Post Surgical Giant Epidermal Inclusion Cyst of the Lid and Orbit- A Rare Case
Salil Kumar Mandal1, Aparna Mandal2, Arghya Bandyopadhya3
1 Associate Professor, Department of Ophthalmology, Regional Institute of Ophthalmolog, Medical College & Hospital, Kolkata, India.
2 Assistant Professor, Department of Physiology, College of Medicine & Sagore Dutta Hospital, West Bengal, India.
3 Demonstrator, Department of Pathology, Burdwan Medical College & Hospital, West Bengal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Salil Kumar Mandal, 183.R.N. Guha Road. DumDum, Calcutta-700074, West Bengal, India. E-mail : salil_dum@live.com
Epidermoid cyst within the lid and orbit is extremely rare. Epidermoid tumours are inclusion of ectodermal elements in the site not normally containing these structures. It is of two types; primary type related to implantation of ectoderm at the time of closure of the neural groove and secondary type caused by post traumatic inclusion of the surface epithelium. A 45-year-old male had complaint of swelling on the right upper lid and orbital region. It first appeared two years back. It was painless progressively increased in size and shape. There was difficulty in opening of eye lid due to large swelling, feeling of heaviness in the right upper lid and occasional headache. There was history of right eye ocular infection following vegetative matter injury three years back. Evisceration of right eye was done for aforementioned reason. USG report shows cystic encapsulated mass with calcification foci in right upper lid-orbital region with fat component. MRI right orbit shows fairly large hyperintense cystic lesion seen involving right orbit with posterior extension up to optic canal. No intracranial extension. FNAC confirmed epidermal inclusion cyst. We did upper lid reconstruction with removal of mass. We have successfully removed the mass without any complication and with one year follow-up there is no recurrence.
Dermoid cyst, Lid tumour, Orbital cyst, Sebaceous cyst
Case Report
A 45-year-old male had a swelling at the right upper lid and orbital region since two years. It first appeared as painless progressive swelling which increased in size and shape. Difficulty in opening of the eyelid due to large swelling and heavy weight of the mass, feeling of heaviness in the right upper eyelid and occasional headache history of right ocular infection following vegetative matter injury three years back, evisceration of the right eye done for aforementioned reason.
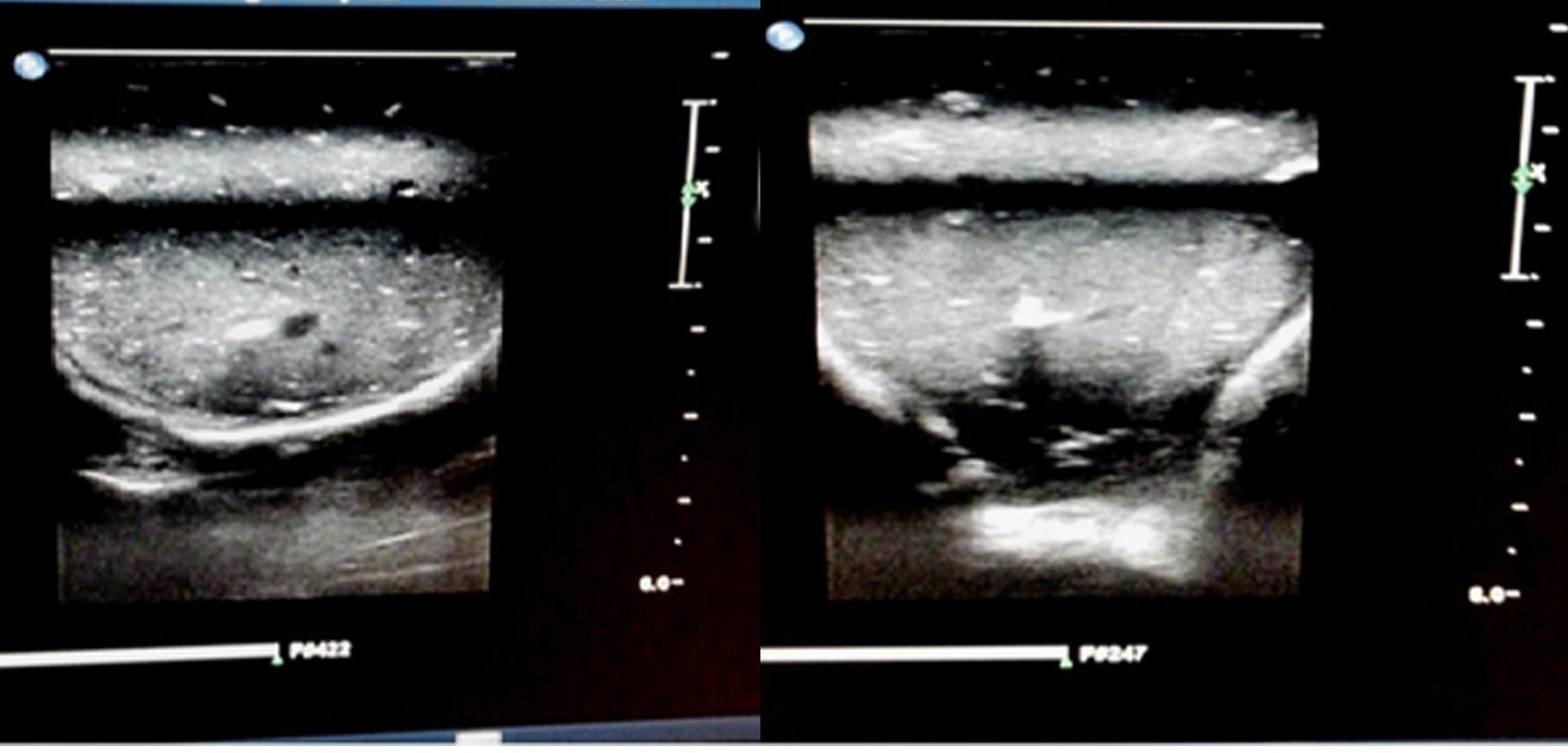
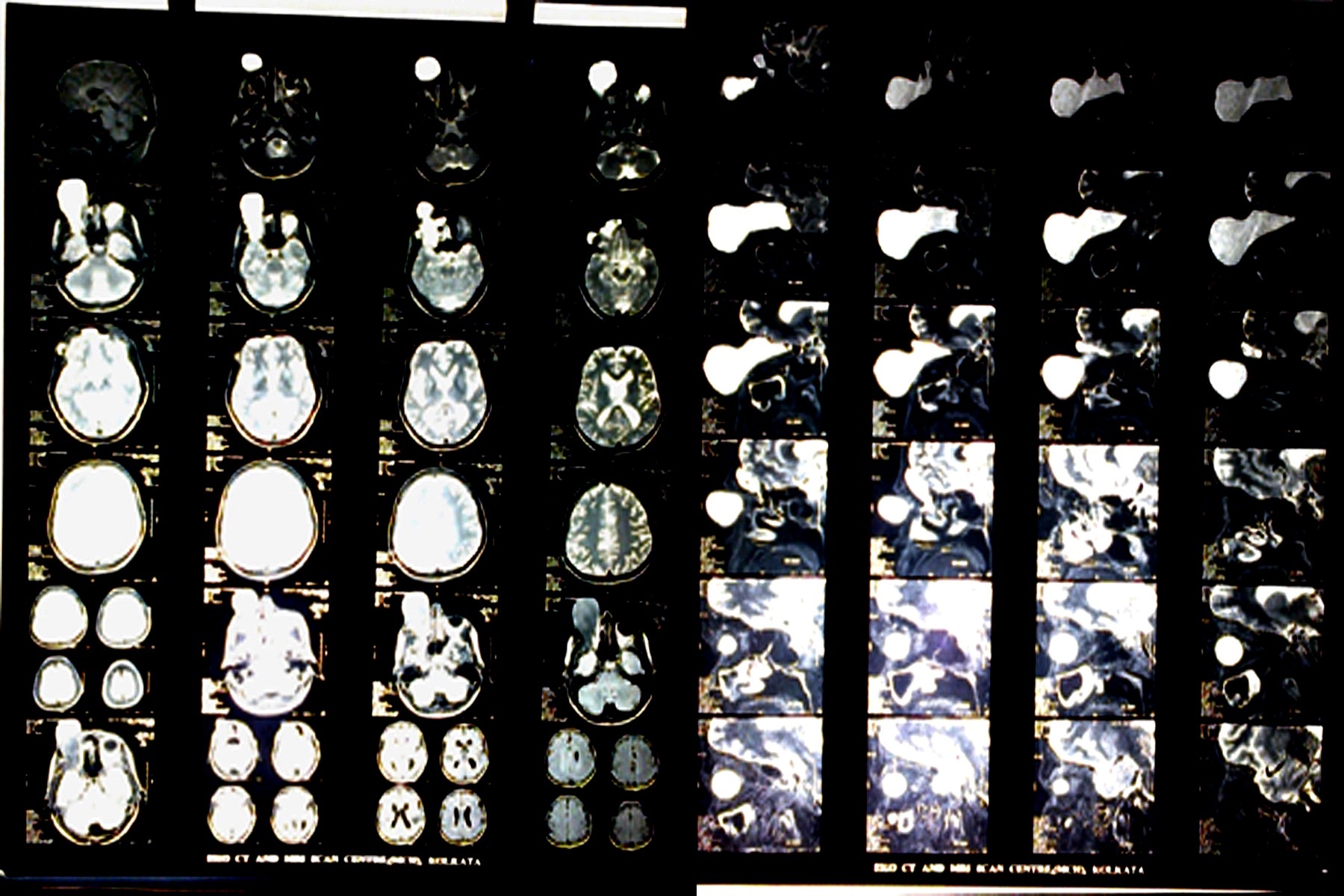
BCVA to Left eye is 6/6 -1.00 dsph with -0.25 dcyl 100 degree. Near BCVA N-6 with +1.75 dsph. Right eye no vision, it is enucleated. On examination, it is tense, cystic swelling, 80 mm/50 mm/50 mm in dimension globular mass arising from the right upper lid and orbit. Double margins of eyelashes, grey line of the lid are present and conjunctival surface of tarsal plate is visible. On palpation firm to cystic feeling, partially mobile in both vertical and horizontal axis, painless mass beneath the right superior orbital rim [Table/Fig-1]. Transillumination test was negative. No ocular anatomical structure found in right orbit. It is non-tender, non compressible, no expansile impulse on coughing, no bruit. Overlying skin is tense and stretched with blackish pigmentary colour change. Routine blood examination was within normal limit. Ultra sonography (USG) and Magnetic Resonance Imaging (MRI) was done for evaluation of the tumour mass for its location and extension. USG report showed Cystic well encapsulated mass in Right upper lid-orbital region with fat component. There are definite calcification foci inside the cystic mass [Table/Fig-2]. But USG alone is not in conclusive for the diagnosis of the location and extension of the SOL (Space occupying lesion). In this case MRI is definite for diagnosis extension and location in the lid and orbit. MRI report shows Right orbital cystic lesion seen involving right orbit with: fairly large in dimension, 75 mm/45 mm/40 mm globuler hyperintense mass with posterior extension up to optic canal. Mild extension noted in temporal region. Right ocular bulb not visualized, Right optic nerve oedematous. Pan sinusitis was noted with collection. There was evidence of underlying muscle, bone and orbicularis muscle involvement but, no evidence of intra-cranial communication and extension [Table/Fig-3]. To rule out malignancy and plan of treatment FNAC is mandatory.
Pre-operative anteroposterior and lateral view of the right upper lid and orbital epidermal inclusion cyst in above two images and postoperative anteroposterior view after removal of cyst with upper lid reconstruction and insertion of conformer in right eye below single image

USG report shows cystic encapsulated mass with calcification foci in right upper lid-orbital region with fat component
MRI Orbit and brain shows right upper lid cystic lesion involving orbit with: fairly large in dimension, 75mm/45mm/40mm globuler hyperintense mass with posterior extension up to optic canal. Mild extension noted in temporal region. Right ocular bulb not visualized, Right optic nerve oedematous. Pansinusitis noted with collection. There was evidence of underling muscle, bone and orbicularis muscle involvement. But no evidence of intra-cranial communication and extension
FNAC aspirate shows cheesy material with plenty of anucleate squamus cells suggestive of benign epidermal cyst. It was decided to remove the mass entirely.
Surgical Procedure: Elliptical incision was made over the swelling marked by marker pen before. With the help of crescent knife (2.6mm) classical cleavage was made between skin and capsule of the tumour mass.
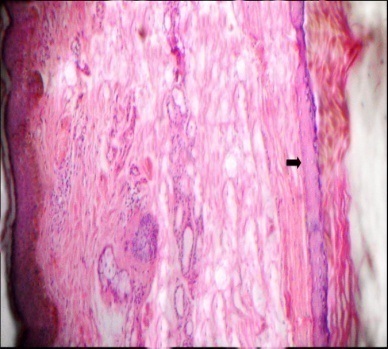
After that, tumour mass was removed with intact wall, from temporal approach. No such stalk found for intracranial communication. Potential space was closed by 6-0 polyglactin. Then wound closed by 4-0 black silk and drain given for effective drainage. Pressure badge was applied and suture removed on 7th postoperative day with good wound healing. Lower lid margin well opposed to globe [Table/Fig-4]. Tumour mass was sent for histopathological examination. Tumour mass showed grossly elongated nodular bosselated or multilobuler appearance, measuring the diameter of 5 cm horizontal/5 cm vertical and/5 cm thickness of partly cystic, partly solid mass filled with sebum. Microscopic section shows features of epidermal inclusion cyst, no malignancy [Table/Fig-5].
Steps of excision of upper lid and orbital epidermal inclusion cyst with upper lid reconstruction

Histopathological section shows orbital skin with adnexal structure within dermis epidermal cyst lining (arrow) & lamellated keratin within it (40X H&E Stain)
Discussion
Epidermoid cyst within the lid and orbit is extremely rare. It is incorporation of ectodermal elements within the cyst. It is classified as primary and secondary types or congenital and acquired variety. In primary or congenital types, there is incorporation of ectodermal elements at the time of closure of the neural groove or epithelial lines. But secondary or acquired epidermoid cysts are usually present in those areas which are more prone to repeated trauma. As a result there is incorporation of surface epithelium beneath the skin and gradually it transform into a cyst [1–6].
In 1807, Pinson first reported the case of epidermoid cyst in the orbit. Macroscopically epdermoid tumour consist of tough outer capsule which is white, glistening, smooth surface on examination and can be easily differentiated from the surrounding tissue during surgical dissection. Inside of the cyst is full of cheesy, sebum like materials of concentric lamina of keratin and epithelial debris. This material contains a numerous calcium soap deposits and has a waxy appearance with oily base.
In 1838, Muller first described the epidermoid inclusion cyst in the orbital bone. It is a secondary variety of the epidermoid cyst. It arises from the dipole of the bone. When it increases in size and shape it causes expansion of the inner and outer table of the bone. In radiography it looks sharply demarcated bone defect with widening of diploic space and typical sclerotic margin. It is the hallmark of intradiploic epidermoid cyst [7–11].
Post traumatic or secondary epidermoid inclusion cyst commonly seen in finger, palms, sole where there is repeated chance of trauma. But rarely seen in lid, orbital space and skull bone where there is minor or negligent trauma can cause epdermoid inclusion cyst [12,13].
In this case there was history of surgery evisceration four years back at the right eye. Two years after that, there is a painless, gradually, progressing swelling at the right upper lid and orbital region and it was so big that it causes impairement of lid opening and vision as well. MRI and USG suggest there is no intracranial connection, plan for surgical removal of the tumour mass. We did successful removal of the mass without any complication and with one year follow–up there is no recurrence.
Conclusion
Post traumatic epidermoid inclusion cyst is rare in the lid and orbital space. Early diagnosis and surgical treatment leads to good prognosis. In this case, cyst is not only located in the upper lid, it peculiarly enters into the orbital space (extraconal space) with typical cyst lining. It produces an hour glass structure of the cyst which is confirmed by MRI scan. Peroperative marsupialisation and thorough curettage of the lining of the cyst is mandatory otherwise it may recur e with discharging sinus. Potential space must be obliterated by non absorbable suture. Postoperatively this patient had good functional and cosmetic outcome observed after six month follow up no such recurrence of the disease.
[1]. Bajoghli A, Agarwal S, Goldberg L, Melanoma arising from an epidermal inclusion cystJ Am Acad Dermatol 2013 68(1):e6-7. [Google Scholar]
[2]. Baek HJ, Lee SJ, Cho KH, Subungual tumours: clinicopathologic correlation with US and MR imaging findingsRadiographics 2010 30(6):1621-36. [Google Scholar]
[3]. Hong SH, Chung HW, Choi JY, MRI findings of subcutaneous epidermal cysts: emphasis on the presence of ruptureAJR Am J Roentgenol 2006 186(4):961-66. [Google Scholar]
[4]. Jakobiec FA, Mehta M, Iwamoto M, Hatton MP, Thakker M, Fay A, Intratarsal keratinous cysts of the Meibomian gland: distinctive clinicopathologic and immunohistochemical features in 6 casesAm J Ophthalmol 2010 149:82-94. [Google Scholar]
[5]. Jakobiec FA, Zakka FR, Hatton MP, Eyelid basal cell carcinoma developing in an epidermoid cyst: A previously unreported eventOphthal Plast Reconstr Surg 2010 26:491-94. [Google Scholar]
[6]. Jin W, Ryu KN, Kim GY, Kim HC, Lee JH, Park JS, Sonographic Findings of Ruptured Epidermal Inclusion Cysts in Superficial Soft Tissue Emphasis on Shapes, Pericystic Changes, and Pericystic VascularityJ Ultrasound Med 2008 27:171-76. [Google Scholar]
[7]. Vagefi MR, Lin CC, McCann JD, Anderson RL, Epidermoid cyst of the upper eyelid tarsal plateOphthal Plast Reconstr Surg 2008 24:323-24. [Google Scholar]
[8]. Lucarelli MJ, Ahn HB, Kulkarni AD, Kahana A, Intratarsal Epidermal Inclusion CystOphthal Plast Reconstr Surg 2008 24:357-59. [Google Scholar]
[9]. The Eye MD Association, American Academy of Ophthalmology, Section 7: Orbit, Eyelids, and Lacrimal System. 2007-08 [Google Scholar]
[10]. Acarturk TO, Stofman GM, Post traumatic Epidermoid inclusion cyst of the Deep infratemporal fossaAnn plastic surgery 2001 46(1):68-71. [Google Scholar]
[11]. Antonius AE, Leo K, Ben V, Intradiploic Epidermoid Cysts of the Bony OrbitOphthalmology 1991 98:1737-43. [Google Scholar]
[12]. Lee KF, Philip JH, Lawrence G, Alphonse S, Three rare cases of unilateral ExophthalmosRadiology 1968 90:1009-15. [Google Scholar]
[13]. Patric CC, Epidermoid and Dermoid tumours of the orbitBritish Journal of ophthalmology 1958 42:225-39. [Google Scholar]