Fibroids in pregnancy is a commonly encountered clinical entity. Objective of this study was to evaluate the maternal and fetal outcome in women having pregnancy with uterine fibroids. We present the clinical, obstetric data, perinatal outcomes of 15 patients from a prospective study. Fifteen pregnant women with fibroid >3cm were prospectively included in study. Major proportion of patient with fibroids were in younger age group of 25-30 years when compared to older age group of 31-35 years (66% vs 33%). Fibroids were more frequent in multi-gravidae, compared to primigravidae. In almost half of patients, (53.3%) fibroids were diagnosed before pregnancy. Common complications encountered during pregnancy in decreasing order of frequency were pain abdomen (46.6%), followed by threatened preterm labour (26.6%) and anaemia (26.6%). Out of 15, three (20%) women had abortion. In remaining, 11/12 patients attained term pregnancy between 37 to 40 weeks. Two patients required antenatal myomectomy. Caesarean section was done in 75% of women who attained term pregnancy and one patient had technical difficulty during caesarean section. Post partum heamorrhage was seen in 5/15 (33.3%) of patients. Out of 12, five babies were low birth weight. Four babies required NICU admission. There was no perinatal mortality. In our small patient series high incidence of caesarean section rates and increased incidence of threatened preterm labour, anaemia, and postpartum haemorrhage, was observed in pregnant patients with fibroids and hence, the pregnancy with fibroids should be considered as high risk pregnancy.
Introduction
Uterine fibroids (leiomyomas) are benign smooth muscle tumors of the uterus. They are found in approximately 20–50% of women of reproductive age [1]. Incidence of fibroids varies from 0.1% to 12.5% [2]. Incidence of fibroids increases with maternal age at pregnancy [2]. Fibroid less than 5 cm in diameter tend to remain stable or decrease in size [3–5] and, larger fibroids (>5 cm) tend to grow during the pregnancy [5]. The risk of adverse events in pregnancy increases with the size of the fibroid [6]. Different complications with variable rates of incidence have been reported in pregnancy with fibroids which include ante-partum haemorrhage, acute abdomen, laparotomy, preterm labour, foeto-pelvic disproportion, malposition of the foetus, retention of the placenta, postpartum haemorrhage, red degeneration, dysfunctional labour, retained placenta, and retained products of conception, intra uterine growth restriction (IUGR) [7–11]. These complications are more commonly seen with large submucosal and retroplacental fibroids [6]. Despite the high incidence of all these adverse events during pregnancy, perinatal outcomes in these patients tend to be fair [9]. Due to risk of all these complications pregnancy with fibroids has been a topic of research for many years. However, there is paucity of literature involving Asian population and especially Indian population [1,12,13]. In this context, this prospective study was planned to assess the outcome of pregnancy in patients with uterine fibroids involving Indian population and we present the case series of 15 patients with their demographic, clinical and obstetric data and perinatal outcomes.
Characteristics of Patients
All the findings are summarized in [Table/Fig-1,2,3,4,5 and 6]. Fifteen (6- primi and 9-multi gravidae) patients were included in this study. Mean age was 28.9 years. History of recurrent pregnancy loss was present in 7 patients. Six patients were primigravida and 9 were multigravida, of which four patients had history of more than three recurrent abortions, obstetric history of 2 abortions were seen in 2 patients and 1 patient had previous history of single abortion. Of 9 who underwent LSCS, 4 had LSCS at request (two patients also had combined indications such as recurrent pregnancy loss with precious pregnancy), 2 were done for myomectomy scar, 3 for non progress of labour.
Maternal demographic characteristics: n=15
| S. no | Age | Parity | Type ofConception | H/O abortions | Time ofDiagnosis |
|---|
| 1 | 28 | G1 | S | No | 12 weeks |
| 2 | 28 | G3A2 | S | Yes | 14 weeks |
| 3 | 32 | G4A3 | S | Yes | Before pregnancy |
| 4 | 31 | G1 | IVF | No | Before pregnancy |
| 5 | 26 | G1 | S | No | 16 weeks |
| 6 | 28 | G4A3 | OI | Yes | Before pregnancy |
| 7 | 30 | G4A3 | OI | Yes | Before pregnancy |
| 8 | 32 | G4A3 | IVF | Yes | Before pregnancy |
| 9 | 28 | G3A2 | OI | Yes | 14 weeks |
| 10 | 26 | G1 | S | No | 16 weeks |
| 11 | 27 | G2A1 | S | Yes | Before pregnancy |
| 12 | 28 | G2P1L1 | S | No | Before pregnancy |
| 13 | 27 | G2P1L1 | S | No | Before pregnancy |
| 14 | 28 | G1 | OI | No | 16 weeks |
| 15 | 26 | G1 | S | No | 28 weeks |
S- Spontaneous, OI-ovulation induction, IVF-Invitro fertilization, G-Gravida, P-Para, L-living, A-Abortion
Ultrasound characteristics fibroid: n= 15
| S. no | Number | Site | Size (cm) |
|---|
| 1 | Single | IM-Ant, LUS | 5-10 |
| 2 | Single | IM-Post | 5-10 |
| 3 | Single | IM-Ant, fundal | >10 |
| 4 | Single | IM-Ant, fundal | <5 |
| 5 | Single | SS, Pedunculated | >10 |
| 6 | Multiple | SSIM-fundal IM-Ant | >10<5 |
| 7 | Multiple | IM-FundalIM-Ant | >10<5 |
| 8 | Single | IM-Post | 5-10 |
| 9 | Single | IM-Ant | >10 |
| 10 | Single | IM-fundal | <5 |
| 11 | Multiple | SSIM | >10<5 |
| 12 | Multiple | SSIM-Ant | 5-10<5 |
| 13 | Single | IM-post | <5 |
| 14 | Multiple | SSIM-Ant | <55-10 |
| 15 | Single | IM-post | <5 |
SS-Subserosal, IM-Intramural
Antenatal complications: n= 15
| S. no | Abortions | Anaemia | Pain abdomen | PPROM | ThreatenedPreterm | IUGR | APH | Antenatalmyomectomy |
|---|
| 1 | N | Y | Y | N | Y | Y | N | N |
| 2 | N | N | Y | N | N | N | N | N |
| 3 | N | Y | Y | N | Y | N | N | N |
| 4 | N | N | N | N | N | Y | N | N |
| 5 | N | N | Y | N | N | N | N | Y |
| 6 | N | Y | Y | Y | Y | Y | N | Y |
| 7 | Y | N | Y | N | Y | N | N | N |
| 8 | N | N | N | N | N | Y | N | N |
| 9 | N | N | N | N | N | N | N | N |
| 10 | N | Y | Y | N | N | N | N | N |
| 11 | Y | N | N | N | N | N | N | N |
| 12 | Y | N | N | N | N | N | N | N |
| 13 | N | N | N | N | N | N | N | N |
| 14 | N | N | N | N | N | Y | N | N |
| 15 | N | N | N | N | N | N | N | N |
PPROM- Preterm Premature rupture of membranes, IUGR- Intrauterine growth restriction, APH- antetarum haemorrhage, Y-Yes, N-No
Intrapartum variables, n=12
| S. no | GA at delivery | Mal-presentation | PROM | Obstructedlabour | Prolongedlabour | PPH | Technicaldifficultiesduring delivery | Adherentplacenta |
|---|
| 1 | Term | N | N | N | N | N | N | N |
| 2 | Term | N | Y | N | Y | Y | N | N |
| 3 | Term | N | Y | N | Y | Y | Y | N |
| 4 | Term | N | N | N | N | N | N | N |
| 5 | Term | N | N | N | N | N | N | N |
| 6 | 34 weeks | N | N | N | N | Y | N | N |
| 7 | - | - | - | - | - | - | - | - |
| 8 | Term | N | N | N | N | Y | N | N |
| 9 | Term | N | N | N | N | N | N | N |
| 10 | Term | N | Y | N | Y | Y | N | N |
| 11 | - | - | - | - | - | - | - | - |
| 12 | - | - | - | - | - | - | - | - |
| 13 | Term | N | N | N | N | N | N | N |
| 14 | Term | N | N | N | N | N | N | N |
| 15 | Term | N | N | N | N | N | N | N |
GA-gestational age, PROM-Premature rupture of membranes, PPH-Post partum haemorrhage, Y-Yes, N-No
Postpartum variables, n= 12.
| S. no | Blood transfusion | Sepsis | Subinvolution | Reduction in size offibroid | Vaginal delivery | LSCS |
|---|
| 1 | Y | N | Y | Y | Y | N |
| 2 | N | N | Y | Y | N | Y (non progress of labour) |
| 3 | Y | Y | Y | N | N | Y (non progress of labour) |
| 4 | N | N | N | Y | N | Y (Maternal request) |
| 5 | N | N | N | Y | N | Y (Myomectomy scar) |
| 6 | Y | Y | N | Y | N | Y Myomectomy scar) |
| 7 | - | - | - | - | - | - |
| 8 | Y | N | Y | N | N | Y (Maternal request) |
| 9 | N | N | N | Y | N | Y (Maternal request) |
| 10 | Y | N | Y | Y | N | Y (non progress of labour) |
| 11 | - | - | - | - | - | - |
| 12 | - | - | - | - | - | - |
| 13 | N | N | N | Y | Y | N |
| 14 | N | N | Y | Y | N | Y (Maternal request) |
| 15 | N | N | N | Y | Y (Vaccuum) | N |
LSCS-Lower segment caesarean section, Y-Yes, N-No
| S. no | Term | Birth weight | Birth asphyxia | NICU admission |
|---|
| 1 | Y | 2.25 | N | Y (Hyperbilirubinemia) |
| 2 | Y | 2.8 | N | N |
| 3 | Y | 2.9 | N | N |
| 4 | Y | 2.4 | N | Y (Hyperbilirubinemia) |
| 5 | Y | 2.8 | N | N |
| 6 | N | 2 | Y | Y (RDS, Prematurity) |
| 7 | - | - | - | - |
| 8 | Y | 2.4 | N | N |
| 9 | Y | 2.8 | N | N |
| 10 | Y | 2.8 | N | N |
| 11 | - | - | - | - |
| 12 | - | - | - | - |
| 13 | Y | 2.75 | N | N |
| 14 | Y | 2.3 | Y | Y (Asphyxia) |
| 15 | Y | 2.6 | N | N |
RDS- respiratory distress Syndrome, Y-Yes, N-No
Majority of the patients (8/15) had prenatal diagnosis of fibroids. Majority of patients had single fibroid and one thirds had multiple fibroids. Most common location of fibroids was intramural followed by subserosal location. Around 20% (3/15) of the patients had early pregnancy loss. Majority of the patients had (11/12) term pregnancy. Pain was the most frequently noted complication followed by threatened preterm, and anaemia. High incidence of PPH, and IUGR were noted.
There was one preterm baby, who developed RDS (8.3%). The incidence of IUGR was 41.6% (5/12). Four babies (33.3%) were admitted in NICU. There was no neonatal death noted in our study.
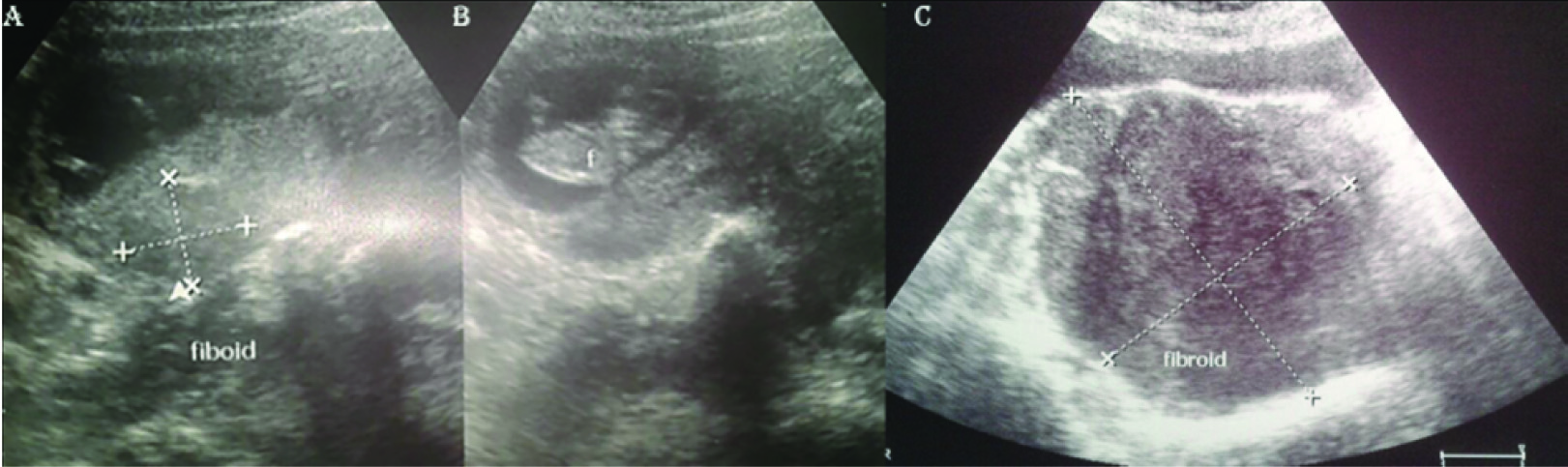
USG findings of few patients are shown in [Table/Fig-7A-C].
A) Longitudinal ultrasound images showing live intrauterine gestation; B) 2.5X2.5cm fibroid. This patient had uneventful course during pregnancy; C) Longitudinal ultrasound images of uterus showing a large intramural fibroid of size 12x8 cm. This patient had an early abortion
Discussion
This study was conducted to evaluate the outcome of pregnancies complicated by leiomyomas. Mean maternal age in our study was found to be 28.9 years, which is comparable to other studies, showing occurrence of leiomyomas in second and third decades of life [1,13].
We found that fibroids were less frequent in first pregnancy compared to multigravidae. This is in consistent with earlier studies by Noor et al., [13] (73.33% multigravida and 23.66% primigravida) and Sarwar et al., [1] (63% multigrvida and 37% primigravida). Regarding obstetric complications, in our study, 3 out of 15 patients (20%) had abortion. High incidence of abortions in patients with fibroids is in agreement with results from earlier studies [1,9]. The proposed mechanism is compressed endometrial vascular supply, affects the fetus adversely resulting in abortion [1]. In our study, 7/15 (47%) had significant pain abdomen, which is slightly higher to results reported in the prior studies [1,3,9,14]. These patients were managed by bed rest, analgesics and reassurance. Cause of pain was due to red degeneration, which is thought to be result of effect of progresterone on fibroids, and occurs more commonly in pregnancy [12].
Though 4/15 (26.6%) patients had history of threatened preterm labour during pregnancy, 11 (73.3%) patients had continued their pregnancy till term and only one patient (7%) had preterm delivery at 34 weeks of gestation due to PPROM. The incidence of preterm delivery was low in our study compared to study by Sarwar et al., (33.3%) [1]. We reported slightly increased incidence of PROM, (3/15, 20%) compared to Sarwar et al., (10%). Anaemia was found in four patients (26.6%), comparable with study by Noor et al., (20.6%) [13].
Regarding mode of delivery, 3 patients had spontaneous onset of labour. Of 12 patients, 9 had LSCS, 2 had spontaneous vaginal delivery and 1 patient was delivered by ventouse assistance. This is similar to studies by Noor et al., (70%) and three folds higher, compared to studies by Sarwar et al., (2.6%) [1,13].
In our patient population, 5 patients (33.3%) had PPH, similar to study by Noor et al., (33.3%) and slightly high, compared with 14% in study by Lam et al., [13,15]. Only one patient had technical difficulty during caesarean section, owing to the larger fundal fibroid, similar to Sarwar et al., [1]. However, no patient in our study required casearean hysterectomy, as compared to13.33% in Noor et al., study [13], Caserean myomectomy should be avoided unless fibroid is in line of incision. Two of our patients underwent myomectomy, at 14 to 16 weeks of gestation, one for torsion of pedunculated subserosal fibroid and another for multiple subserosal and intramural fibroids with pain abdomen resistant to conservative management.
Surgical management is reserved in patients with subserosal and pedunculated fibroids with pain and who do not respond to conservative management. Other complications like obstructed labour, adherent placenta, uterine inversion, malpresentation, placentaprevia, abruption placentae, prolapse of pedunculated fibroid through cervix, reported in earlier studies were not observed in our study [8–10,12,15].
Conclusion
Pregnancy with fibroids is associated with various adverse events during pregnancy which included but not limited to high caesarean section rates, threatened preterm labour, anaemia, post partum haemorrhage, and hence, it should be considered as high risk pregnancy.
S- Spontaneous, OI-ovulation induction, IVF-Invitro fertilization, G-Gravida, P-Para, L-living, A-Abortion
SS-Subserosal, IM-Intramural
PPROM- Preterm Premature rupture of membranes, IUGR- Intrauterine growth restriction, APH- antetarum haemorrhage, Y-Yes, N-No
GA-gestational age, PROM-Premature rupture of membranes, PPH-Post partum haemorrhage, Y-Yes, N-No
LSCS-Lower segment caesarean section, Y-Yes, N-No
RDS- respiratory distress Syndrome, Y-Yes, N-No
[1]. Sarwar I, Habib S, Bibi A, Malik N, Parveen Z, Clinical audit of foeto maternal outcome in pregnancies with fibroid uterusJournal of Ayub Medical College, Abbottabad: JAMC 2012 24(1):79-82. [Google Scholar]
[2]. Laughlin SK, Baird DD, Savitz DA, Herring AH, Hartmann KE, Prevalence of uterine leiomyomas in the first trimester of pregnancy: an ultrasound-screening studyObstetrics and gynecology 2009 113(3):630-35. [Google Scholar]
[3]. Rice JP, Kay HH, Mahony BS, The clinical significance of uterine leiomyomas in pregnancyAmerican journal of obstetrics and gynecology 1989 160(5 Pt 1):1212-16. [Google Scholar]
[4]. Strobelt N, Ghidini A, Cavallone M, Pensabene I, Ceruti P, Vergani P, Natural history of uterine leiomyomas in pregnancyJournal of ultrasound in medicine: official journal of the American Institute of Ultrasound in Medicine 1994 13(5):399-401. [Google Scholar]
[5]. Akhtar N, Sulthana S, Zabin F, Successful Outcome of pregnancy with large fibroid uterus- a case reportBangladesh J Obstet Gynaecol 2010 25(2):87-9. [Google Scholar]
[6]. Ciavattini A, Clemente N, Delli Carpini G, Di Giuseppe J, Giannubilo SR, Tranquilli AL, Number and size of uterine fibroids and obstetric outcomesThe journal of maternal-fetal & neonatal medicine 2015 28(4):484-88. [Google Scholar]
[7]. Hasan F, Arumugam K, Sivanesaratnam V, Uterine leiomyomata in pregnancyInternational journal of gynaecology and obstetrics 1991 34(1):45-48. [Google Scholar]
[8]. Katz VL, Dotters DJ, Droegemeuller W, Complications of uterine leiomyomas in pregnancyObstetrics and gynecology 1989 73(4):593-96. [Google Scholar]
[9]. Klatsky PC, Tran ND, Caughey AB, Fujimoto VY, Fibroids and reproductive outcomes: a systematic literature review from conception to deliveryAmerican journal of obstetrics and gynecology 2008 198(4):357-66. [Google Scholar]
[10]. Koike T, Minakami H, Kosuge S, Usui R, Matsubara S, Izumi A, Uterine leiomyoma in pregnancy: its influence on obstetric performanceThe journal of obstetrics and gynaecology research 1999 25(5):309-13. [Google Scholar]
[11]. Lev-Toaff AS, Coleman BG, Arger PH, Mintz MC, Arenson RL, Toaff ME, Leiomyomas in pregnancy: sonographic studyRadiology 1987 164(2):375-80. [Google Scholar]
[12]. Gupta S, Manyonda IT, Acute complications of fibroidsBest practice & research Clinical obstetrics & gynaecology 2009 23(5):609-17. [Google Scholar]
[13]. Noor S, Fawwad A, Sultana R, Bashir R, Quratul A, Jalil H, Pregnancy with fibroids and its and its obstetric complicationJournal of Ayub Medical College, Abbottabad: JAMC 2009 21(4):37-40. [Google Scholar]
[14]. Levy G, Hill MJ, Beall S, Zarek SM, Segars JH, Catherino WH, Leiomyoma: genetics, assisted reproduction, pregnancy and therapeutic advancesJ Assist Reprod Genet 2012 29(8):703-12. [Google Scholar]
[15]. Lam SJ, Best S, Kumar S, The impact of fibroid characteristics on pregnancy outcomeAmerican journal of obstetrics and gynecology 2014 211(4):e1-395. [Google Scholar]