Trichinella spiralis: Mere Co-Existence or Carcinogenic Parasite For Oral Squamous Cell Carcinoma?
Nadia Shirazi1, Sampan Singh Bist2, Sohaib Ahmad3, Meena Harsh4
1 Associate Professor, Department of Pathology, Himalayan Institue of Medical Sciences, Jolly Grant, Dehradun, Uttarakhand, India.
2 Professor, Department of Ear, Nose and Throat, Himalayan Institue of Medical Sciences, Jolly Grant, Dehradun, Uttarakhand, India.
3 Professor, Department of Medicine, Himalayan Institue of Medical Sciences, Jolly Grant, Dehradun, Uttarakhand, India.
4 Professor, Department of Pathology, Himalayan Institue of Medical Sciences, Jolly Grant, Dehradun, Uttarakhand, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Nadia Shirazi, B-IX-6, HIHT Campus, Swami Rama Himalayan University, Jolly Grant, P.O. Doiwala, Dehradun, Uttarakhand-248140, India.
E-mail: shirazinadia@gmail.com
Trichinella spiralis is a parasite which is usually seen in pork-eaters. Most of the trichinosis infections cause little or no symptoms. We report a rare case of a middle aged North Indian male who presented with a painless ulcer in right buccal mucosa which was biopsied and reported as squamous cell carcinoma. Wide local excision was done subsequently which showed encysted larvae of Trichinella spiralis in the deeper skeletal muscle bundles. This article supports the carcinogenic potential of trichinosis and suggests timely work-up and treatment of the parasite.
Buccal mucosa, Nematode, Trichinosis
Case Report
A 37-year-old male presented to the Otolaryngology (ENT) OPD with a painless, progressive non healing ulcer on right buccal mucosa since 2 months. He gave a dietary history of pork meat intake since many years. He consumed alcohol off and on but was not a tobacco/gutka chewer. There were no co-morbidities and he was immunocompetent. He could open his mouth completely and there were no episodes of repeated mouth ulcers. On examination, the ulcer was 1.5x1.0 cm in size with irregular heaped up margins and necrotic floor [Table/Fig-1]. A punch biopsy was taken and sent for histopathological examination (HPE) which was reported as well differentiated keratinizing squamous cell carcinoma [Table/Fig-2]. The surgeon planned a wide local excision of the residual ulcer and sent it again for HPE. A complete haemogram ordered prior to surgery showed mild to moderate eosinophilia with absolute eosinophil count (AEC) of 600/mm3.

H&E: 20x10X: Sheets of nests of well differentiated squamous cell carcinoma

On gross examination, a mucosa covered tissue piece was received measuring 3x2x1.8cm. The central part showed an ulcerated area measuring 1.5x1x0.2cm. On serial slicing through the ulcer no definite growth was seen however multiple sections were taken from ulcer including margins and the tissue was submitted entirely for processing.
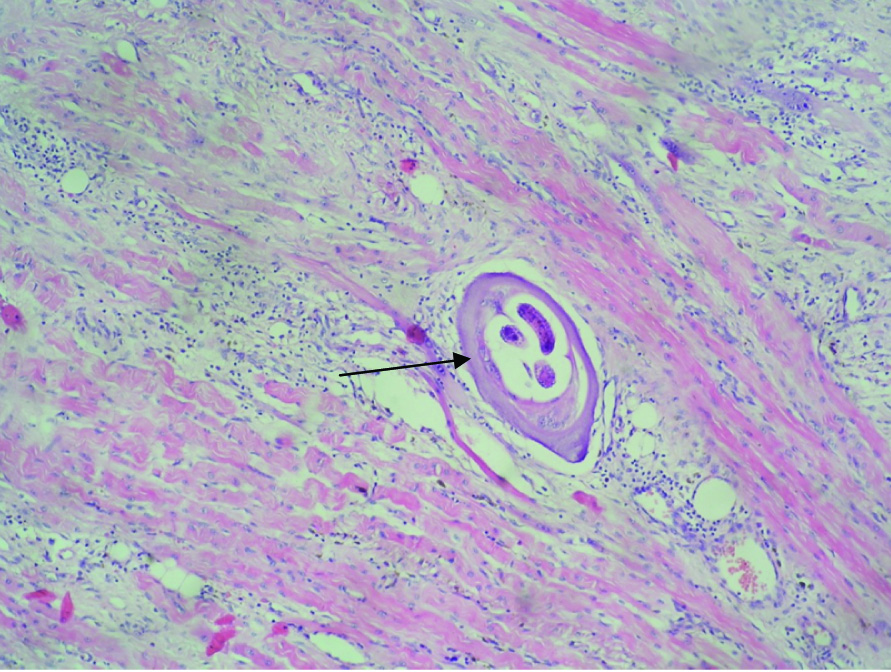
On microscopic examination, sections showed mucosa covered tissue piece with central area of ulceration. The ulcer was covered with fibrinoid necrosis and neutrophilic exudate. Just beneath the ulcer, dense lymphoplasmacytic infiltrate was seen with fair number of eosinophils. Skeletal muscle bundles showed larvae of Trichinella spiralis which were encysted or enclosed in a capsule [Table/Fig-3]. There was no residual viable malignant tumour in this specimen indicating the tumour was small in size and may have been removed during biopsy.
H&E: 20X 10X: Larva of Trichinella spiralis in deeper skeletal muscle bundles of buccal cavity
The patient was discharged after administering the anti-helminthic Mebendazole 400 mg thrice a day for 10 days and supportive medications and is being followed up regularly without any complaints.
Discussion
Trichinella infection has been reported in association with endometriosis, non union of fractures as well as carcinomas of oral cavity and breast [1–4]. Trichinosis in man usually follows consumption of raw or undercooked pork contaminated with infective larvae or adult nematode Trichinella spiralis. Recently, an outbreak of acute trichinellosis was reported in 54 patients from this region of north India [5]. There are two main phases for the infection: enteral (affecting intestines) and parenteral (outside intestines) [6]. The symptoms depend on the phase, species of Trichinella, amount of encysted larvae ingested, age, gender and host immunity. Most cases run a subclinical course. Local symptoms are seen in intestinal tract in the first week following ingestion of pork and result in diarrhea, vomiting or nausea. Systemic or parenteral manifestations of the disease are myositis, swelling, fever, pain and weakness. The worm has a predilection for the oxygenated skeletal muscles [6]. Typical worm is seen coiled in a cyst wall derived from the host cells with surrounding lymphocytic and eosinophilic infiltrate. Serological tests may be used to substantiate the infection in doubtful cases; the characteristic appearance in biopsy sample is diagnostic.
The pronounced eosinophilia observed in trichinellosis may be attributed to interleukin-5, produced by the Th2 subset of CD4+ T cells. Eosinophils are cytotoxic for newborn larvae in human antibody dependent cellular cytotoxicity (ADCC) “invitro” reactions, by releasing the major basic protein, peroxidase or reactive oxygen species; their actual role “invivo” is not clear [7].
Presence of trichinosis can merely be a co-existence of infestation in tumour tissue as discussed by Jozo Kristek [8]. Moisan PG also concluded that there was no evidence to support that trichinella was the cause of malignancy [9]. Whether or not it is a carcinogenic factor is a matter of speculation, however, constant irritation by the very presence of the organism may be responsible for the development of the malignancy. It is postulated that trichinella upregulates Vascular Endothelial Growth Factor (VEGF) and modifies external kinases as well as nucleotide metabolizing enzymes [10,11]. Each of these activities potentially modulates multiple host functions including tumour immunity. The detection of the parasite in the vicinity of the malignancy in this case and the detection of the same nematode in other case reports of head and neck [2] and breast malignancies [3] lend credibility to its carcinogenic potential and not merely a co-incidental finding.
Traditionally, people of lower socio-economic class residing in the hilly areas are pork eaters and occasionally present with trichinosis. This case from the north Indian state of Uttarakhand presented de novo with a well circumscribed malignancy bereft of the symptoms of trichinosis. This is the first case report of trichinosis with carcinoma of buccal mucosa from the Indian subcontinent and may suggest exhaustive work-up for the parasite and malignancy in pork eaters.
Conclusion
Trichinosis appears to be re-emerging as an important zoonotic infection in various parts of the world with few cases associated with malignancies of oral cavity, larynx and breast. This association strengthens the fact that control of trichinosis depends on persistent vigilance, awareness of disease, identification of parasite and early management of the disease. Immunization of swine against Trichinella spiralis may also be carried out where pork eaters are present.
[1]. Bezeya T, Odida M, Okelo J, Trichinella spiralis infestation complicating open reduction and internal fixation for closed fracture femurEast and Central African Journal of Surgery 2009 14(1):81-83. [Google Scholar]
[2]. Cheung LK, Yeung RW, Leung SY, Samman N, Trichinosis associated with carcinoma of the tongue: case reportOral Surg Oral Med Oral Pathol Oral Radiol Endod 1997 84(1):32-34. [Google Scholar]
[3]. Kristek J, Marjanovic K, Dmitrovic B, Krajinovic Z, Sakic K, Trichinella spiralis and breast carcinoma-a case reportColl Antropol 2005 29(2):775-77. [Google Scholar]
[4]. Feldemeir H, Bienzle U, Jasen-Rosseck R, Kremsner PG, Wieland H, Dobos G, Sequelae after infection with Trichinella spiralis: A prospective cohort studyWien Klin Woschensch 1991 103(4):111-16. [Google Scholar]
[5]. Weller PF, Trichinella and other tissue nematodes. In: Fauci 2. AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, et al, editorsHarrison’s principles of internal medicine 2012 18th edNew YorkThe McGraw-Hill Company:1735-38. [Google Scholar]
[6]. Sharma RK, Raghavendra N, Mohanty S, Tripathi BK, Gupta B, Goel A, Clinical & biochemical profile of trichinellosis outbreak in north IndiaIndian J Med Res 2014 140:414-19. [Google Scholar]
[7]. Bruschi F, Murrell KD, New aspects of human trichinellosis: the impact of new Trichinella speciesPostgrad Med J 2002 78:15-22. [Google Scholar]
[8]. Kristek J, Trichinella spiralis and Breast Carcinoma– A Case ReportColl Antropol 2005 29(2):775-77. [Google Scholar]
[9]. Moisan PG, Lorenz MD, Stromberg PC, Simmons HA, Concurrent trichinosis and oral squamous cell carcinoma in a catJ Vet Diagn Invest 1998 10(2):199-202. [Google Scholar]
[10]. Virginia A-Capo, Dissckson DD, Ramola IP, Trichinella spiralis: Vascular Endothelial Growth Factor is upregulated within the nurse cell during the early phase of its formationJ Parasitol 1998 84(2):209-14. [Google Scholar]
[11]. Bruce RA, Trichinosis associated with oral squamous cell carcinoma: a report of 3 casesJ Oral Surg 1975 33(2):136-41. [Google Scholar]