Infections are the most common complications in the burn patients admitted to the hospitals leading to high morbidity and mortality [1]. Burn patients are more prone to nosocomial infections as compared to patients hospitalized for other reasons. This is often attributed to immunocompromized state of burn patients due to disrupted skin barrier, altered physiology, longer stay in hospital and invasive interventions. Prompt antibiotic treatment can be life saving in burn patients. Increasing resistance is the major hurdle to achieve this goal. For an empirical therapy one requires a prior knowledge of prevalence of common bacteria and their antibiotic resistance pattern in that area.
Materials and Methods
A cross-sectional study was conducted at Department of Microbiology, Maulana Azad Medical College, New Delhi in 2012-13. Wound swabs from 1294 patients hospitalized in burnward were collected for bacteriological examination. Swabs were inoculated on blood agar, Mac Conkey agar and brain heart infusion broth. Plates and the broth were incubated at 370C for overnight. Culture plates were checked for the bacterial growth next day.
All bacterial isolates were examined for colony characteristics, Gram staining, motility and biochemical tests. Biochemical tests employed were oxidase, catalase, nitrate, urea hydrolysis, citrate utilization, sugar fermentation, Indole production test and H2S production on TSI agar.
Antibiotic sensitivity
Antibiotic sensitivity testing of Klebsiella isolates was done by modified Stokes disc diffusion method. A suspension of 0.5 McFarland standards was prepared from the colonies of isolated organism and was inoculated along with control strains on Mueller Hinton agar plates by sterile swabs. Antibiotic discs were applied on agar and kept for overnight incubation. The antibiotics that were included for testing were cephalexin (30mcg), ceftriaxone (30mcg), cefotaxime (30mcg), amoxicillin (20mcg), ciprofloxacin (5mcg), gentamicin (10mcg), amikacin (30mcg), imipenem (10mcg), meropenem (10mcg), piperacillin tazobactam (100/10), netilmicin (10mcg), polymyxin B (300unit) and colistin (10mcg).
Statistical Analysis
The data collected was analysed with the aid of the Statistical Package for Social Sciences (Version 10) computer software. A p-value < 0.05 was taken as significant.
Result
Out of 883 isolates from 1294 patients 195 were found to be Klebsiella spp. Based on the biochemical properties 153 isolates were Klebsiella pneumoniae, 37 were Klebsiella oxytoca and 5 were others species.
Klebsiella was the second most common bacteria isolated. On comparison with previous studies from India and abroad we found this unusually high rate of isolation.
On antibiotics susceptibility testing Klebsiella strains from clinical cases were found highly susceptible to imipenem, meropenem, colistin and polymyxin B. At the same time over 50 to 60% strains were found resistant to amoxicillin, gentamicin, ceftriaxone and cefotaxime. Most of the isolates were resistant to cephalexin.55% of the isolates were resistant of third generation cephalosporins [Table/Fig-2].
Percentage of resistant Klebsiella isolates for different antibiotics
| Klebsiella isolates (195) | |
|---|
| Sensitive | Intermediate Sensitive | Resistant | Resistant (%) |
|---|
| Cephalexin | 6 | 1 | 188 | 96 |
| Ceftriaxone | 83 | 4 | 108 | 55 |
| Cefotaxime | 82 | 5 | 108 | 55 |
| Amoxicillin | 73 | 1 | 121 | 62 |
| Ciprofloxacin | 72 | 16 | 97 | 48 |
| Gentamicin | 77 | 1 | 117 | 60 |
| Amikacin | 28 | 4 | 163 | 84 |
| Imipenem | 147 | 12 | 36 | 18 |
| Meropenem | 152 | 19 | 19 | 10 |
| Piperacillin/tazobactam | 121 | 22 | 52 | 26 |
| Netilmicin | 120 | 4 | 71 | 36 |
| Polymyxin B | 180 | 1 | 14 | 7 |
| Colistin | 178 | 1 | 16 | 8 |
Discussion
In our study we found that 54% of the Klebsiella isolates were multidrug resistant as they were resistant to at least one antibiotic of three or more different groups of antibiotics. Sensitivity pattern of multi drug resistant isolates is shown in [Table/Fig-3].
Multidrug resistant Klebsiella
| Multi drug resistant Klebsiella isolates (106) |
|---|
| Sensitive | Intermediate Sensitive | Resistant | Resistant (%) |
|---|
| Cephalexin | 1 | 0 | 105 | 99 |
| Ceftriaxone | 75 | 3 | 28 | 26 |
| Cefotaxime | 75 | 3 | 28 | 26 |
| Amoxicillin | 8 | 12 | 86 | 81 |
| Ciprofloxacin | 0 | 0 | 106 | 100 |
| Gentamicin | 0 | 0 | 106 | 100 |
| Amikacin | 69 | 11 | 26 | 24 |
| Imipenem | 73 | 16 | 17 | 16 |
| Meropenem | 90 | 2 | 14 | 13 |
| Piperacillin/tazobactam | 2 | 0 | 104 | 98 |
| Netilmicin | 94 | 2 | 10 | 9 |
| Polymyxin B | 63 | 1 | 42 | 39 |
| Colistin | 89 | 1 | 16 | 15 |
In the present study we have shown that Gram negative bacteria are the most common bacteria causing burn wound infection. Gram-negative isolates were the five times more in number then Gram-positive pathogens this is consistent with other studies [5–7]. However, some workers have found Gram positive organisms as predominant isolates from burn wounds [8,9].
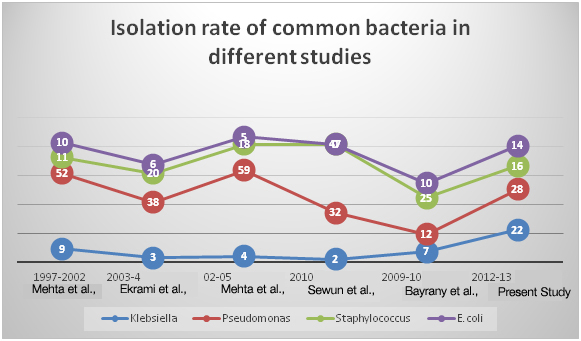
Klebsiella species was the second most frequent pathogen isolated after pseudomonas (28%), accounting for 22% of the total and 26% of all the Gram negative isolates. This is consistent with another study from India which reported Pseudomonas aeruginosa (36%) as the most frequently isolated pathogen [10]. Many studies have reported Klebsiella as the most common organism [11,12]. We have shown that percentage isolation of Klebsiella (22%) was significantly higher than previous studies [Table/Fig-4,5], and we gave special attention to its antibiotic susceptibility pattern.
Comparison of isolates in various studies
| Present study(2012-13) | Mehta et al., [2] 2007(1997-02) | Mehta et al., [2] 2007(2002-05) | Sewunet et al., [13]2013 | Ekrami A et al., [14]2007 | Bayram Y et al., [15]2013(2009-2011) |
|---|
| Pseudomonas | 28 | 59 | 52 | 32 | 38 | 12 |
| Staphylococcus | 16 | 18 | 11 | 47 | 20 | 25 |
| Klebsiella | 22 | 4 | 9 | 2 | 3 | 7 |
| E. coli | 14 | 5 | 10 | --- | 6 | 10 |
| Enterobacter | 1 | 4 | 2 | --- | 2 | 9 |
| Proteus | 8 | 3 | 2 | 17 | 5 | --- |
| Providentia | 2 | --- | --- | 2 | --- | --- |
| Acinetobacter | 8 | 7 | 14 | --- | 10 | 24 |
| Citrobacter | 1 | --- | --- | --- | 2 | --- |
| Morganella | 0.1 | --- | --- | --- | --- | --- |
Isolation rate of common bacteria in different studies
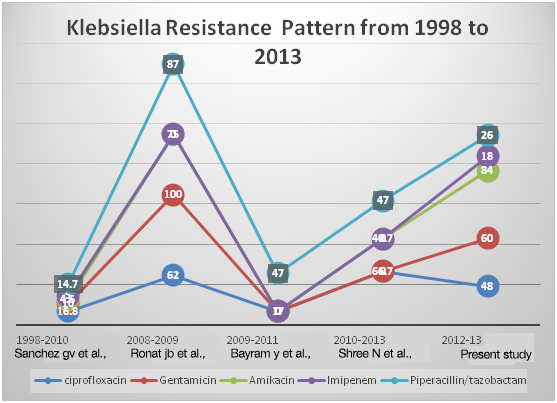
There is great variability in antibiotics resistant percentage in various studies. Comparison of the common antibiotics is shown in [Table/Fig-6]. In this study we found a high rate of resistance for imipenem (18%). Bayraam et al., and Ronat et al., have found no isolate resistant for imipenem however Sanchez et al., has shown only 5% resistance for imipenem [15–17].
Comparison of resistant Klebsiella isolates for common antibiotics
| Antibiotics | Klebsiella isolates resistant to antibiotics (%) | Our study |
|---|
| Sanchez GV et al., [16] | JB Ronat et al., [17] | Bayram Yet al., [15] | Shree N et al., [19] |
|---|
| Ciprofloxacin | 16.8 | 62 | 17 | 66.7 | 48 |
| Gentamicin | 10 | 100 | 0 | -- | 60 |
| Amikacin | 4.5 | 75 | 0 | 40.7 | 84 |
| Imipenem | 5 | 0 | 0 | 0 | 18 |
| Piperacillin/tazobactam | 14.7 | 87 | 47 | 47 | 26 |
Klebsiella resistance pattern from 1998 to 2013
Fifty four per cent of the Klebsiella isolates were multi drug resistant. They were resistant to at least one antibiotic of three or more antibiotics group of different mechanism of action. All of the multidrug resistant isolates were resistant to ciprofloxacin and Gentamicin. Only two isolates of Klebsiella species were sensitive for piperacillin/tazobactam which is a commonly used antibiotic combination used for the Gram negative bacteria.
If we see the resistance pattern of Klebsiella spp over the years, its resistance has not come down. In our study 16 % resistance for Imipenem is very high comparing to the other studies in which very less resistance (0 to 5%) for imipenem was observed. This might have happen due to the inclusion of only burn patients in our study. For gentamicin people have reported resistance from 0-100%. But for other antibiotics overall trends show that there is no decrease in their resistance pattern.
Most MDR isolates were resistant to cephalosporins which are commonly used for Klebsiella infection as monotherapy and in combination with other. Although plasmid mediated resistance to broad spectrum antibiotics is a common phenomenon among the members of family Enterobacteriaceae but it is more commonly seen with Klebsiella spp. These bacteria inactivates broad spectrum antibiotics by producing extended spectrum beta lactamase enzymes. Although in our study MDR Klebsiella showed lowest resistance to meropenem, imipenem, netilmicin, and colistin, but there were isolates which were resistant to these antibiotics. Being plasmid mediated this resistance can be transferred horizontally from one bacterium to another. Which is an alarming state and needs to be addressed by prompt identification, isolation and treatment of the infection cases. Successful decrease in mortality and morbidity has been reported in burn patients by prompt isolation and treatment [18].
Conclusion
We have shown that Klebsiella stays as an important isolate from burn wound infections and its rate of isolation has increased in last ten years. Also, it appears that the resistance to the commonly used antibiotics is increasing over the time. There is a need for similar studies from the other health care facilities.