Covering the clinically exposed root surface of a tooth has now become a routine demand of patients to improve aesthetics and also to reduce the instances of hypersensitivity. The idea behind the treatment of gingival recession is to place the gingiva as close as possible to the cement-enamel junction so that the exposed root area is covered and a normal sulcus is created. Here we present a series of two cases of gingival recession treatment in young patients affecting the maxillary anterior region. The affected sites were treated by a periodontal flap with synthetic collagen membrane and patient derived platelet rich fibrin. It may be emphasized that platelet-rich fibrin can be used as a membrane for periodontal tissue regeneration and it has the ability to promote platelet aggregation, be chemotactic for fibroblast and enhance wound stability and proper healing. Hence, both the methods can be successfully used in place of a connective tissue graft for treating gingival recession.
Coronally advanced flap, Connective tissue graft, Cosmetic surgery, Gingival recession
Case Report
Two patients, one male and one female, of age 25 and 27 years respectively, reported with a complaint of receding gingiva in the maxillary central incisors to the Department of Periodontology, Ragas Dental College, Chennai. History revealed that they were not finding their smile aesthetic and occasionally there was hypersensitivity to hot and cold food. Because of the discomfort both had stopped brushing and cleansing that area which lead to more accumulation of plaque thereby aggravating the condition. The medical, personal and family histories were non-contributory.
On examination, a detailed clinical assessment of the affected site and classification of the gingival recession as well as complete medical evaluation was carried out.
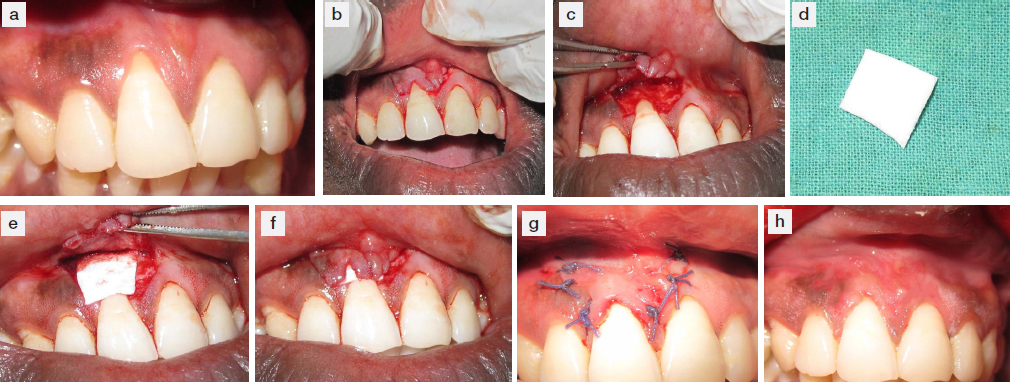
The clinical probing depth (PD) was 2 mm with no associated bleeding on probing. The clinical attachment level (CAL) was 4 mm from the cemento enamel junction. Width of the keratinized gingiva (KG) was 2 mm. In this case the root coverage was planned using collagen membrane [Table/Fig-1a].
(a) Intra-oral picture of the patient presenting with gingival recession buccally in relation to 11 (b) Horizontal incisions were given parallel to the cemento-enamel junction followed by vertical incisions beyond the muco-gingival fold (c) Flap was raised using a combination of full thickness and partial thickness in the apical portion to mobilize the flap towards coronal portion of tooth (d) The collagen membrane was resized properly to cover the recession area mesially, distally and apically (e) The trimmed collagen membrane is placed under the raised flap (f) The flap was coronally advanced covering the collagen membrane and secured at a position 2mm beyond the cemento-enamel junction (g) The flap is sutured at a coronal position (h) Clinically stable condition after 6 months with adequate root coverage
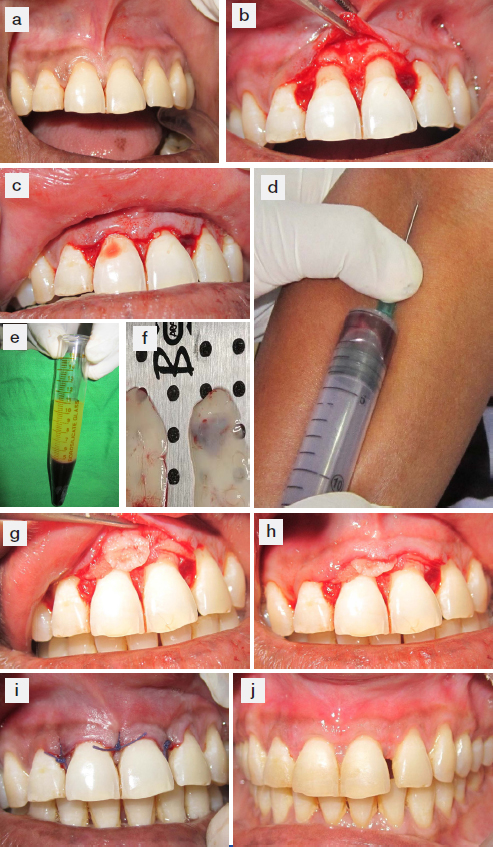
The PD was of 2 mm with no associated bleeding on probing. The CAL was 5 mm from the cement enamel junction. Width of keratinized gingiva (KG) was 3 mm. In this case root coverage was planned using platelet rich fibrin (PRF) derived from patients’ blood [Table/Fig-2a].
(a) Intra-oral picture of the patient presenting with gingival recession in relation to upper central incisors (b) Horizontal incisions made parallel to cemento-enamel junction with preservation of the interdental papillae (c) Adequate mobility of the flap was achieved to place it coronally 2mm below the cement-enamel junction without stretching (d) Collection of venous blood from the patient (e) Centrifuged blood showing the 3 layers: upper straw-coloured acellular plasma, central fibrin clot and the lower red-coloured cellular elements (f) Prepared platelet rich fibrin membrane derived from the blood (g) Platelet rich fibrin was pushed under the raised flap (h) Platelet rich fibrin was positioned 2mm coronal the cement-enamel junction (i) Coronally advanced flap sutured with the interdental papillae using interrupted sutures (j) Clinically stable condition after 6 months with complete root coverage
Both the patients were informed in detail about the surgical procedure and patient consent was obtained.
Treatment
One hour prior to the periodontal surgery ibuprofen 600 mg was administered. In order to achieve proper local anaesthesia and haemostasis 4% articaine with epinephrine at 1:200,000 infiltrations were used. Following the administration of local anaesthesia the exposed portion of the root was conditioned. This was done with the help of ultrasonic devices and application of fresh tetracycline solution on the exposed root surface (125 mg tetracycline/mL saline). This conditioning removes the smear layer from the root surface, provides antibiotic coating, inhibits collagenase and promotes the formation of type I collagen. After conditioning, root surfaces are washed with normal saline and air-dried.
Case 1
After adequate anaesthesia two horizontal incisions were made on both sides parallel to the cemento-enamel junction of the tooth to be treated with a no. 15C blade, creating a well-defined butt joint margin. In this way we were able to preserve the interdental papillae for a better outcome. Vertical releasing incisions were made on the mesial and the distal aspects at the surgical site (at the terminal ends of the horizontal incisions) and placed at the line angles of adjacent teeth. These releasing incisions were extended beyond the mucogingival junction for the flap to be mobile. An intrasulcular incision around the affected tooth was made that connected the two vertical incisions coronally with the horizontal incisions [Table/Fig-1b].
A full-thickness flap was raised using a periosteal elevator (24G) (Hu-Friedy) which enabled bone visibility 3 mm apical to the exposed root. The flap was then converted to a partial thickness apically that will enable coronal mobilization [Table/Fig-1c]. When moved coronally was now able to cover and lie passively on the recession area without any tension. This is critical because any tension while suturing will affect the positive outcome of the procedure. The collagen membrane [Table/Fig-1d] was trimmed to cover the recession area properly [Table/Fig-1e]. The membrane was adjusted in such a way that it extended 2 mm beyond the borders of the recession mesially, distally and apically. The membrane was placed coronally at the level of CEJ and was secured [Table/Fig-1f]. Once the membrane is stabilized, then the buccal flap is moved coronally and secured to the papillae with interrupted suture using 5-0 absorbable sutures [Table/Fig-1g]. In order to prevent the exposure of the membrane and also to counter for the postoperative shrinkage the buccal flap is usually placed around 1 to 2 mm beyond the cemento enamel junction. A periodontal dressing was then placed on the surgical site and left for a week. Both the collagen membrane and the suture materials used were absorbable which eliminated the chances of interference with the healing zone during suture removal.
Case 2
In this case there was 2 mm of recession on both central incisors in the maxillary arch [Table/Fig-2a]. Adequate presurgical anaesthesia was achieved. Root conditioning was also done using tetracycline solution as done in the 1st case. Horizontal incisions were given parallel to CEJ covering the affected central incisors and extending to the lateral incisors on both sides. This resulted in a butt joint preserving the interdental papillae. Then flap was raised using a periosteal elevator (24G) (Hu-Friedy) [Table/Fig-2b]. The fibres under the flap were undermined using 15 C blade. This was done to make the flap mobile. Care was taken not to tear or puncture the flap. Adequate mobility was achieved so that the flap can be placed coronally [Table/Fig-2c].
Preparation of PRF: 5 ml of whole venous blood was collected from the patient [Table/Fig-2d] in two sterile vaccutainer tubes (6ml) and placed in centrifugal machine set at a speed of 3000 revolutions per minute. After this the blood settled in 3 layers - Upper straw-coloured acellular plasma, red-coloured lower fraction containing red blood cells (RBCs), and the middle fraction containing the fibrin clot [Table/Fig-2e]. The straw coloured layer was discarded. The middle fraction was collected and the bottom red coloured fraction with RBCs was also discarded. The collected PRF was compressed to make a PRF membrane [Table/Fig-2f].
The PRF membrane was then pushed under the raised flap. The PRF membrane was adjusted so that it can cover the recession area [Table/Fig-2g]. The interdental papilla was de-epithelialized. The PRF membrane was placed 1 to 2 mm coronally to CEJ [Table/Fig-2h]. The flap was then coronally advanced and sutured to the interdental papillae using interrupted suture with a 5-0 absorbable suture material [Table/Fig-2i]. Periodontal dressing was applied at the surgical site and left for a week.
Post Surgical Care: Both patients were prescribed oral antibiotics (Amoxycillin + Potassium Clavunate/625 mg) twice daily for 5 days and non-steroidal analgesic ibuprofen (600 mg twice daily for 5 days). They were also instructed to use chlorhexidine mouthrinse twice daily for two weeks. Patients were advised not to manipulate the surgical site. The sutures were removed in 14 days post-surgery. Both the patients were recalled after an interval of 6 months for postoperative assessment. During all the postoperative appointments the teeth involved in surgery were cleaned and polished.
Clinical Measurements: Parameters that were recorded to assess the outcome of the cases were Recession depth (REC), sulcus depth (PD), width of keratinized gingiva (KG), and Gingival Thickness (GT). Recession depth and sulcus depth were measured using William’s probe. A number 15 reamer was used to evaluate the gingival thickness. GT was measured at a point 1 mm apical to the sulcus depth. After applying topical anaesthesia the reamer was gently inserted and after hitting the alveolar bone the rubber stop was adjusted at the correct height. The reamer was carefully removed and the penetration depth measurement was taken using graduated caliper.
Starting from the day of surgery (T0) both patients were recalled after an interval of 6 months. Both the patients showed uneventful healing. On 6th month recall both the patients showed an excellent tissue healing with complete coverage of the recession area. The contour and colour had improved. All the necessary clinical parameters were recorded on the day of 6th month recall and were compared with the corresponding values recorded at the beginning of the treatment. The [Table/Fig-3,4] show relative comparisons of the recorded clinical parameters, before and after recession coverage of the case 1 and 2 respectively.
Clinical Parameters Comparison at T0 and T6 (Case 1)
| Gingival recession coverage using collagen membrane |
|---|
| Parameter | Value at T0 | Value at T6 |
|---|
| REC (mm) | 3 | 1 |
| KG (mm) | 2 | 3 |
| GT (mm) | 2 | 3 |
| CAL (mm) | 4 | 2 |
Clinical Parameters Comparison at T0 and T6 (Case 2)
| Gingival recession coverage using PRF membrane |
|---|
| Parameter | Value at T0 | Value at T6 |
|---|
| REC (mm) | 3 | 1 |
| KG (mm) | 3 | 3 |
| GT (mm) | 2 | 3 |
| CAL (mm) | 5 | 3 |
In both the patients adequate root coverage at the recession site was seen with satisfactory contour and colour.
In the first patient (case 1) as evident in the 6 month postoperative picture [Table/Fig-1h] there was a marked improvement in the colour and contour of the gingiva at the affected site. There was a reduction in the recession depth (REC) from 3 mm to 1 mm. Gingival thickness also showed an improvement from 2 mm to 3 mm. There was also a gain in the clinical attachment level of 2 mm.
In the second patient (case 2), the 6 month postoperative picture [Table/Fig-2j] showed an appreciable improvement in colour and contour. There was a reduction in the recession depth from 3 mm to 1 mm. The gingival thickness showed an increase by 1 mm. There was also a gain of 2 mm in the clinical attachment level. In both the cases there was a marked improvement in the clinical parameters as well as aesthetics at the end of 6th month.
Discussion
The coronally advanced flap together with CTG is one of the most widely used procedures to correct gingival recession. However, this method has limitations in treatment [1,2]. In such cases there is an associated morbidity at the site of CTG harvesting. It not only creates discomfort for the patient but also, many times the harvested CTG is not adequate to cover all the recession defect sites.
In the case reports presented here, two alternative treatment modalities for root coverage have been discussed in patients having Miller’s Class I Gingival recession. In one case we used commercially available collagen membrane and in second case platelet rich fibrin (PRF) derived from patient’s blood. This provides two unique advantages: First the coverage of the gingival recession sites without inducing any morbidity in the patient as there is no tissue-harvesting site and secondly, the defect sites showed a satisfactory covering thereby enhancing the aesthetics and decreasing area of recessions that can act as foci of systemic infection.
There have been prior studies to explore the use of coronally advanced flap in association with platelet concentrates and collagen membrane in the coverage of gingival recession. Sofia Aroca et al., have concluded in their study that the coronally advanced flap in association with platelet rich fibrin placed under the flap provided for a better healing and increased gingival thickness at the operative site [3,4]. Pini Prato et al., have also proposed that the use of guided tissue membrane provides much better results in terms of recession coverage and patient comfort [5]. Studies by Cardaropoli et al., Jepsen et al., and McGuire et al., have showed that the treatment of single or multiple recessions using collagen membrane resulted in good aesthetics and increased thickness of gingiva as the membrane [6–8]. Soni et al., have proposed that the use of collagen membrane in gingival recession coverage provides a better aesthetics and thicker gingival [9]. In the study by Kontovazainitis et al., gingival recession coverage was carried out using a combination of platelet rich fibrin with collagen membrane in the same patient and the results showed marked improvement in aesthetics and clinical parameters [10].
In vitro studies have demonstrated that the use of platelet rich fibrin helps is the better and faster healing of the operative site [11–13]. Platelet rich fibrin acts as a source of growth factors. Oates et al., have studied that growth factors (PDGF)-AA and PDGF-BB were major mitogens for human periodontal ligament cells, and transforming growth factor (TGF)-1 played a role as a regulator of the mitogenic responses [13]. Kawase et al., have proposed that platelet rich fibrin clot stimulates the formation of type 1 collagen in periodontal ligaments and osteoblastic cells invitro [12]. In vivo studies with the use of platelet concentrates have showed accelerated maturation of bone and periodontal ligaments. Since platelet concentrate has a higher number of platelets per milliliter, it is expected to contain a higher concentration of growth factors to accelerate or enhance regeneration [14].
In this case series, there was an attempt to make the process of root coverage less invasive by eliminating the second surgical donor site. In place of connective tissue graft, a coronally advanced flap was used using collagen membrane and platelet rich fibrin which resulted in a good aesthetic outcome with gain in clinical attachment and width of keratinized tissue.
Conclusion
The two cases presented here illustrate that the platelet rich fibrin and collagen membrane can be a more efficient and less invasive approach to treat gingival recession defects. In both the cases excellent aesthetic results were achieved in relation to colour, contour and consistency of the gingiva. Both the cases also showed similar improvement in the clinical parameters with satisfactory root coverage and increased gingival thickness.
[1]. Aroca S, Keglevich T, Nikolidakis D, Gera I, Treatment of class III multiple gingival recessions: a randomized-clinical trialJ Clin Periodontol 2010 37:88-97. [Google Scholar]
[2]. Hofmänner P, Alessandri R, Laugisch O, Aroca S, Predictability of surgical techniques used for coverage of multiple adjacent gingival recessions: a systematic reviewQuintessence Int 2012 43:545-54. [Google Scholar]
[3]. Aroca S, Molnár B, Windisch P, Gera I, Treatment of multiple adjacent Miller class I and II gingival recessions with a modified coronally advanced tunnel (MCAT) technique and a collagen matrix or palatal connective tissue graft: a randomized, controlled clinical trialJ Clin Periodontol 2013 40:713-20. [Google Scholar]
[4]. Aroca S, Keglevich T, Barbieri B, Gera I, Clinical evaluation of a modified coronally advanced flap alone or in combination with a platelet-rich fibrin membrane for the treatment of adjacent multiple gingival recessions: a 6-month studyJ Periodontol 2009 80(2):244-52. [Google Scholar]
[5]. Pini Prato GP, Tinti C, Vincenzi G, Magnani C, Guided tissue regeneration versus mucogingival surgery in the treatment of human buccal gingival recessionJ Periodontol 1992 63:919-28. [Google Scholar]
[6]. Cardaropoli D, Cardaropoli G, Healing of gingival recessions using a collagen membrane with a hemineralized xenograft: a randomized controlled clinical trialInt J Periodontics Restorative Dent 2009 29:59-67. [Google Scholar]
[7]. Jepsen K, Jepsen S, Zucchelli G, Stefanini M, Treatment of gingival recession defects with a coronally advanced flap and a xenogeneic collagen matrix: A multicenter randomized clinical trialJ Clin Periodontol 2013 40:82-89. [Google Scholar]
[8]. McGuire MK, Scheyer ET, Xenogeneic collagen matrix with coronally advanced flap compared to connective tissue with coronally advanced flap for the treatment of dehiscence-type recession defectsJ Periodontol 2010 81:1108-17. [Google Scholar]
[9]. Soni N, Sikri P, Kapoor D, Soni BW, Jain R, Evaluation of the efficacy of 100% type-I collagen membrane of bovine origin in the treatment of human gingival recession: a clinical studyIndian J Dent 2014 5(3):132-38. [Google Scholar]
[10]. Kontovazainitis G, Griffin TJ, Cheung WS, Treatment of gingival recession using platelet concentrate with a bioabsorbable membrane and coronally advanced flap: a report of two casesInt J Periodontics Restorative Dent 2008 28:301-07. [Google Scholar]
[11]. Okuda K, Kawase T, Momose M, Murata M, Platelet-rich plasma contains high levels of platelet-derived growth factor and transforming growth factorand modulates the proliferation of periodontally related cells InvitroJ Periodontol 2003 74:849-57. [Google Scholar]
[12]. Kawase T, Okuda K, Wolff LF, Yoshie H, Platelet-rich plasma-derived fibrin clot formation stimulates collagen synthesis in periodontal ligament and osteoblastic cells InvitroJ Periodontol 2003 74:858-64. [Google Scholar]
[13]. Oates TW, Kose KN, Xie JF, Graves DT, Receptor binding of PDGF-AA and PDGF-BB, and the modulation of PDGF receptors by TGF-beta, in human periodontal ligament cellsJ Cell Physiol 1995 162(3):359-66. [Google Scholar]
[14]. Hatakeyama I, Marukawa E, Takahashi Y, Omura K, Effects of platelet-poor plasma, platelet-rich plasma, and platelet-rich fibrin on healing of extraction sockets with buccal dehiscence in dogsTissue Eng Part A 2014 20(3-4):874-82. [Google Scholar]