Pseudoepitheliomatous, Keratotic and Micaceous Balanitis: A Case Report
Shashikant Malkud1, Veeresh Dyavannanavar2
1 Senior Resident, Department of Dermatology, Venereology & Leprosy, ESIC Medical College, Gulbarga, Karnataka, India.
2 Assistant Professor, Department of Dermatology, Venereology & Leprosy, ESIC Medical College, Gulbarga, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shashikant Malkud, Senior Resident, Department of Dermatology, Venereology & Leprosy, ESIC Medical College, Gulbarga - 585106, Karnataka, India. E-mail : smalkud@yahoo.com
Pseudoepitheliomatous, keratotic and micaceous balanitis (KPMB) is a rare condition affecting glans penis of elderly men. It is characterized by thick hyperkeratotic plaque with micaceous scaling often leading to phimosis. Here we are reporting a rare case of pseudoepitheliomatous, keratotic, and micaceous balanitis in 50-year-old man who has undergone circumcision 16 years back. Till date only a handful cases have been reported in world literature.
Glans penis, Hyperkeratotic, Verrucous
Case Report
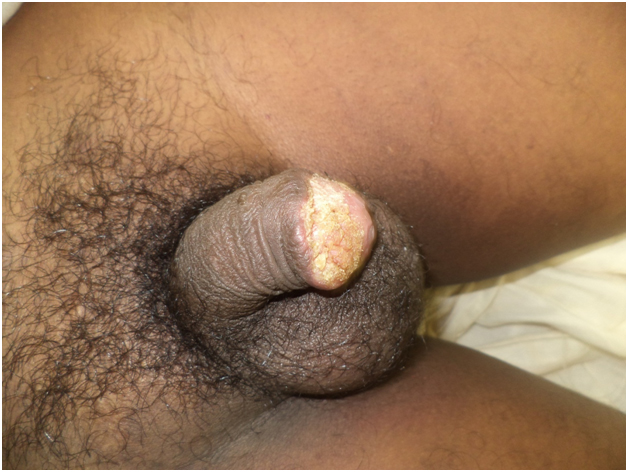
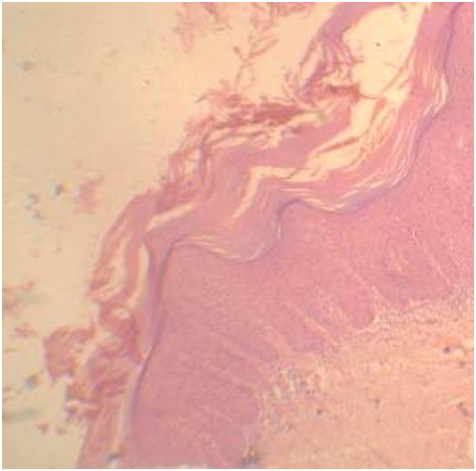
A 50-year-old male patient presented with a complaint of scaly lesion over glans penis since 4 years duration. It was initially small in size and gradually progressed to attain present size. It was not associated with itching or burning sensation. Patient was non-diabetic and there was no history suggestive of sexually transmitted infections. There was no history of bleeding either spontaneously or following minor trauma. Patient had undergone circumcision 16 years back for phimosis. Clinical examination revealed 4 X 3 cm thick hyperkeratotic plaque with adherent micaceous scales seen over dorsal aspect of glans penis extending into coronal sulcus [Table/Fig-1]. On blood investigations, complete blood counts and blood glucose level were within normal limit. Serological tests for human immunodeficiency virus, hepatitis B and syphilis were negative. Incisional biopsy was performed under local anesthesia, which on histopathology revealed pseudoepitheliomatous hyperplasia, acanthosis, elongation of rete ridges, and nonspecific dermal inflammatory cell infiltrates consisting mainly of lymphocytes with few eosinophils [Table/Fig-2]. There was no cytological atypia, koilocytes or evidence of malignancy. Diagnosis of PKMB was made based on clinical and histopathological features. Patient was started on daily topical 5-flurouracil. Patient discontinued treatment 5 days after initiating therapy.
Thick hyperkeratotic plaque on glans penis
Histopathology section showing hyperkeratosis, parakeratosis, acanthosis, elongation of rete ridges and nonspecific inflammatory infiltrates in the dermis
Discussion
Pseudoepitheliomatous, keratotic and micaceous balanitis was first described by Lortat-Jacob and Civatte in 1961 in French literature [1]. It is a rare, acquired penile disorder affecting glans penis of elderly men which is characterized by thick hyperkeratotic plaque with micaceous scaling often leading to phimosis [2]. Most patients are over the age of 60 and frequently have been circumcised for phimosis in adult life [3]. It is often asymptomatic but may be associated with irritation or burning sensation [4].
It is thought to be a form of pyodermatitis or pseudoepitheliomatous response to infection whose exact aetiopathogenesis is not known [1]. The pathogenesis of PKMB occurs in four stages: a) initial plaque stage; b) late tumour stage; c) verrucous carcinoma; and d) transformation to squamous cell carcinoma [3]. It shows considerable overlap with verrucous carcinoma though being an integral part [4]. Reports have shown its progression to invasive squamous cell carcinoma in few cases [5]. To best of our knowledge, till date only less than 10 cases have been reported from Indian subcontinent. [1–4,6–8].
There is a well-known association between PKMB and circumcision. Our patient developed PKMB after 16 years of circumcision. In most of the uncircumcised elderly patients circumcision is indicated when phimosis supervenes [9], but many developed PKMB after circumcision which was carried out in later life [10]. So, whether circumcision is the cause or effect of PKMB needs to be clarified.
Classical histopathological examination reveals hyperkeratosis, parakeratosis, acanthosis, and elongated rete ridges and mild lower epidermal dysplasia, with non-specific dermal inflammatory infiltrates of eosinophils and lymphocytes [11]. PKMB shows considerable overlap with verrucous carcinoma though being an integral part [12,13]. Some authors considered it as a variant of lichen sclerosus [14]. Reports have shown its progression to invasive squamous cell carcinoma in few cases [5,15]. Long term follow-up is needed for early detection of malignant transformation.
The treatment of PKMB should be conservative, if there is no cytological atypia, which includes topical 5-flurouracil, cryotherapy or electrocoagulation. A case reported in India was treated completely with 5-flurouracil for 3 weeks and no recurrence was noted after 10 months of follow up [2]. Surgical excision is the treatment of choice if there is any evidence of malignancy [1].
Conclusion
Pseudoepitheliomatous, keratotic, and micaceous balanitis is a rare, non-venereal penile disorder. Only few cases have been reported from Indian subcontinent. Long term follow-up is needed for early detection of malignant transformation.
[1]. Murthy P S, Kanak K, Raveendra L, Reddy P, Pseudoepitheliomatous, keratotic, and micaceous balanitisIndian J Dermatol 2010 55:190-91. [Google Scholar]
[2]. Hanumaiah B, Mohan Lingaiah NB, Kumaraswamy SK, Vijaya B, Pseudoepitheliomatous keratotic and micaceous balanitis: A rare condition successfully treated with topical 5-fluorouracilIndian J Dermatol 2013 58:492 [Google Scholar]
[3]. Sardesai VR, Agarwal TD, Dalal AB, Mhatre MA, Pseudoepitheliomatous keratotic and micaceous balanitis with malignant transformationIndian J Sex Transm Dis 2013 34:38-40. [Google Scholar]
[4]. Adya KA, Palit A, Inamadar AC, Pseudoepitheliomatous keratotic and micaceous balanitisIndian J Sex Transm Dis 2013 34:123-25. [Google Scholar]
[5]. Bart RS, Kopf AW, On a dilemma of penile horns: Pseudoepitheliomatous, hyperkeratotic and micaceousbalanitis?J Dermatol Surg Oncol 1997 3:580-82. [Google Scholar]
[6]. Das S, Ghoshal L, Pseudoepitheliomatous keratotic and micaceous balanitis of CivatteIndian Dermatol Online J 2014 5:148-50. [Google Scholar]
[7]. Pai VV, Hanumanthayya K, Naveen KN, Rao R, Dinesh U, Pseudoepitheliomatous, keratotic, and micaceous balanitis presenting as cutaneous horn in an adult maleIndian J Dermatol Venereol Leprol 2010 76:547-49. [Google Scholar]
[8]. Zawar V, Kirloskar M, Chuh A, ‘Watering-can penis’ in pseudoepitheliomatous, keratotic and micaceous balanitisActa Derm Venereol 2004 84:329-30. [Google Scholar]
[9]. Edwards , Balanitis and balanoposthitis: a reviewGenitourin Med 1996 72:155-59. [Google Scholar]
[10]. Sandra SI, Edward A, Pseudoepitheliomatous, keratotic and micaceous balanitisArch Dermatol 1981 117:435-37. [Google Scholar]
[11]. Bunker CB, Neill SM, The Genital, Perianal and Umbilical Regions. In: Burns T, Breathnach S, Cox N, Griffiths C, editorsRook’s text book of dermatology 2010 8th ednOxfordBlackwell Publishing:71.37-71.38. [Google Scholar]
[12]. Beljaards RC, van Dijk E, Hausman R, Is pseudoepitheliomatous, micaceous and keratotic balanitis synonymous with verrucous carcinoma?Br J Dermatol 1987 117:641-46. [Google Scholar]
[13]. Jenkins D, Jakubovic HR, Pseudoepitheliomatous, keratotic and micaceous balanitis. a clinical lesion with two histologic subsets: hyperplastic dystrophy and verrucous carcinomaJ Am Acad Dermatol 1998 18:419-22. [Google Scholar]
[14]. Ridley CM, Lichen sclerosusetatrophicusBr Med J (Clin Res Ed) 1987 295:1295-96. [Google Scholar]
[15]. Perry D, Lynch PJ, Fazel N, Pseudoepitheliomatous, keratotic, and micaceous balanitis: case report and review of the literatureDermatol Nurs 2008 20:117-20. [Google Scholar]