A well-functioning vascular access is essential for providing efficient dialysis therapy. Vascular access complications are the leading cause of morbidity in dialysis population and add to high healthcare costs. There are three types of vascular access: native arteriovenous fistula (AVF), arteriovenous grafts (AVG) and central vein catheter (CVC) [1].
AVF have lower complication rates, better patency rates, better access and patient survival as compared to catheter and arteriovenous grafts (AVGs). Central venous catheters are used for rapid access for immediate dialysis, and alternative vascular access is not available or has failed [1]. Catheter use is linked to higher rates of infection and its complications. Early diagnosis of CKD allows creation of native AVF in predialysis stage and, consequently, usage of a temporary catheter can be avoided.
Aim of the present study is to assess the different types of vascular access in chronic kidney disease patients on haemodialysis, their location, failure rate, and associated complications.
Materials and Methods
This prospective observational study was carried out in our institute between January 2014 and December 2014. All patients who were initiated on haemodialysis for CKD stage V in our center during the above period were included in the study. Prevalent patients already on maintenance haemodialysis were excluded. There was 50 incident CKD patients initiated on haemodialysis and were included in the study. Patients were advised surgery for AVF when diagnosed with stage IV CKD. Central venous catheter (CVC) was inserted only in cases who presented late and required HD before creation or maturation of fistula. Dual–lumen polyurethane non-cuffed non-tunneled HD catheters (MAHURKAR™* 11.5Fr Dual Lumen Acute Dialysis Catheter, USA) were inserted under strict asepsis and sutured to the skin. Physical examination of arteries and the veins, and Allen’s test were performed in all patients before AVF surgery. Preoperative colour doppler of upper limb veins and arteries was done in selected patients to look for size and patency. The data collected included patient demographics, co-morbidities, details of basic disease, date, location and type of CVC and AVF, operative details, patency, complications, and mortality. All patients underwent twice weekly four hour session of haemodialysis.
Statistical Analysis
The data was analysed using SPSS (Statistical Package for Social Sciences version 20). Continuous variables were presented as means±SD while categorical variables were presented as percentages.
Results
During 2014, 50 patients were initiated on Haemodialysis for CKD in our dialysis unit. The demographic data of the study patients are tabulated in [Table/Fig-1]. The most common cause of End Stage Renal Discase (ESRD) was diabetic nephropathy (38%). All the study patients underwent HD twice weekly. Co-morbid conditions included diabetes mellitus in 46% and hypertension in 72% of the patients.
Baseline characteristics of study patients
| Number of patients | 50 |
| Age (Mean±SD) | 51.28 ± 2.32 years |
| Males | 33 (66%) |
| Females | 17(34%) |
| Weight (Mean±SD) | 57.14 ± 12.81kg |
| Diabetes | 46% |
| Hypertension | 72% |
| Number of CVC inserted | 58 |
| Number of AVF created | 40 |
| Number of AVF successfully cannulated | 30 (75%) |
Seven patients (14%) had access failure and the remaining 43 (86%) were incident patients. Only 9.3% patients had planned dialysis initiation whereas 90.7% patients had unplanned dialysis initiation. The main cause of unplanned haemodialysis was previously undiagnosed CKD, patients declining for elective dialysis initiation, and acute exacerbation of chronic kidney disease, due to an intercurrent illness such as dehydration, sepsis and nephrotoxic drugs. Initial access was CVC in 48(96%) patients and AVF in two (4%) patients. Two patients who had planned dialysis initiation started dialysis through catheter due to delayed maturation of fistula.
A total of 58 catheters were inserted in 48 patients. Catheter was inserted in right internal jugular vein (93.1%), left internal jugular vein (5.17%) and left femoral vein (1.73%). The maximum number of catheters in a single individual over the study period was three in two patients who had no alternative dialysis access. Twenty (34.48%) of the 58 catheters inserted were complicated by catheter related sepsis. Parenteral use of antibiotics was successful in 10 (50%) patients. Eight catheters (40%) had to be removed to control infection and two (10%) patients died despite catheter removal and antibiotics. During follow-up, 48 catheters were removed. The reasons for removal of catheter in ESRD patients were elective removal (50%), catheter related sepsis (CRS) (20.83 %), thrombosis (6.25%) and others (22.91%). Catheter survival ranged between 32 and 129 days with a mean survival of 77.23 ± 14.8 days.
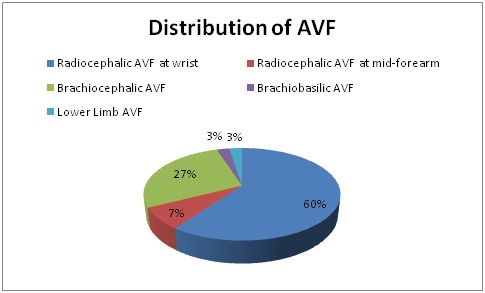
A total of 40 AVFs were created in 34 patients. Five patients required repeat procedure due to failure of previous fistula. Thirteen (32.5%) fistulas were done on right side and 26 (65%) were done on left side. Radio-cephalic AVF was the most common fistula followed by others as mentioned in [Table/Fig-2]. The various sites, artery and vein used for AVF creation in our patients are tabulated in [Table/Fig-3]. Lower limb AVF was created in one patient (2.5%) due to poor caliber of upper limb veins. End (vein) to side (artery) anastomosis was done in all cases [Table/Fig-4].
Sites of distribution of AVF
Details of AVF creation and complications
| Site of AVF | Wrist – 60% |
| Forearm – 7.5% |
| Arm – 30% |
| Lower limb – 2.5% |
| Vein | Cephalic vein – 82.5% |
| Ante cubital vein – 12.5% |
| Brachial vein – 2.5% |
| Great saphenous vein – 2.5% |
| Artery | Radial artery - 67.5% |
| Brachial artery - 30% |
| Posterior tibial artery - 2.5% |
| Complications | Limb oedema-17.5% |
| Venous hypertension-2.5% |
| Primary failure | 25% |
| Causes: maturation failure (12.5%), and thrombosis (12.5%). |
| Secondary Failure | 10% due to thrombosis |
Brachio-cephalic fistula-End to side anatamosis

Complications include distal oedema in 7 (17.5%) patients and venous hypertension in one (2.5%) patient. Primary failure occurred in 10 (25%) patients due to maturation failure (50%), and thrombosis (50%). Presence of diabetes was the most important risk factor for primary failure (p-value - 0.01). Secondary failure due to thrombosis occurred in 3 (10%) patients. One patient had her AVF recanalised after intravenous heparin. AVF failure occurred more commonly in distal fistulas (76.92%, p-value < 0.05) in our series. Patients older than 60 years (p-value < 0.05) had more fistula failures compared to young patients.
The mean period before cannulation was 46.65±2.55 days in patients who had successful AVF creation. Ten patients (26.31%) starting dialysis with a CVC remain to be catheter dependent at 90 days of which 80% (p-value < 0.05) were > 60 years of age. There were 10 deaths during follow up period including two patients who died of catheter related sepsis.
Discussion
Dialysis vascular access is at the same time both the ‘lifeline‘ and the ‘Achilles heel’ of haemodialysis. Hence, successful HD depends on creation and maintenance of adequate vascular access. Haemodialysis can be done through various types of vascular access namely venous catheters, AV fistula and graft, each with its own merits and demerits [Table/Fig-5] [2,3]. Though AVF is considered to be the ideal choice of vascular access for haemodialysis, many patients in India initiate dialysis through catheters.
Comparison of various types of vascular access [2,3]
| Vacular access | Catheter | AVF | AVG |
|---|
| Advantages | -universally applicable to all patients-can be inserted into multiple sites relatively easily-can be used immediately-No maturation time needed-Skin puncture not required-No short-term Haemodynamic consequences-lower initial costs and replacement costs | -lower rate of complications-the lowest rate of thrombosis-require the fewest interventions, -longer survival of the access-costs of implantation and access maintenance are the lowest-lower rates of infection than grafts-less prone to infection than percutaneous catheters | -large surface area available for cannulation initially.-technically easy to cannulate-lag-time from insertion to maturation is short-Multiple insertion sites are available-A variety of shapes and configurations is available |
| Disadvantages | -High morbidity caused by thrombosis, infection-risk for permanent central venous stenosis-discomfort and cosmetic disadvantage of an external appliance.-Shorter expected life-Lower blood flow rates | -lag time of 4-6 weeks from creation to maturation-high primary failure rates | -number of access events is 3 to 7 fold greater in prosthetic grafts than in native fistulae-lower cumulative patency than fistulas |
| Mortality | -catheter use being consistently associated with the worst survival rates | -Fistulae are associated with increased survival and lower hospitalization. | -Patients receiving catheters and grafts have a greater mortality risk than patients with fistulae |
| Complications | -insertion related complications-central venous stenosis-catheter related septicemia, exit site and tunnel infection-thrombosis-catheter malfunction | -thrombosis-limb oedema / venous hypertension-aneurysm / pseudoaneurysm-conduit stenosis -infection-vascular steal phenomenon-high output cardiac failure | -thrombosis-infection-conduit stenosis-aneurysm |
In our study of 50 cases, 38% patients had diabetes as a cause of ESRD similar to a recent study from India [1]. The usage of temporary catheters for initiation of HD in our series was very high (96%), when compared to other studies where it has varied from 15 to 60% [4–7]. Late presentation, delayed diagnosis, and late referral leads to unplanned dialysis initiation and hence insertion of acute HD catheters in these patients. Even if CKD was diagnosed earlier, very few agree for AVF creation. For patients, vascular access is more than a mere surgical procedure. Vascular access creation signifies kidney failure and imminent dialysis, which is emotionally confronting for the patients. Right internal jugular vein was most commonly used as per K/DOQI guidelines [2]. Subclavian catheter was avoided in our patients as it was frequently associated with stenosis which precludes creation of AVF in the limb [2].
K/DOQI guidelines suggest that incidence of catheter related bacteraemia should be less than 10% at 3 months [2]. The incidence of catheter related sepsis was high (34.48%) in our patients during the study period probably due to poor hygiene, poor socioeconomic status and prolonged dependence on catheters. The reasons for catheter removal in our patients were elective removal after successful AVF cannulation (50%), catheter related sepsis (CRS) (20.83 %), thrombosis (6.25%) and others (22.91%). Jeffery et al., and Altaee KA et al., reported similar catheter outcomes with most of the catheters removed after AVF maturation [8,9]. Mean catheter survival was 77.23 ± 14.8 days in our study. This, in contrast to 35 days reported by Altaee KA et al., indicates prolonged catheter dependence in our patients [9]. Late presentation and delayed diagnosis has lead to dialysis initiation through catheters followed by AVF creation necessitating prolonged catheter use and its associated complications.
The most common site of AVF in our series was distal radio cephalic fistula, described initially in 1966 by Brescia, et al., [10]. High radio cephalic (mid forearm), brachio-cephalic and brachial-basilic AVFs were reserved for patients with previously failed distal AVF. This is line with K/DOQI guidelines to preserve proximal veseels for future use [2].
The overall incidence of primary failure of AVFs was 23.9%, which is similar to other published series (15-30%) [1,11,12]. Three risk factors were identified: diabetes, old age (>60 years) and distal site of creation of AVF. A Bahadi et al., found distal site of AVF and diabetes to be associated with high rates of primary failure [13]. This is due to smaller caliber of distal vessels and damage to the vessel wall due to frequent venipunctures. Diabetes is associated with endothelial dysfunction, increased oxidative stress, and high prevalence of peripheral arterial disease, which may explain the increased incidence of thrombotic events [13]. The K/DOQI (Kidney Disease Outcome Quality Initiative) Work Group did not recommend to monitor primary failure rates of fistula as it may discourage attempts at AVF construction in patients with complex vascular anatomy [2].
Due to poor socioeconomic status and poor follow up, fistula salvage by embolectomy and radiological intervention was not attempted in our patients. Instead new AVF were created in such situations. Arteriovenous grafts were not done in our patients due to high costs of such grafts. The mean time to first cannulation of native AVF was 46.65±2.55 days in our study similar other reports which varies between 25 and 98 days respectively [9,14]. Fewer patients (26.31%) starting dialysis with a CVC failed transition to permanent access within 90 days compared to 59.4% reported by Wasse H et al., [15]. Older patients (>60 years) were more likely to remain CVC dependent at 90 days compared with those younger than 60 years.
Conclusion
Most patients initiate HD through catheters which with its complications lead to avoidable morbidity, mortality and huge heath care burden. Many patients consider vascular access as an agonizing reminder of their disease disrupting their identity and daily living. Counseling and early AVF creation in predialysis stage may avoid unnecessary dialysis catheter insertion and leads to better outcomes in haemodialysis patients.