diagnosis and management of osteoporosis from the perspective of Indian healthcare practitioners. The following were the objectives of this survey to understand:
Materials and Methods
This was a questionnaire-based survey which was conducted between June to November 2013, over a duration of 6 months. A structured questionnaire was designed, which contained pre-validated questions covering various aspects of osteoporosis epidemiology and management. The questionnaire was categorized into 3 major sections:
Epidemiology and patient impact of osteoporosis.
Approach to the diagnosis and management of osteoporosis.
Clinical manifestations, investigations and management of osteoporosis,
Role of Bisphosphonates in osteoporosis,
Patient compliance pattern in osteoporosis,
Specific pharmacotherapy of osteoporosis.
Usage, efficacy and tolerability of Zoledronic acid and Calcitonin nasal spray in osteoporosis,
The questionnaire contained a mixture of objective and open-ended questions, with the former type being the majority. The questionnaire was circulated amongst orthopaedic surgeons across India (total of 39 centres in India: 13, 3, 2, 1 and 10 respectively in North, South, Central, East, and West parts of India) by means of post/courier, after giving a brief overview of the study telephonically, and only those orthopaedicians agreeing to participate in the survey were included in the study. The questionnaire was accompanied with a self-addressed envelope which enabled the respondents to post back the completed questionnaires.
Statistical Analysis
After receiving the completed questionnaires, the data was entered electronically and analysed after giving proper weightage to each section and each question. Data was expressed as numbers and percentages, as per the question and situation. Microsoft excel version 2013 was utilized for analysis and graphical representation of data.
Results
A total of 95 orthopaedic surgeons were contacted and the filled questionnaire was returned by a total of 84 orthopaedic surgeons throughout India. While most of the questions were filled in properly by all the 84 respondents, there were inconsistencies with respect to some questions and such inconsistencies were not included during analysis.
1. Epidemiology and Patient Impact of osteoporosis
The prevalence of osteoporosis in India according to the orthopaedic surgeons was 38.4%, and there was a female preponderance (61%). Most patients of osteoporosis were in the age group 51-60 years (31.67%), followed by those aged above 70 years (28.85%). Most respondents (68.67%) encounter over 20 cases of osteoporosis every month, and most of them (35.71%) see around 5-10 new cases of osteoporosis every month. On an average, 48.78% of the new osteoporosis cases are referred to the respondents by other practitioners, most notably by general physicians (40.3%).
The impact of osteoporosis on the patients, from the orthopaedicians perspective, included an increased chance of low impact trauma fractures (33.33%), psychological symptoms such as depression and loss of self-esteem (13.54%), straining of interpersonal relationships in the lives of the patients (1.04%) and all the three (52.08%).
2. Approach to the diagnosis and Management of osteoporosis
Most of the respondents felt out of every 100 osteoporosis patients in India, less than 20 patients are actually diagnosed and treated for osteoporosis (45.24% and 57.14% respondents respectively).
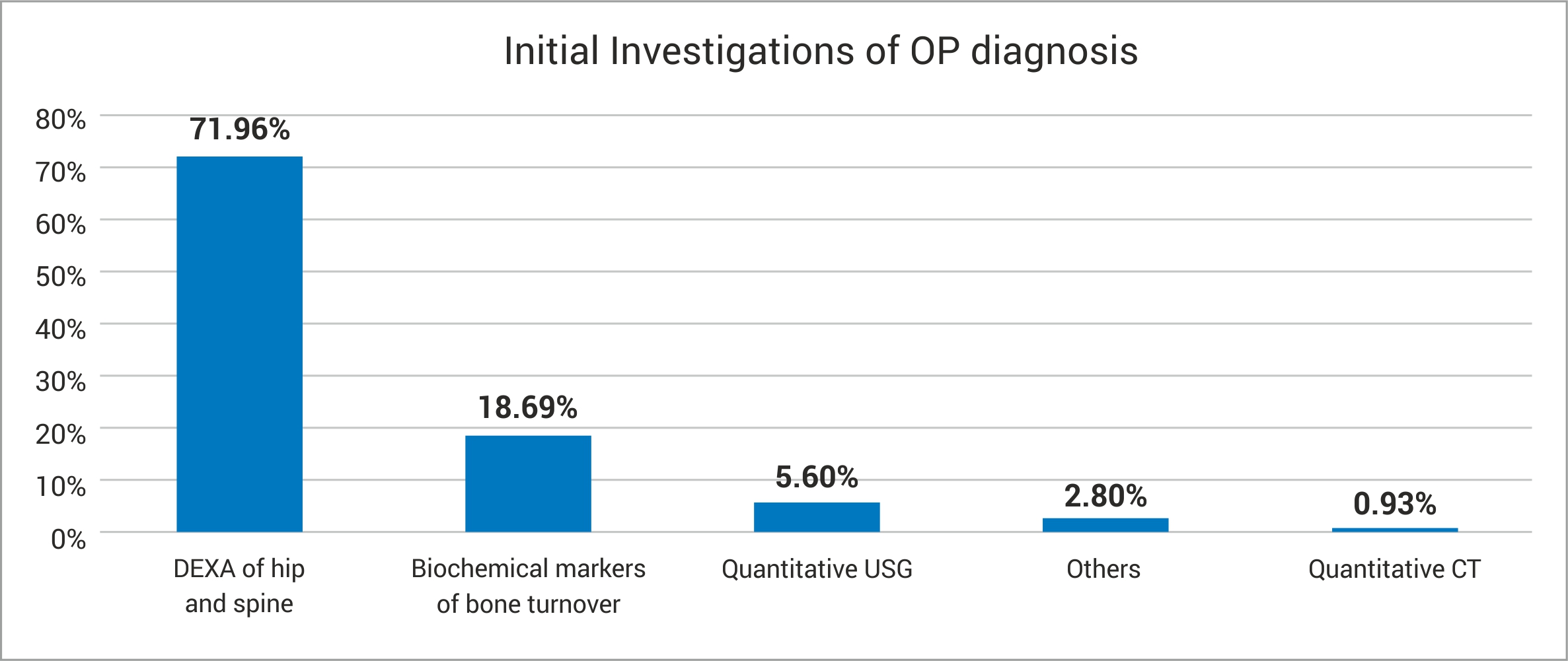
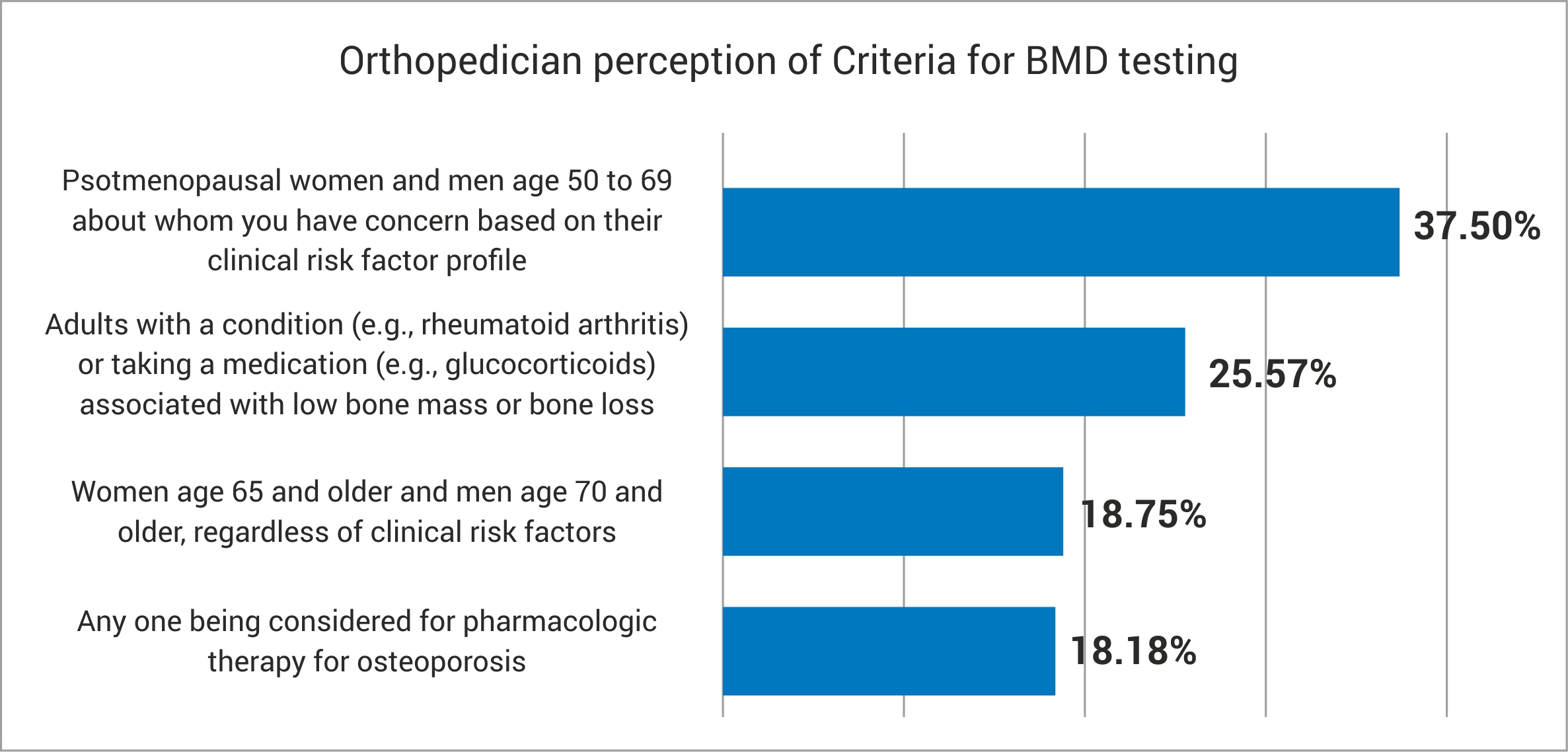
Clinical manifestations, Investigations and Management of osteoporosis: The three most common initial presenting features of established osteoporosis cases were general symptoms (45.16%), fracture (29.06%), and comorbid osteoarthritis (23.87%). The three most commonly considered risk factors before the diagnosis of osteoporosis were age and gender (36.59%), previous history of fracture (30.73%), and prior or current glucocorticoids usage (28.78%). Before considering a diagnosis of osteoporosis, 86.9% of the respondents consider alternate diagnoses such as hyperparathyroidism or osteomalacia, which is also, associated with a low BMD (bone mineral density) values. The initial investigation preference and criteria for initial BMD estimation are summarized in [Table/Fig-1a,b].
(a) ‘Initial investigations for OP diagnosis’ (b) ‘Orthopedician perception of Criteria for BMD testing’
Very few respondents (24.39%) routinely ordered for biochemical markers of bone metabolism for osteoporosis diagnosis. The reasons for this reluctance included high cost, poor availability of the biochemical tests and patient reluctance; some respondents felt that routine biochemical investigations are not important.
After treatment initiation, for monitoring treatment outcomes, the respondents utilized clinical examination (42.86%) and investigations like BMD estimation (34.52%) and DEXA (22.62%).
Most respondents chose first-line therapy for newly diagnosed osteoporosis as lifestyle modifications (34.5%), calcium-vitamin D supplementation (34%), and anti-osteoporosis therapy (31%).
The respondents were asked to enumerate the patient profile in which they preferred different treatment strategies; the responses are summarized in [Table/Fig-2].
Preferred patient profile for different treatment strategies of OP
| Treatment strategy andpreferred patient profile | No ofrespondents(%) | Treatment strategy andpreferred patient profile | No ofrespondents(%) |
|---|
| Calcium and Vitamin D | | Bisphosphonates | |
| All Patients | 20 (23.81%) | Post-Menopausal | 11(13.1%) |
| Age <50 years | 13 (15.48%) | All Patients | 11(13.1%) |
| Osteopenic patients | 11 (13.1%) | Severe OP | 10 (11.9%) |
| Mild to moderate OP | 6 (7.14%) | Elderly patients | 8 (9.52%) |
| Specific health condition (Myalgia, obesity, alcohol consumption, renal compromise) | 5 (5.95%) | BMD values | 7 (8.33%) |
| Others | 3 (3.57%) | Osteopenia | 4(4.76%) |
| Low calcium in diet or blood | 2 (2.38%) | Others | 3 (3.57%) |
| Absence of risk factors | 1 (1.19%) | <60 years | 2 (2.38%) |
| Teriparatide | | Mild to Mod OP | 1 (1.19%) |
| Severe OP | 20 (23.81%) | Calcitonin | |
| Fractures | 12 (14.29%) | Back pain/ Vertebral Fractures | 32 (38.1%) |
| Others | 6 (7.14%) | Post-Menopausal | 8 (9.52%) |
| Non-responding | 2 (2.38%) | Elderly | 6 (7.14%) |
| | Moderate to Severe OP | 4 (4.76%) |
| Denosumab | | Others | 4 (4.76%) |
| Bone pain, fractures | 4 (4.76%) | All patients | 3 (3.57%) |
| Moderate to severe OP | 2 (2.38%) | | |
Bisphosphonates in osteoporosis: Majority of respondents preferred to administer bisphosphonates orally in almost all patients with osteoporosis, and intravenously in moderate to severe cases of osteoporosis [Table/Fig-3].
Preferred patient profile for different treatment strategies of OP
| Patient characteristicsfor initiating OralBisphosphonates | No ofrespondents(%) | Patient characteristicsfor initiating Intravenousbisphosphonates | No ofrespondents(%) |
|---|
| Most/ All | 25 (29.76%) | Moderate to Severe OP | 12 (14.29%) |
| Post-menopausal | 15 (17.86%) | None | 10 (11.90%) |
| Elderly | 5 (5.95%) | Elderly | 8 (9.52%) |
| Mod to Severe OP | 4 (4.76%) | Post-operative, Hospitalized, or Bed-ridden | 6 (7.14%) |
| <50 years | 2 (2.38%) | Low compliance | 4 (4.76%) |
| Fractures | 2 (2.38%) | Unable to take oral medications | 2 (2.38%) |
| Others (mobile patients, educated patients, patients with renal compromise) | 4 (4.76%) | Post-Menopausal | 2 (2.38%) |
| | Others (poor oral hygiene, absence of cardiac diseases) | 2 (2.38%) |
Most respondents reported that the average duration of therapy of bisphosphonates was the maximum (27.04 months) among the other anti-osteoporosis therapies that they used. In comparison, the average durations of calcium, calcitriol, teriparatide and calcitonin were 10.2 months, 6.27 months, 11.52 months, and 4 months respectively.
Among various dosage schedules, one-a-month scheduling of oral bisphosphonates was preferred by most respondents (66.67%).
The gastrointestinal side effects of bisphosphonates when given orally as reported by the respondents included esophagitis (52.80%), gastric ulcer and gastritis (27.20%), difficulty in swallowing (18.40%), and nausea (1.6%).
Most respondents agreed that IV administration of bisphosphonates offered several advantages including less gastrointestinal side effects (47.52%), administration of medication under supervision (45.39%), and better compliance (7.09%). Among the various IV bisphosphonates, 81.18% of respondents had used Zoledronate.
Patient compliance pattern in osteoporosis: On an average, the patient compliance rate in osteoporosis management was around 64%. The most common reasons given for non-compliance in osteoporosis patients included lack of awareness (36.77%), and lack of visible advantages of the medicine to the patient (31.61%).
The most common steps employed by the respondents to improve compliance in osteoporosis patients included encouragement of lifestyle measures (35.23%), and stressing upon the importance of compliance to osteoporosis therapy (32.39%).
Most respondents (85.71%) felt that once-yearly IV bisphosphonate therapy would help improve compliance, and the reasons given included better convenience, better safety and better efficiency with IV route.
3. Specific pharmacotherapy of osteoporosis
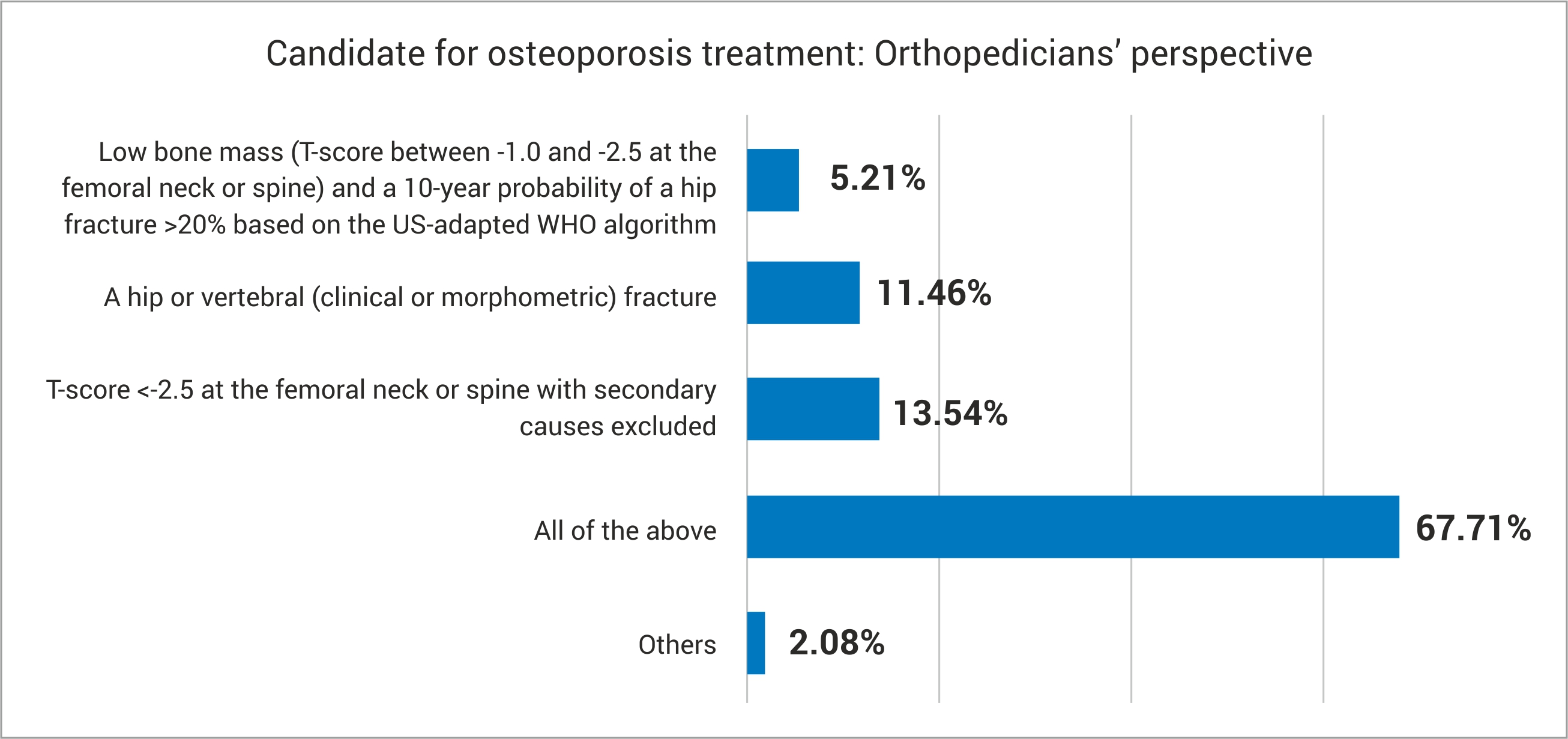
The orthopaedicians’ perspective of the suitable candidate for initiating osteoporosis treatment is summarized in [Table/Fig-4].
Orthopedicians’ perspective regarding candidate for OP treatment
Intravenous Zoledronic Acid (ZA) in osteoporosis: This therapy was preferred only in established osteoporosis cases by most of respondents (82.14%), and the reasons given for using in only this patient group and not elsewhere included compliance, convenience, safety concerns if used in other cases, high cost, and literature evidence. Some respondents also opined that they would initiate ZA earlier, if indicated. However, a small number of respondents (2/84) felt that available evidence concerning ZA did not show adequate efficacy.
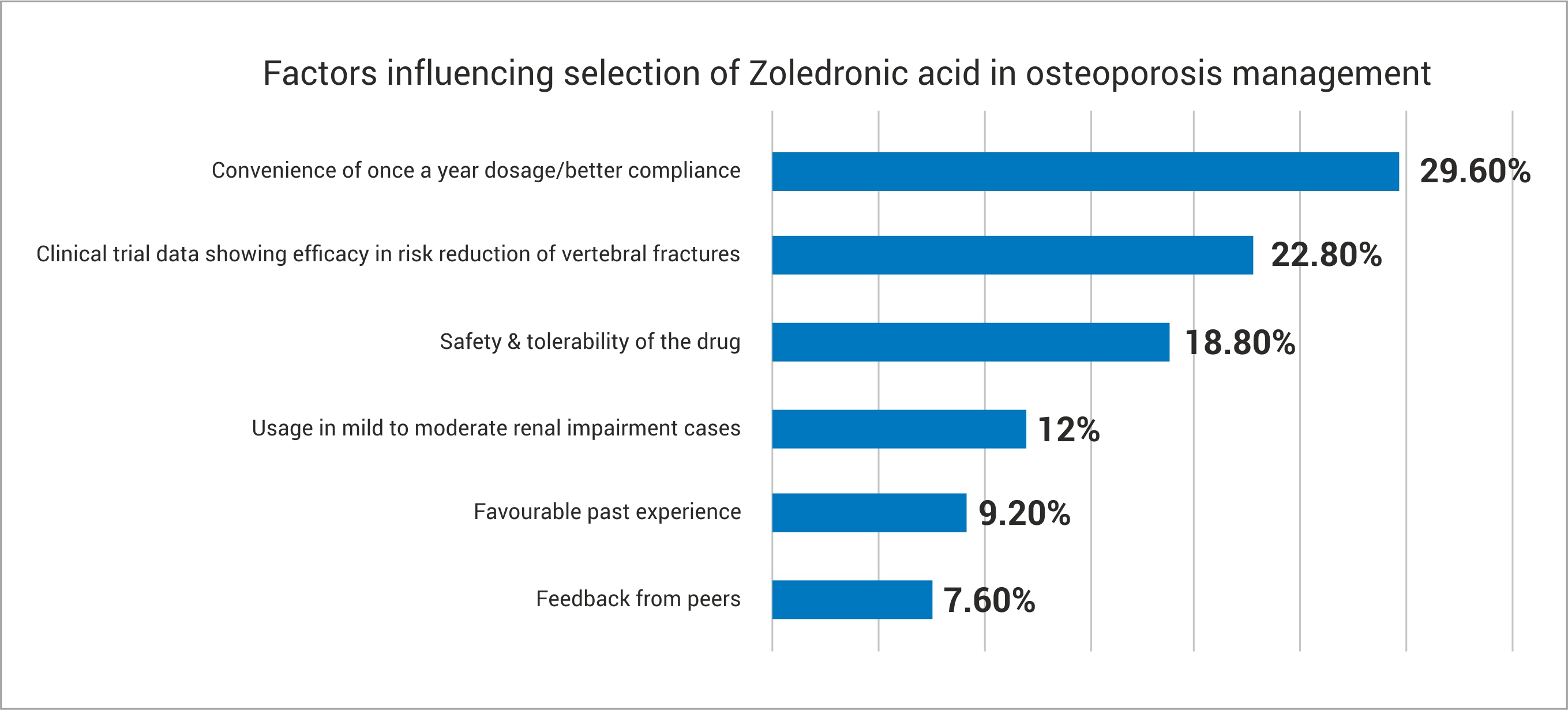
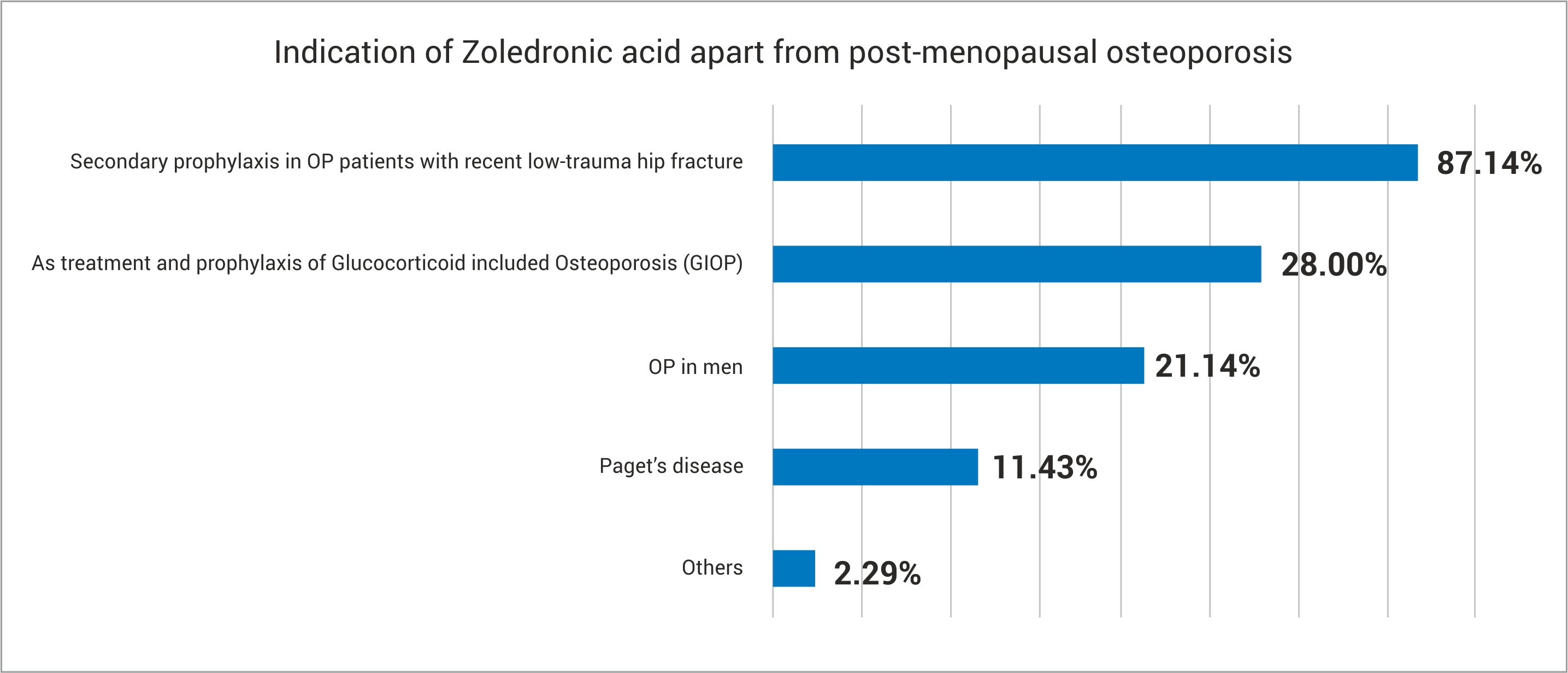
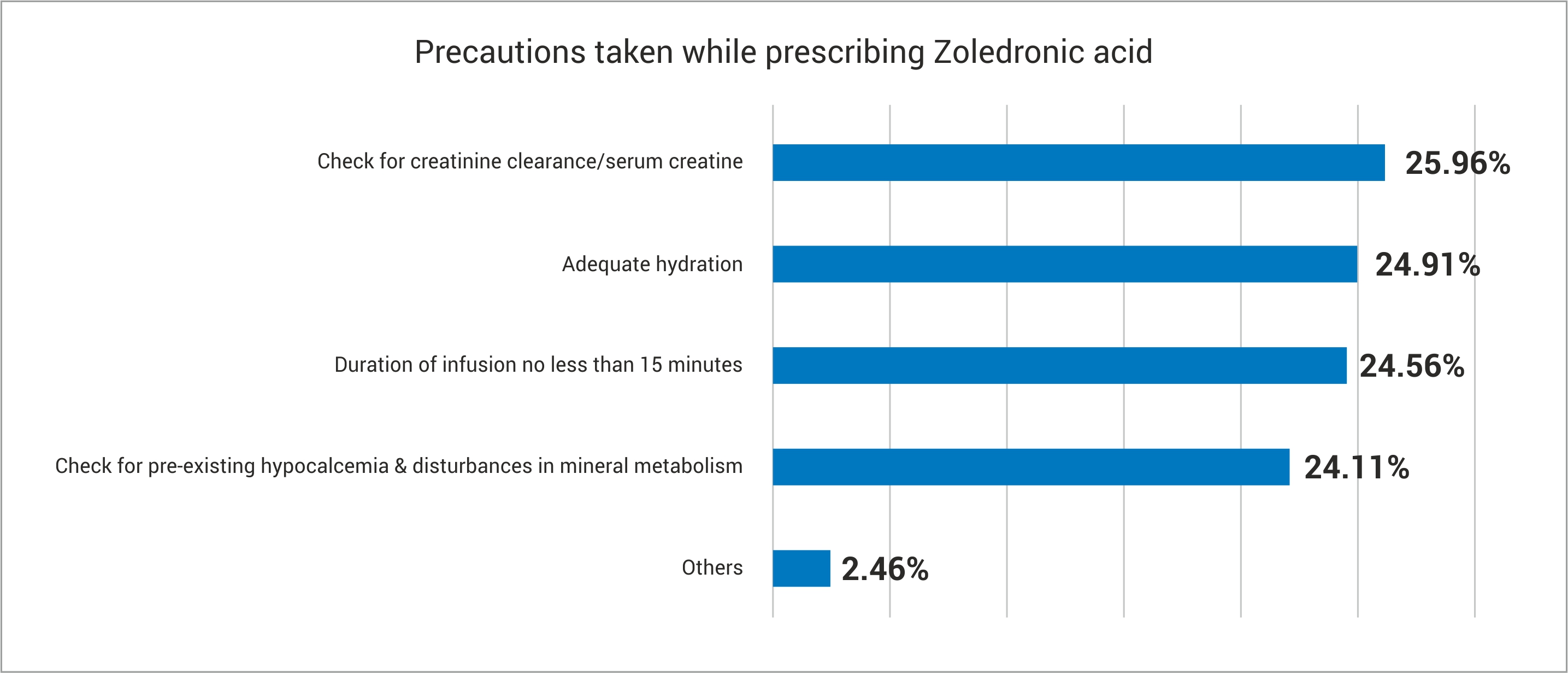
The various factors influencing selection of ZA, indications for starting ZA in patients other than post-menopausal osteoporosis, and precautions taken with ZA administration by the respondents are summarized in [Table/Fig-5].
Zoledronic acid in OP: (a) Factors influencing ZA selection; (b) Indications of ZA apart from PMO; (c) Precautions taken while prescribing ZA
Flu-like reactions, which are the expected side-effects seen with ZA, were seen in 2-5% of patients prescribed with the drug by almost one-third of the respondents (31.33%), and 84.34% of the respondents routinely prescribed antipyretic and/or anti-allergic medications to reduce this side effect.
Intranasal Calcitonin in osteoporosis: The clinical profile of patients in whom the responds considered calcitonin intranasal therapy are summarized in [Table/Fig-6].
Patient profile for initiating calcitonin intranasal therapy
| Clinical Profile | No of Respondents (%) | Clinical Profile | No of Respondents (%) |
|---|
| Fracture | 19 (22.62%) | Post-menopausal OP | 13 (15.48%) |
| Backache/ Bone pain | 9 (10.71%) | Age | 7 (8.33%) |
| Severe OP | 4 (4.76%) | Osteopenia | 3 (3.57%) |
| Sex | 2 (2.38%) | Myalgia | 2 (2.38%) |
Factors prompting the respondents to introduce intranasal calcitonin for osteoporosis management included significant analgesic efficacy (21.81%), ease of administration (19.94%), no need for hospitalization (18.69%), better tolerability (15.58%), dosage convenience (15.26%), and the presence of clinical trial data (8.72%).
Most respondents prescribed 200 IU (1 puff) nasal calcitonin per day, for a duration of 3-6 months, and most (90.91%) respondents felt that the analgesic efficacy was the key factor which differentiated nasal calcitonin over other therapies. Among those respondents who used intranasal calcitonin, 76.6% reported good tolerability, while 21.27% reported excellent tolerability.
Finally, as for incidence of nasal irritation and rhinitis with calcitonin, 63.41% of the respondents replied that such a reaction was found in only 0-1% of their patients. For these patients, the prospect of introducing oral calcitonin was reported to be favorable by 58.23% of the respondents, and the reasons given were improved compliance and better efficacy.
Discussion
In spite of all the advances in medicine, no treatment modality exists which can completely reverse established osteoporosis. For those patients in whom osteoporosis is diagnosed early, appropriate and prompt medical intervention can retard the progression of the condition, and improve the quality of life [1]. There are various recommendations regarding the diagnosis and management of osteoporosis, such as the American Association of Clinical Endocrinologists (AACE) guidelines, guidelines by the National Osteoporosis Foundation (NOF), American College of Physicians (ACP) guidelines, and the European guidelines [4–7].
Though all of these guidelines are based on the best available evidence, the presence of these and other guidelines, the actual scenario at the ground level is rarely documented.
The purpose of the present survey was to explore the real-world clinical practice scenario of the management of osteoporosis in India. We collected information under various heads as detailed in the previous section for a better understanding of the clinical situation from all possible viewpoints.
Epidemiology and Patient Impact of osteoporosis: The peak incidence of osteoporosis occurs at about 70-80 years of age in the Western countries; however, in India it usually afflicts at least 1 or 2 decades earlier, viz. the age group of 50-60 years [2]. Though the overall prevalence value of osteoporosis in India has not been estimated satisfactorily, the prevalence of osteoporosis in Indian males above 50 years is estimated to be around 8.5% [8] and in peri- and post-menopausal women is about 53% [9]. Our study reported similar epidemiological parameters in that there was female preponderance, and most of the patients belonged to the age group 51-60 years. The fact that osteoporosis also causes an adverse impact on interpersonal relationships and depression has been highlighted previously [10]. Despite being a widespread health condition having a large impact on patient life, the diagnosis and treatment rates of osteoporosis in India are presumed to be very low. Health education activity and improving doctor access to patients is the need of the hour to tackle this problem.
Though it has been presented that the first indication of osteoporosis is a fracture, most respondents in our survey initially reported that the commonest initial presentation was general symptoms.
Management of osteoporosis: BMD estimation by DEXA was the most favoured initial investigation of most of the respondents. This observation goes in accordance with the guidelines that DEXA is the gold-standard tool for osteoporosis diagnosis [11].
Though biochemical markers of bone turnover have contributed to a better understanding of pathophysiology of osteoporosis and other metabolic bone disorders, they are not usually considered necessary for the initial diagnosis of osteoporosis. The most important reason for this is the wide analytical and biological variability of the markers [12]. Even in our study, biochemical markers were not a popular tool for the diagnosis of osteoporosis.
In addition to lifestyle modifications, the two most popular treatment modalities of osteoporosis among the respondents were calcium-and-vitamin D, and bisphosphonates. Most respondents reserved treatment options like teriparatide, calcitonin and Denosumab to special conditions such as severe osteoporosis and vertebral fractures. This is in accordance with the guidelines by AACE and ACP [4,6] which prescribe that calcium and vitamin D supplementation should accompany all treatment modalities, and that bisphosphonates (except ibandronate) are the first-line agents.
Though the most frequently used therapy for osteoporosis is oral bisphosphonates, its long average duration of therapy and the tendency of oral bisphosphonates to cause gastrointestinal side effects can be associated with other practical problems such as increased cost of therapy and poor compliance. This finding from our study has also been reported previously [13]. Perhaps this was the reason why once-a-month scheduling of oral bisphosphonates was the most preferred regime by the respondents. On the other hand, though initially IV bisphosphonates were used in oncology, their use in osteoporosis is gaining popularity (especially Zoledronic acid) in view of their not being associated with GI side effects and poor compliance [14].
Most of the respondents began therapy for osteoporosis in accordance with the NOF guidelines [5] which recommend that pharmacotherapy for osteoporosis should be started only in post-menopausal women and men aged ≥ 50 years who have:
A hip or vertebral fracture.
T-score of -2.5 or less at the femoral neck or spine after appropriate evaluation to exclude secondary causes.
Low bone mass (T-score between -1.0 and -2.5 at the femoral neck or spine) and a 10-year probability of a hip fracture of 3% or greater or a 10-year probability of a major osteoporosis-related fracture of 20% or greater based on the US-adapted WHO algorithm.
Zoledronic Acid (ZA) in osteoporosis: ZA is the newest and most potent bisphosphonate, which is available only as an IV preparation. Small doses of ZA are enough to produce significant inhibition of bone resorption. Longer dosing intervals of ZA and a lower incidence of GI side effects can improve patient compliance [15].
A potential for acute renal failure or renal function impairment has been reported with the use of ZA. This is linked to the formation of insoluble complexes in the blood, and is correlated with dose and rate of infusion. As a result, it is recommended that ZA infusion should be slow and after considerably diluted. Further, renal function impairment has not been reported with annual (4 mg), biannual (2 mg) and quarterly (0.25 – 1 mg) use of ZA [14].
Most of the results of the present study closely correlated with these findings. While convenience of dosing regimen, safety and efficacy from clinical trials encouraged them to initiate ZA therapy, cost, availability, uncertainty about evidence, and safety concerns were the factors which deterred the respondents from using ZA in a more widespread fashion. Those who initiated ZA therapy prescribed it in specific patients, such as those with history of recent low-trauma fracture and those with glucocorticoid-induced osteoporosis. Most respondents also took precautions such as checking for renal functioning, hydration, pre-existing hypocalcemia and mineral metabolism disturbances, and also ensured that the infusion was continued for duration of not less than 15 minutes.
Intranasal Calcitonin in osteoporosis: Calcitonin is a naturally occurring peptide hormone which acts through specific receptors on osteoclasts and decreases their activity, thereby reducing bone loss. Out of all recombinant or synthetic variants of calcitonin that were introduced in the market, salmon calcitonin is the most popular product. Calcitonin is mostly administered as an intranasal spray because of its convenience of administration, at a single daily spray providing 200 IU of the drug. As with other osteoporosis therapies, calcitonin therapy is recommended to be used in conjunction with calcium and vitamin D supplementation [1,16].
Calcitonin diminishes bone pain due to osteoporotic vertebral fractures, and is usually reserved for patients with vertebral crush fractures and also for those patients who are not candidates for the other available osteoporosis treatments. Adverse effects of intranasal calcitonin include rhinitis, epistaxis and allergic reactions, especially in patients with a history of allergy to salmon [5,16].
In the present study, respondents mostly used intranasal calcitonin in patients with fracture, backache, bone pain, and in post-menopausal osteoporosis patients, especially when they were looking for features like improved analgesia, improved ease of administration, better tolerability profile, mitigating need for hospitalization, and patient convenience. The major limitation of this study is the small sample size of 84 participants.
Conclusion
The current clinical practice scenario of osteoporosis management in India largely adheres with various clinical practice guidelines for osteoporosis. Lack of patient compliance can be a serious issue and can hamper the clinician’s attempts at preventing fractures due to osteoporosis. The main factors leading to such a reduction in patient compliance include side effects, frequency and lengthy duration of therapy with bisphosphonates. One possible solution to this can be the widespread popularization of ZA which needs to be prescribed only once yearly, and of calcitonin which is associated with increased patient convenience and low incidence of side effects.