We report a rare case of bilateral broad ligament haematoma in twin pregnancy presented as gravida 3 para 2 living 2 (G3P2A0L2), with undelivered second twin with transverse lie with cord and hand prolapse with obstructed labour referred to our hospital from primary health centre after spontaneous vaginal delivery of first live healthy twin baby four hours later. On examination patient was stable, her investigations were within normal limits and patient was taken up for emergency lower segment caesarian section. Intraoperatively features of obstructed labour were present; a dead term baby was extracted with dichorionic diamniotic placenta. Bilateral broad ligament haematomas approximately of 8x8 cm were noted which were increasing in size after extraction of baby. On both sides haematomas were evacuated and drained along with bilateral uterine artery ligation. Three pints of blood were transfused intra and postoperatively. Her postoperative period was uneventful and the patient was discharged on postoperative day 14.
Hysterectomy, Retroperitoneal haematoma, Uterine artery ligation
Case Report
A 30-year-old, third gravida (G3P2A0L2), with undelivered second twin with transverse lie was referred to our hospital from primary health centre after spontaneous vaginal delivery of first live healthy twin baby four hours later. She had experienced normal spontaneous vaginal deliveries for her first two singleton pregnancies and birth weight ranged from 2.5 to 3 kg and had no antepartum, intrapartum or postpartum complications and had undergone no uterine surgeries in her past.
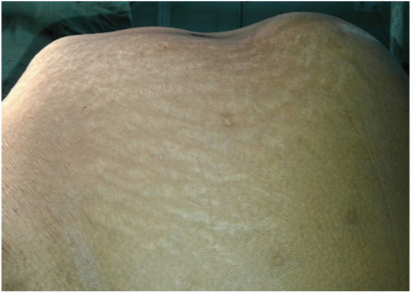
On examination patient was conscious, pulse was 92 bpm and her BP was 110/70 mm of Hg. On inspection her bladder was distended, She had a “three-tumour abdomen’” an oedematous distended bladder, a distended, tender lower segment, and a tonically contracted upper segment [Table/Fig-1]. A ring (Bandl’s ring) could be felt through her abdominal wall between her upper and lower segments. The uterus was enlarged to the size of a full-term pregnancy with transverse lie with signs of obstruction. Foetal heart sound was absent
Abdominal examination showing signs of obstructed labour-“three-tumour abdomen” an oedematous distended bladder, a distended, tender lower segment, and a tonically contracted upper segment
On local examination clamped umbilical cord of delivered first twin along with left hand and umbilical cord prolapse without pulsations of second twin were seen outside the vulva [Table/Fig-2]. On per vaginal examination cervix was fully dilated with the left shoulder at 0 station with hand and cord prolapse. Catheterizing her was difficult, blood-stained urine drained after catheterization. Her investigations were within normal limits. A coagulation screen prothrombin time (PT), activated partial thromboplastin time (APTT), INR were done to exclude bleeding disorders. All her investigations were within normal limits and patient was taken up for emergency lower segment caeserian section in view of obstructed labour.
Left hand prolapse with cord prolapse of second twin and clamped cord of first twin

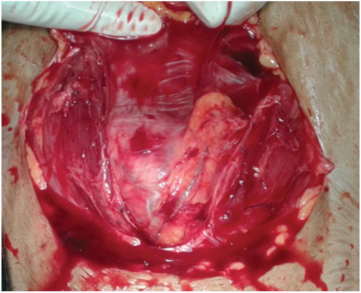
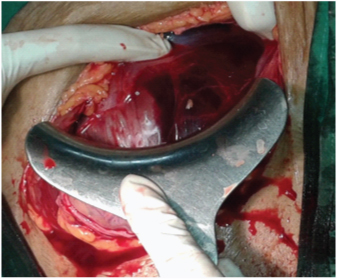
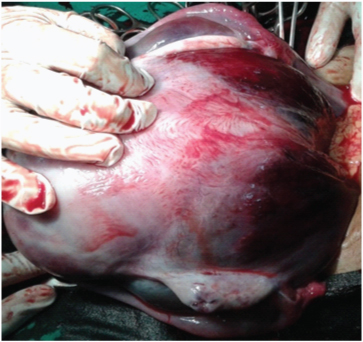
Intraoperatively bladder was edematous and pulled up [Table/Fig-3], after separating uterovesical fold of peritoneum bladder was pushed down [Table/Fig-4]. Lower uterine segment was stretched out. Khers incision was given on lower uterine segment and a dead term female baby of weight 2.4kg was extracted as breech. Placenta was dichorionic diamniotic. No uterine malformations were there. Bilateral broad ligament haematomas approximately of 8x8 cm were noted which were increasing in size after extraction of baby [Table/Fig-5,6], on both sides haematomas were evacuated and drained along with bilateral uterine artery ligation was done. A drain was kept in pouch of douglas and abdomen was closed in layers. One unit of whole blood was transfused intraoperatively and two unit of whole blood was transfused postoperatively. She was monitored in ICU (intensive care unit) for 72 hours. Monitoring patient’s pulse, blood pressure, temperature, respiratory rate, oxygen saturation and urine output (Foley’s catheter) every 4 hours for the first 48 hours, then every 6 hours afterwards. Intravenous prophylactic antibiotics (ceftriaxone 1gm BD, metronidazole 500 mg TDS) were prescribed for 7 days. An ultrasound scan was done on her third postoperative day showed full resolution of broad ligament haematoma [Table/Fig-7]. Foley’s catheter was retained in bladder for 14 days to prevent fistula because of avascular necrosis. The woman recovered well and was discharged home 14 days later. At discharge, a repeat scan confirmed no recurrence of the haematoma.
Bladder edematous and pulled up
Left broad ligament and uterine haematoma after separating uterovesical fold of peritoneum before extraction of baby
Bilateral broad ligament hematoma by exteriorization of the uterus anterior aspect
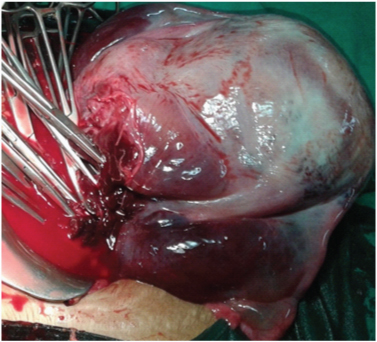
Bilateral broad ligament hematoma by exteriorization of the uterus posterior aspect
Postoperative day 3 abdomino pelvic scan showed involuting uterus, full resolution of broad ligament haematoma

Discussion
Bilateral broad ligament haematoma are rare complication after vaginal delivery of a first twin in twin pregnancy, which is a life threatening situation if unrecognized and managed early. Whitridge Williams’ reported series of cases in a monograph on subperitoneal haematomat. He found 33 cases of spontaneous broad ligament haematomas and ascribed them to capillary bleeding, he was the first person to report broad ligament haematomas in 1904 [1].
The incidence is 1:20,000-1:3500 [2]. Formation of broad ligament haematomas and retroperitoneal haematomas are due to lacerations of the uterine artery or vein or a tear in the upper vagina, cervix or uterus that extends into uterine or vaginal arteries, which has a higher rate of morbidity and mortality and a rare event in obstetrical practice.
About a third of broad ligament haematomas follows spontaneous vaginal delivery, caesarean section, precipitate labour and forceps delivery, breech delivery, delivery of multiples, prolonged second stage labour, birth weight above 4,000 g, hereditary clotting defi-ciencies and pre-eclampsia [3]. Fifty percent of these are recognised immediately while other fifty percent are discovered after about 24 hours. Rapidly expanding haematomas are of arterial origin and appear bright or dark red, slow expanding haematomas are of venous origin and appear dark red or bluish in colour. It may be silent with no obvious vaginal bleeding [3].
The symptomatology of the haematomas depends upon the size and rate of formation and type of haematoma. Haematomas are usually diagnosed when patient presents with haemorrhagic shock or even death, due to its insidious nature [4].
Patients may present with persistent postpartum pelvic pain, back pain, fullness or pressure in the recto-anal area, or an urge to push within the first few hours after delivery, headache, dizziness and become hypotensive, with a sudden fall in haematocrit value [5].
Symptoms can be quite vague. The diagnosis can be confirmed by USG. Patients with persistent postpartum localized pelvic pain without clinical findings, MRI should be done to evaluate such type of patients [6].
Key steps in treating broad ligament haematoma are resuscitation, volume replacement and surgical exploration. Broad ligament haematomas are managed conservatively with close observation or surgical exploration under regional or general anaesthesia depending on their behaviour, small non spreading broad ligament haematomas are self-limiting, if they appears to be expanding, direct pressure is applied to the site and observed for any further expansion. If haematomas are expanding still, uterine and/or ovarian artery ligation should be done.
Hysterectomy [7], internal iliac artery ligation, angiographic embolization [8] have been proposed as surgical options depending upon patients’ circumstances and their clinical presentation. Algorithm of Bienstman-Pailleux et al, Pelvic arterial embolization is safe only in haemodynamically stable patients and embolization unit should be close to delivery room [9–11].
Broad ligament haematomas were reported after 24 hours after spontaneous vaginal delivery which was managed conservatively [12], after snake bite [5], after road traffic accident in pregnancy which was managed surgically [13], after caeserian section, our case is very rare, accidental finding of bilateral broad ligament haematoma intraoperatively in twin pregnancy after vaginal delivery of first twin, second twin with transverse lie with obstructed labour, which was managed by evacuation and bilateral uterine artery ligation. In haemodynamically stable patients and with no congenital or acquired bleeding tendency, broad ligament haematomas are conservatively managed.
Conclusion
Bilateral broad ligament haematomas are rare complication after vaginal delivery of first twin in twin pregnancy and it’s a life threatening situation. Clinical symptoms can be quite vague. Broad ligament haematomas are self-limiting, if the haematoma appears to be expanding, evacuation is done. If expansion of the haematoma persists, uterine and/or ovarian artery ligation is done. In our case bilateral broad ligament haematomas were managed by evacuation and bilateral uterine artery ligation. Hysterectomy, internal iliac artery ligation or angiographic embolization has been proposed as surgical options depending upon patients’ circumstances and their clinical presentation.
[1]. Williams JW, Trans. Amer. Gynec Soc 1904 29:186 [Google Scholar]
[2]. Saleem N, Ali HS, Irfan A, Afzal B, Broad ligament haematoma following a vaginal delivery in primigravidaPak J Med Sci 2009 25:683-85. [Google Scholar]
[3]. Edmonds Dewhurst’s Textbook of Obstetrics & Gynecology6th ednLondonBlackwell Science [Google Scholar]
[4]. Park M, Han SS, A case of secondary postpartum haemorrhage with shock followed by rupture of progressive retroperitoneal haematoma through left upper vaginal wallKorean J Obstet Gynecol 2011 54:314-16. [Google Scholar]
[5]. Addo V, Kokroe FA, Reindorf RL, Broad ligament haematoma following a Snake BiteGhana Med J 2009 43:181-82. [Google Scholar]
[6]. Jain KA, Olcott EW, Magnetic resonance imaging of postpartum pelvic haematomas: early experience in diagnosis and treatment planningMagn Reson Imaging 1999 17:973-77. [Google Scholar]
[7]. Maxwell C, Gawler D, Green J, An unusual case of acute postpartum broad ligament haematomaAustralia NZ J Obstetrics & Gynecology 1997 37:239-41. [Google Scholar]
[8]. Muthulakshmi B, Francis I, Magos A, Roy M, Watkinson A, Broad ligament haematoma after a normal deliveryJournal of Obstetrics & Gynecology 2003 23:669-70. [Google Scholar]
[9]. Bienstman-Pailleux J, Huissoud C, Dubernard G, Rudigoz RC, Management of puerperal haematomasJ Gynecol Obstet Biol Reprod (Paris) 2009 38:203-08. [Google Scholar]
[10]. Doumouchtsis SK, Papageorghiou AT, Arulkumaran S, Systematic review of conservative management of postpartum haemorrhage: what to do when medical treatment failsObstet Gynecol Surv 2007 62:540-47. [Google Scholar]
[11]. Sentilhes L, Gromez A, Clavier E, Resch B, Verspyck E, Marpeau L, Predictors of failed pelvic arterial embolization for severe postpartum haemorrhageObstet Gynecol 2009 113:992-99. [Google Scholar]
[12]. Murali A Rare Case of Broad Ligament Haematoma 24 Hours after Normal Vaginal DeliveryJ Clin Case Rep 2014 4:7 [Google Scholar]
[13]. Koffi Damage to the Right Rectus Abdominus Muscle and Haematoma of the Right Uterine Broad Ligament: Rare Complications of a Road Accident during PregnancyClinics Mother Child Health 2013 11:1 [Google Scholar]