Co-Existence of Acinic Cell Carcinoma - Papillary Cystic Variant and Extrapulmonary Tuberculosis – Report of A Case with Brief Review
Krishnappa Amita1, Shivshankar Vijayshankar2, Manchaiah Sanjay3
1 Associate Professor, Department of Pathology, Adichunchanagiri Institute of Medical Sciences, B.G. Nagara, Mandya District, Karnataka, India.
2 Professor, Department of Pathology, Adichunchanagiri Institute of Medical Sciences, B.G. Nagara, Mandya District, Karnataka, India.
3 Assistant Professor, Department of Pathology, Adichunchanagiri Institute of Medical Sciences, B.G. Nagara, Mandya District, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Krishnappa Amita, Associate Professor, Department of Pathology, Adichunchanagiri Institute of Medical Sciences, B.G. Nagara, Mandya District, Karnataka-571448, India. E-mail : dramitay@rediffmail.com
Tuberculosis (TB) and cancer are two lethal diseases causing significant morbidity and mortality in developing countries like India. Co-existence of these two disease lead to diagnostic dielemma among the clinicians. Overlapping clinical manifestations lead to delay in diagnosis. We report a case of acinic cell carcinoma –papillary cystic variant of the salivary gland and extra pulmonary tuberculosis in a young female. We emphasize the importance of the awareness of the co-existence of these two diseases and the role of fine needle aspiration cytology in the initial diagnosis.
Cytology, Fine needle aspiration
Case Report
A 28-year-old female presented with swelling in the pre-auricular region of two years duration. The swelling was slowly increasing in size and was not associated with pain. She also complained of swelling in the cervical region of 20 days duration. This swelling was rapidly increasing in size and was not associated with pain. On further questioning she gave a positive history of fever on and off, with a history of weight loss and loss of appetite. On examination the pre-auricular swelling was located in the parotid region and measured 1×1 cm. The swelling was non tender, firm to hard in consistency and mobile. Overlying skin was unremarkable. Facial nerve was not involved. Swelling in the cervical region was 4×2 cm, firm in consistency and freely mobile. A provisional clinical diagnosis of a parotid gland tumour probably malignant due to associated lymphadenopathy was rendered. Ultrasound findings suggested a similar diagnosis. Haematology investigations were within normal limits except for haemoglobin which was 8 gm/dl and ESR of 40mm at the end of first hour by Westergren’s method.
Fine needle aspiration cytology (FNAC) was done from both pre auricular swelling and cervical lymph node.
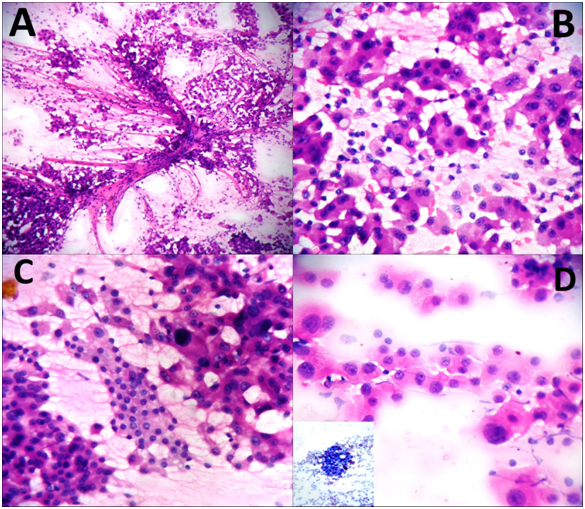
Cytology smears from pre auricular swelling showed abundant cellularity comprising of tumour cells arranged in acini, sheets and papillary pattern. Tumour cells were seen clinging to the fibro vascular core. The individual cells were large polygonal with abundant eosinophilic granular cytoplasm, nucleus with moderate anisonucleosis and prominent 1 to 2 nucleoli. Also seen were vacuolated cells with multi vacuolated to clear cytoplasm. Sheets of ductal epithelial cells with uniform appearance were noted [Table/Fig-1a-d]. Additional findings included haemosiderin pigment, bare nuclei and lymphocytic sprinkling in the background. Based on these cytomorphological features a final diagnosis of an acinic cell carcinoma was made.
a) Cytology smears showing papillary pattern, tumour cells were seen clinging to the fibro vascular core. (H&E, X 40)
b) Cytology smears showing acinar pattern. (H&E, X 100)
c) Cytology smears showing sheet of ductal epithelial cells. (H&E, X 100)
d) Cytology smears showing anisokaryosis. (H&E, X 100) Inset shows vacuolization (Giemsa, X 40)
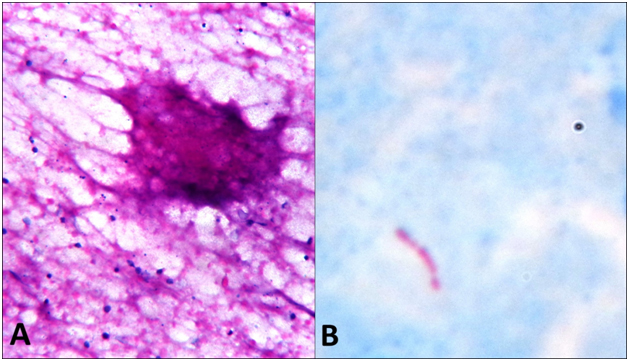
Cytology smears from the right cervical lymphnode showed caseation necrosis with epitheloid cells in clusters. Acid fast stain for tubercle bacilli was positive [Table/Fig-2a,b].
a) cytology smears show caseation necrosis. (H&E, X 400)
b) Cytology smears show positive acid fast bacilli. (Ziel Nelson, X 400)
Hence, a final diagnosis of acinic cell carcinoma of salivary gland associated with cervical tuberculosis lymphadenitis was made.
Patient was started on anti tuberculosis therapy and surgery was planned a week later. Preoperative w workup comprising of biochemistry, haematology and radiology investigations were within normal limits.
At surgery subtotal parotidectmy was performed and the specimen was sent for histopathological examination.
Gross: Cut surface of the specimen showed a well defined encapsulated tumour mass in the parotid gland measuring 1×1 cm. The tumour was homogenous, lobulated and grey white.
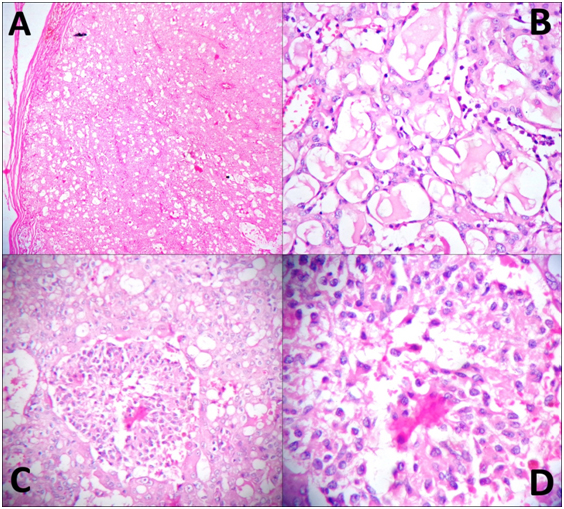
Histopathology: Sections showed an encapsulated tumour with normal parotid gland at the periphery. Focal capsular invasion was noted. The tumour cells were arranged in acini, papillary pattern and in sheets. At places micro cystic pattern was noted. Individual tumour cells were polygonal with amphophilic granular cytoplasm, at many places showing micro vacuolation and clearing. Nuclei showed moderate anisokaryosis with fine chromatin and prominent nucleoli [Table/Fig-3a-d]. A final histopathological diagnosis of acinic cell carcinoma-Papillary cystic variant was made.
a) Section studied shows tumour which is encapsulated. (H&E, X 100)
b) Section studied shows acini with luminal secrections. (H&E, X 100)
c) Section studied shows ductal cells in sheets. (H&E, X100)
d) Section studied shows ductal cells in sheets. (H&E, X400)
Patient responded well to anti tuberculosis therapy and the postsurgical period was also uneventful. Follow up after one year was remarkably good.
Discussion
Cancer is a major public health problem worldwide. About one million new cases of cancer are being diagnosed every year, the plausible projected mortality incidence being 1.7 million in 2035 [1]. On the other hand, tuberculosis is in fact the major killer disease with India representing 26% of the total tuberculosis deaths globally, with 1.98 million new cases diagnosed annually [2]. Association of tuberculosis with cancer has fascinated clinicians and researchers for a long time. Documentation in the literature dates back to some 200 years ago when Bayle described the association by proposing cancer as a type of tuberculosis [3,4]. Later, Pearl, based on the autopsy study observed that lung cancer occurred with less frequency in tuberculosis patients and he proposed tuberculin for treating cancer. Pearl’s views were endorsed by Rokitansky and Berrroya. Antagonist for the pearl’s theory was Carlson and Bell. However, it was Pilliet and Plattot who first described the association of tuberculosis and cancer [5]. Ever since then, many authors have reported association of tuberculosis with cancers in various organs in the body. Kaplan et al., studied 210 cases which had co-existence of TB and cancer [6]. Similarly, Falgas conducted an extensive review of literature regarding the association of these two diseases. According to their observation, malignancies occurring in association with tuberculosis include lymphomas, leukaemia, cancer of lung, colon, bladder, uterus, breast, prostate and kidney [7]. Tuberculosis lymhadenopathy has been reported to occur in association with various neoplasm including breast cancer, haematological, gastrointestinal tract, pulmonary and thymic malignancy [7]. Tuberculosis occurring in Warthin’s tumour and pleomorphic adenoma of the salivary gland has been documented in the literature. However in all, the cases numbers are few and both the pathologies occurred concurrently in salivary gland [8]. Extensive search of English literature did not reveal any report of co-existent of extra pulmonary tuberculosis in lymph node and acinic cell carcinoma papillary cystic variant of the salivary gland.
Co-existence of tuberculosis and malignancy in the same patient has several practical implications. Clinical manifestation of two diseases show a considerable overlap, even modern imaging techniques cannot accurately diagnose either condition with precision. Tuberculosis, being a chronic inflammatory disease can act as a risk factor for cancer development, which needs to be substantiated and the research on which is still on. Similarly malignancy and the associated chemotherapy produce an immune deficient state in the patient, making way to reactivation of latent tuberculosis or acquisition of a new infection [9]. Delay in diagnosis leading to delay of or non institution of therapy in these cases will lead to dissemination of tuberculosis infection. This, the clinician may falsely attribute to the worsening of malignancy or due to the effect of anticancer drugs. Both diagnosis and management is a big challenge for the clinicians in these cases. More so, the presence of a lymph node enlargement due to tuberculosis may lead to over staging of the malignant process clinically.
Acinic cell carcinoma is a rare tumour of parotid gland accounting for 1 to 3% of all the salivary gland tumours. Prognosis of acinic cell carcinoma is excellent with five year survival rate being 90%. Lymph node metastases are seen in 10% of the cases and entail a poor prognosis. FNAC is a popular method for diagnosis of various salivary gland lesions. However, the accuracy rate is low for malignant lesions as compared to benign tumours, even more so for sub typing of malignant tumours. Diagnosis of acinic cell carcinoma by FNAC can be particularly challenging especially in the papillary cystic variant which is unique and rare entity, the false negative rate being very high (7.1%) [10,11]. More commonly acinic cell carcinoma is easily confused with normal salivary gland aspirate. Other tumours with which ACC is confused are oncocytoma, clear cell carcinoma, muco epidermoid carcinoma, epithelial myoepithelial carcinoma and metastatic renal cell carcinoma. However, careful attention to cytomorphology aids in the precise diagnosis of malignancy as well as in accurately sub typing it. Presence of discohesive fragments and of bare nuclei, absence of adipocyte fragments and ductal cells helps to differentiate ACC-PCV from normal salivary gland/sialadenosis [7]. Similarly, oncocyte like cytoplasm can be seen in ACC-PCV but it will be intermixed with other cell type like clear – vacuolated cells, ductal cells and granular cells. Whilst in oncocytoma, the predominant population is usually monomorphic [11]. In the papillary cystic variant of ACC, cystic fluid in the smear and vacuolated clear cells can mimic mucin and mucin secreting cells leading to an erroneous diagnosis of mucoepidermoid carcinoma [12]. The vacuolated cells of mucoepidermoid carcinoma are positive for mucin while those of acinic cell carcinoma are mucin negative. Basement membrane material and occasionally hyaline globules typifies epithelial myoepithelial carcinoma. A history of renal cell carcinoma points to the diagnosis of metastasis of renal cell carcinoma [13]. In addition, papillary fragments of histiocytic cells or vacuolated cells or granular cells are a clue to the diagnosis. Since a plethora of lesions including non neoplastic lesions, benign tumours and various malignancies can mimic ACC–PCV, careful attention to the cytomorphology is important.
Conclusion
The co-existence of extrapulmonary tuberculosis of the lymph node with a rare and unique tumour of salivary gland i.e, ACC-PV is unusual. Awareness of the occurrence of this rare tumour variant, its cytomorphology and the co-existence with extrapulmonary tuberculosis is must for clinicians and pathologist in making an early yet precise diagnosis and scheduling appropriate management.
[1]. Mallath MK, Taylor DG, Badwe RA, Rath GK, Shanta V, Pramesh CS, The growing burden of cancer in India: epidemiology and social contextThe Lancet Oncology 2014 15:e205-12. [Google Scholar]
[2]. Global Tuberculosis Control 2012, WHO, Geneva, 2012 www.who.int/tb/publications/global_report/ [Google Scholar]
[3]. Bayle GL: Recherches Sur la Phthisis Pulmonaire Paris, 1810: 315 as quoted by Jackson et al., (1957) [Google Scholar]
[4]. Jackson A, Garber PE, Post GW, Co-existing pulmonary tuberculosis and malignancyDis. of Chest 1957 32:189-97. [Google Scholar]
[5]. Harikrishna J, Sukaveni V, Prabath Kumar D, Mohan A, Cancer and tuberculosisJournal Indian Academy of Clinical Medicine 2012 13:142-44. [Google Scholar]
[6]. Kaplan MH, Armstrong D, Rosen P, Tuberculosis complicating neoplastic disease. A review of 201 casesCancer 1974 33:850-58. [Google Scholar]
[7]. Falagas ME, Kouranos VD, Athanassa Z, Opterides PK, Tuberculosis and malignancyQ J Med 2010 103:461-87. [Google Scholar]
[8]. Al Bisher H, A rare case of primary tuberculosis infection with concurrent pleomorphic adenoma of the parotid glandInfectious Disease Reports 2010 2:6 [Google Scholar]
[9]. Silva FA, Matos JO, de Q, Mello FC, Nucci M, Risk factors for and attributable mortality from tuberculosis in patients with haematologic malignancesHaematologica 2005 90:1110-15. [Google Scholar]
[10]. Mosunjac MB, Siddiqui MT, Tadros T, Acinic cell carcinoma-papillary cystic variant. Pitfalls of fine needle aspiration diagnosis: study of five cases and review of literatureCytopathology 2009 20:96-102. [Google Scholar]
[11]. Jain R, Gupta R, Kudesia M, Singh S, Fine needle aspiration cytology in diagnosis of salivary gland lesions: A study with histologic comparisonCyto Journal 2013 10:5 [Google Scholar]
[12]. Shet T, Ghodke R, Kane S, Chinoy RN, Cytomorphologic patterns in papillary cystic variant of acinic cell carcinoma of the salivary glandActa Cytol 2006 50:388-92. [Google Scholar]
[13]. Mukunyadzi P, Review of fine-needle aspiration cytology of salivary gland neoplasms, with emphasis on differential diagnosisAm J Clin Pathol 2002 118:100-15. [Google Scholar]