Deceptive Lesions of Periodontium: A Case Series
Deepak Pandiar1, Manjusha Pattamparambath2, Pranav Vijayan Kalathingal3, Shameena Pallikandi Maliyekkal4, Amol Nagrale Vijay5
1 Research Scholar, Faculty of Dental Sciences, IMS, BHU, Varanasi, UP, India.
2 Post Graduate Trainee, Department of Oral Pathology and Microbiology, GDC, Calicut, Kerala, India.
3 Post Graduate Trainee, Department of Oral Pathology and Microbiology, GDC, Calicut, Kerala, India.
4 Head of Department, Department of Oral Pathology and Microbiology, GDC, Allapuzha, Kerala, India.
5 General Practitioner, Periodontist and Implantologist, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Deepak Pandiar, Research Scholar, Faculty of Dental Sciences, IMS, BHU, Varanasi-221005, UP, India. E-mail : deepakpandiar1923@yahoo.com
Basic pathology of the common appearing diseases of the periodontium are not always common inflammatory reactions. The root cause may be malignant and metastatic lesions. Here, we present unusual causes of these common periodontal lesions. This article also stress upon the importance of histopathological examination of the surgically excised localized gingival swellings which fail to regress after conservative therapy.
Gingival enlargements, Lymphoma, Metastasis, Periodontitis
Case Report
Case 1: A 70-year-old male patient reported to the Department of Oral Medicine and Radiology, Government Dental College, Calicut, Kerala with a chief complaint of spontaneous bleeding from gums since 1 month. The patient had consulted a physician who discerned a swelling in 43-45 tooth region. There was no associated pain. Patient was asthmatic and had a psychogenic disorder. He was under medication for these conditions. The patient was using corticosteroids, salbutamol by inhalation, for last nine years. The patient had smoking habit for 39 years but was non-alcoholic. The patient appeared chronically ill and drowsy but could be awakened easily. The pulse rate was 95/min; fast and irregular but veins appeared thickened on palpation. Respiratory rate, temperature and blood pressure were within normal limits. Right sub-mandibular and upper cervical lymph nodes were palpable but mobile and non-tender. The patient passed black, sticky and tarry stools however micturition habits were normal.
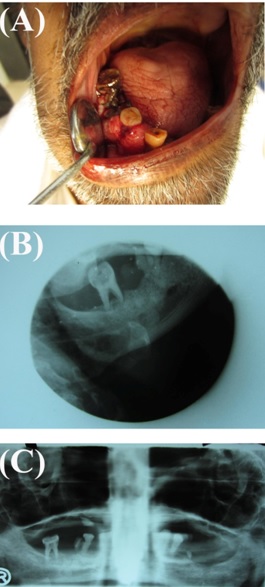
On intraoral inspection, a growth of about 1.5 X 2.5 cm was noticed in relation to 43-47 region [Table/Fig-1a]. The surface of the swelling was smooth and erythematous. On palpation, the growth was non-tender and soft in consistency. It measured 1.7 X 2.3 X 1.4 cm, extended from distal aspect of 43 to mesial aspect of 47 and bled even on slight provocation. The margins were well defined. Oral hygiene was poor. Panoramic radiograph showed generalized bone loss [Table/Fig-1b&c]. A clinical diagnosis of pyogenic granuloma was made and a piece of tissue was incised which was fixed in 10% formalin and sent to the Department of Oral Pathology and Microbiology for histopathological examination.
(Case 1): (a) An erythematous soft growth on mandibular gingiva; (b,c) radiographs showing generalized alveolar bone loss
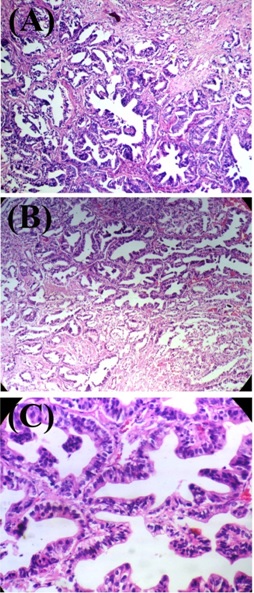
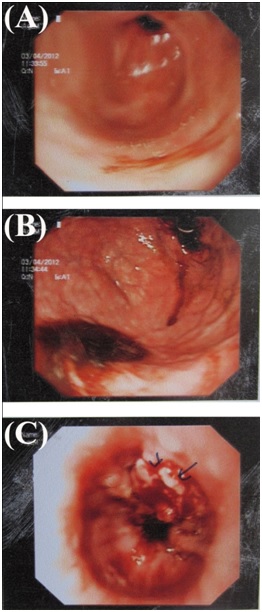
Light microscopy (H&E sections) showed tissue composed of small to large closely apposed duct like spaces, lined by 1-2 layers of tall columnar cells with round to oval vesicular nuclei and papillary projections into the lumen [Table/Fig-2a-c]. At some areas the nuclei were deeply basophilic. In addition few cells showed clear cytoplasm. In some duct like spaces pale eosinophilic material was seen. Numerous mitotic figures were also present. The intervening minimal connective tissue was fibrous and contained chronic inflammatory cells chiefly lymphocytes and endothelium lined vascular spaces. The report was consistent with papillary adenocarcinoma. Based on the histopathologic features and a history of black stools, gastric endoscopy was advised which revealed a non circumferential, friable ulcero-proliferative growth across gastro-oesophageal (GE) junction ([Table/Fig-3a-c]; Suggestive of carcinoma- GE junction). Gastric biopsy revealed the primary tumour. Keeping the general physical condition and age of the patient palliative care was initiated but the patient succumbed to disease within a period of two weeks after diagnosis.
(Case 1) (a,b) H&E section at 100 X magnification; (c) H&E section at 400 X magnification
(Case 1)(a,b) Endoscopic images showing normal antrum and fundus; (c) An ulceroproliferative growth of gastro-esophegeal junction (endoscopic image)
Case 2: A 52-year-old male patient reported to the Department of Oral Pathology and Microbiology, Government Dental College, Calicut, Kerala presenting with a chief complaint of a rapidly growing swelling in the 33-35 tooth region since 3 months. The patient was smoker and consumed alcohol occasionally. The vital signs were within normal limits. No lymphadenopathy was noted. He had a history of carcinoma of thyroid for which radiotherapy was given about 4 years back. On examination a sessile erythematous lesion was seen in relation to 33-35 extending labially and lingually [Table/Fig-4a]. The associated teeth were grade 2 mobile. Based on the history of thyroid carcinoma, a provisional diagnosis of metastatic thyroid tumour was thus made. Fine needle aspiration cytology (FNAC) was done and the smear showed tumour cells arranged in clusters. Some of the cells are arranged in multilayered complex papillary arrangement [Table/Fig-4b]. The presence of the complex papillary clusters (observed under low power) is usually diagnostic of the tumour. Under higher power, the cells were round with hyper-chromatic nuclei and moderate amount of basophilic cytoplasm with moderately altered nucleo-cytoplasmic ratio [Table/Fig-4c] and showed intra-nuclear inclusion [Table/Fig-4c inset]. Presence of these intra nuclear inclusions are of more diagnostic importance and existence of more than three such inclusions on a single aspirate of a thyroid nodule is considered to be almost pathognomonic for a papillary carcinoma.
(Case 2): (a) A sessile erythematous growth on left anterior mandibular gingiva; (b) PAP smear showing malignant tumour cells in complex papillary arrangement; (c) PAP smear shows sheets of follicular cells with basophilic nuclei and enlarged nucleus with intranuclear inclusions (inset); (d&e) H&E section at 40X and 100X magnification respectively; (f) H&E section at 400X magnification (inset: tumour cells positive for thyroglobulin immunohistochemically)
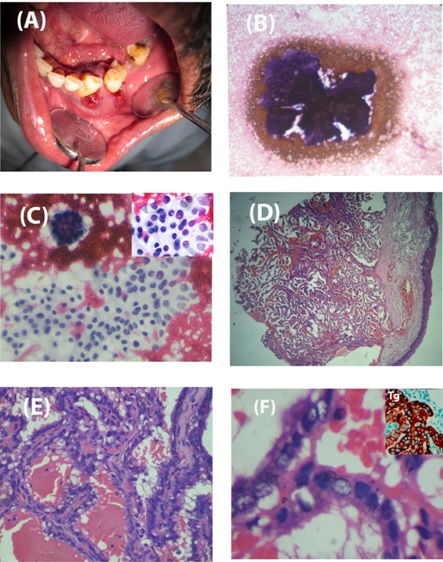
Considering the cytological findings, a diagnosis consistent with malignant neoplasm of thyroid was made. Thereafter an incisional biopsy was done and based on H&E and immunohistochemical analysis (positive for thyroglobulin; [Table/Fig-4d-f]); a final diagnosis of metastatic papillary carcinoma of thyroid was made. The lesion was excised widely and adjuvant radiotherapy was given. The patient died of multiple metastases after a period of one and a half years.
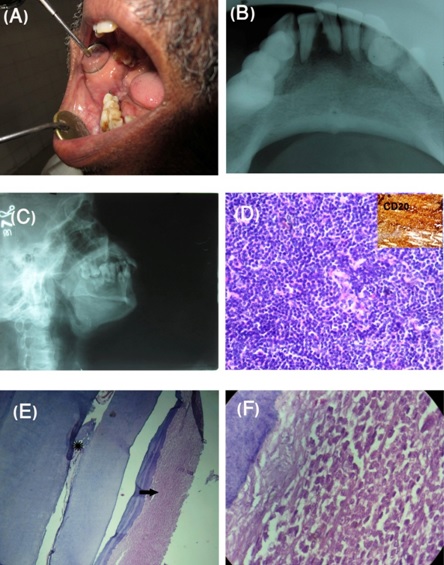
Case 3: A 53-year-old male patient was referred to the Department of Oral Medicine and Radiology, Government Dental College, Calicut, Kerala with a chief complaint of swelling in the right back tooth region since 5 months. The patient had no deleterious habits and the vital signs were within normal range. On examination a swelling of approximate size of 2x2 cm was noticed in the right retromolar region extending slightly onto the buccal mucosa [Table/Fig-5a]. It was rubbery in consistency but non tender. There was no lymphadenopathy. Routine blood picture was normal. There were generalized stains on the teeth and plaque and calculus deposits were minimal. Radiograph showed generalized bone loss around the teeth [Table/Fig-5b&c] and it was clinically evident as deep pockets and tooth mobility. A clinical diagnosis of fibroma with generalized chronic periodontitis was made. 46 showed advanced mobility which was extracted and submitted along with the excised specimen to histopathology laboratory. The soft tissue was routinely processed for H&E staining. The tooth specimen was decalcified in 8% nitric acid and routinely processed thereafter. The histopathology of the soft tissue specimen was consistent with non Hodgkin’s lymphoma (NHL; [Table/Fig-5d]) which was further confirmed by positive immunohistochemistry for CD45 and CD20 (B Cell NHL; [Table/Fig-5d] inset). It was interesting to find out that the decalcified specimen showed infiltration of tumour cells into the periodontal ligament destroying the normal fibers however no infiltration was seen in the dental pulp [Table/Fig-5e-f]. The patient received radiotherapy and is under follow-up. At present he is free of any clinical recurrence and metastasis.
(Case 3): (a) A proliferative growth of right retromolar region; (b&c) Radiographs showing generalized advanced alveolar bone loss with normal appearing basal bone; (d) H&E section at 100 X magnification (inset: tumour cells positive for CD 20 immunohistochemically); (e) Decalcified section showing tumour cells infiltrating periodontal ligament (arrow) however no lymphoma cells are seen in the pulp (asterisk); (f) Decalcified section at 400X showing PDL fibre destruction and replacement by tumour cells
Discussion
An oral health care-taker frequently comes across gingival enlargements and periodontitis in the clinic; however, the underlying pathology of these common conditions may be so unusual that the clinicians usually do not contemplate these causes in their differential diagnosis. The root cause may be an innocuous inflammatory condition to ominous neoplastic and metastatic ones.
The gingival enlargements seen in the oral cavity are usually inflammatory conditions but may be the manifestations of drug intake, underlying systemic diseases or osseous conditions and less commonly the neoplastic conditions [1]. The benignancy or malignancy of these neoplasms decides the outcome of such enlargements. Primary malignant lesions from other distant body parts may at times metastasize to gingiva resulting in enlargements which mimic pyogenic granuloma clinically and here remedies like local excision is not curative. Metastatic carcinomas to oral region constitute approximately 1% of all oral malignancies; breast, lung, adrenal, kidney, gastrointestinal tract and prostate being the most common sites for primary tumour [2]. Thyroid carcinoma metastasizing to the jaw is extremely rare accounting for about 3.85% of all jaws metastases [3].
Similarly, periodontitis is also an inflammatory condition caused by local irritants and may be modified by systemic conditions. At present, diagnosis of periodontitis as a manifestation of systemic diseases is made when the systemic condition is the main cause and local factors are not clearly evident. In cases where the periodontal destruction is clearly the result of local factors but has been exacerbated by the onset of condition such as diabetes mellitus or HIV etc, the diagnosis of chronic periodontitis modified by the systemic condition should be made [1].
Breast cancer and lung cancer are the most common malignancies to give oral metastases in females and males respectively [2]. Metastasis from gastric and thyroid carcinoma to the oral tissues is a rare event. These tumours tend to metastasize to the jaw bones more commonly than oral soft tissues (2.5:1) [2]. Gingiva is the most commonly affected site followed by tongue, lips, buccal and palatal mucosa [4,5]. In the oral soft tissues, the rich capillary network of chronically inflamed gingiva can entrap malignant cells. The proliferating capillaries have a fragmented basement membrane through which tumour cells can more easily penetrate [6].
Malignant lymphomas are a diverse group of neoplasms affecting the lymphoid system and are subdivided into two main groups: Hodgkin’s lymphoma, and non-Hodgkin’s lymphoma (NHL) [7]. NHL may develop extra-nodally outside the lymphoid system and can occur in the stomach, skin, lung, salivary glands and rarely in the mouth. In the oral region, extra-nodal NHL may occur in the jaw bone as well as in the oral soft tissues [8]. Malignant tumour cells may also pervade the pulp and periodontal ligament [9,10]. When suffusing the PDL, periodontitis may be one of the features. In such cases diagnosis of periodontitis is made in the absence of large quantities of local irritating factors such as plaque and calculus. Plasma cell myeloma and leukemic and infiltration to these structures is well documented and illustrated [10]. Although infiltration of the lymphoma cells in the PDL is documented in the literature [11], it is not well illustrated.
In the present case series we have reported two cases of metastatic tumours of oral cavity presenting as gingival enlargement. In Case 1 of our series, the oral lesion was the first sign of the occult metastasis. Gastric carcinoma present no or mild signs at early stages and that is why at the time of detection the tumour is advanced or metastatic [12]. In approximately 30% of the cases the oral lesion leads to the diagnosis of the primary tumour [13]. Similar to our case, Mehta et al., also reported metastasis of oesophegeal signet cell carcinoma to gingiva. They gave a clinical diagnosis of pyogenic granuloma and correct diagnosis and detection of occult primary could be made only after histological examination of specimen from gingiva [14]. The Case 2 in the series showed metastasis of papillary carcinoma of thyroid, which is a rare event. Until the year 2012 only 8 such cases have been reported [15]. Recently in 2013, Verma et al., reported a rare event of coexistence of papillary carcinoma of thyroid and squamous cell carcinoma [16]. The prognosis is grave for metastatic neoplasms to the oral cavity. The time from the appearance of the metastasis to death is several months [2]. Thus, in a rapidly enlarging suspicious gingival growth, metastatic tumours should be kept in the differential diagnosis. The case 3 is an extra-nodal B cell NHL with infiltration of tumour cells in the periodontal ligament. Large quantities of plaque and calculus were not evident, thus the periodontitis in this case may be a manifestation of systemic disease.
Benign appearing gingival exophytic lesions may be the sole manifestation of metastasis thus metastatic lesions should be kept in mind while dealing with lesions such as pyogenic granuloma, peripheral ossifying fibroma, peripheral giant cell granuloma and hemangioma. Rareness of metastatic oral lesion demands high degree of suspicion by both clinicians and pathologists.
Conclusion
There appear to be similarities between the clinical appearances of different types of gingival overgrowths. Gingival growth may be the result of life threatening metastatic lesions. Therefore, it is important to keep them in the differential diagnosis of gingival enlargements and when total excision is done it is mandatory to evaluate them histologically.
[1]. Novak MJ, Classification of the diseases and conditions affecting the periodontium. In: Newman M, Takei H, Carranza F ACarranza’s Clinical Periodontology 2006 9th edPhiladelphiaSaunders:70 [Google Scholar]
[2]. Hirshberg A, Shnaiderman Shapiro A, Kaplan I, Berger R, Metastatic tumours to the oral cavity: pathogenesis and analysis of 673 casesOral Oncol 2008 44:743-52. [Google Scholar]
[3]. Hirshberg A, Leibovich P, Buchner A, Metastatic tumours to the jawbones: analysis of 390 casesJ Oral Pathol Med 1994 23:337-41. [Google Scholar]
[4]. Sauerborn D, Vidakovic B, Baranovic M, Mahovne I, Danic P, Danic D, Gastric adenocarcinoma metastases to the alveolar mucosa of the mandible: a case report and review of the literatureJ Craniomaxillofac Surg 2011 39:645-48. [Google Scholar]
[5]. Florio SJ, Hurd TC, Gastric carcinoma metastatic to the mucosa of the hard palateJ Oral MaxillofacSurg 1995 53:1097-98. [Google Scholar]
[6]. Rajendran R, Shivpadsundaram B, Shafer’s text book of oral pathology 2006 5th editionIndiaElsevier Publication:289 [Google Scholar]
[7]. Parrington SJ, Moorthy P, A Primary non-Hodgkin’s lymphoma of the mandible presenting following tooth extractionBritish Dental Journal 1999 187:468-70. [Google Scholar]
[8]. Kobler P, Borcic J, Zore I, Filipovic, Nola M, Sertic D. Primary non-Hodgkin’s lymphoma of the oral cavityOral Oncology Extra 2005 41:12-14. [Google Scholar]
[9]. Lu SY, Oral manifestations of metastasis from solid cancers and leukemia- 43 cases in a 15-year retrospective studyJ Dent Sci 2006 1:114-25. [Google Scholar]
[10]. George S, Shameena PM, Sudha S, Sherin N, Plasma cell myeloma infiltrating the dental pulp: An interesting findingJ Oral MaxillofacPathol 2013 17:417-19. [Google Scholar]
[11]. Hokett SD, Cuenin MF, Peacock ME, Thompson SH, Van Dyke TE, Non-Hodgkin’s lymphoma and periodontitis. A case reportJ Periodontol 2000 71:504-09. [Google Scholar]
[12]. Roukos DH, Agnantis NJ, Gastric cancer: Diagnosis, staging, prognosisGastr Breast Cancer 2002 1:7-10. [Google Scholar]
[13]. Regezi JA, Sciubba JJ, Jordan RCK, Oral pathology: Clinical pathologic correlations 2012 6th edElsevierW.B. Saunders:343 [Google Scholar]
[14]. Mehta DN, Bailoor DN, Tarsariya VM, Parikh BP, From esophagus to gingiva: A rare case of metastatic adenocarcinomaJ Oral MaxillofacPathol 2012 16:428-31. [Google Scholar]
[15]. Nikitakis NG, Polymeri A, Polymeris A, Sklavounou A, Metastatic Papillary Thyroid Carcinoma to the Maxilla:Case Report and Literature ReviewHead and Neck Pathol 2012 6:216-23. [Google Scholar]
[16]. Verma RK, Tripathi N, Aggarwal P, Panda NK, Metastatic papillary carcinoma thyroid co-existing with oral cavity squamous cell carcinoma: A case report and review of literatureEgyptian Journal of Ear, Nose, Throat and Allied Sciences 2014 15:125-28. [Google Scholar]