CT Guided Removal of Iatrogenic Foreign Body: A Broken Intravenous Cannula
Amanpreet Singh1, Anupama Kaur2, Majhail Singh3, Surinder Kaur4
1 Assistant Professor, Department of Ear, Nose and Throat, M.M Medical College, Mullana, Ambala, India.
2 Asscociate Professor, Department of Physiology, M.M Medical College, Mullana, Ambala, India.
3 Profeesor, Department of Surgery, M.M Medical College, Mullana, Ambala, India.
4 Professor, Department of Physiology, M.M Medical College, Mullana, Ambala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anupama Kaur, E-21, M.M Medical College Residential Campus, Mullana, Ambala-133207, India.
E-mail: dr.anupamakaur@gmail.com
Foreign bodies are encountered on day to day basis by a surgeon. Usually foreign bodies are lodged in narrow cavities of the body and the common age group is in children. They may range from foreign bodies in ear, nose, cricopharynx and even in rectum. Iatrogenic foreign bodies are not uncommon. Unknowingly, surgeons have been known to leave sponges, artery forceps in the abdomen which lead to hazardous sequelae. Intravascular foreign bodies occurrence has increased from a decade or so.
Cubital, Embolism, Gauge, Phlebotomy
Case Report
Here we present the case of a patient who reported in the OPD with history of pain in the right forearm for three days. He gave history of taking medication from local practitioner for gastroenteritis about 15 days back. He was given fluids by intravenous route. Intravenous cannula was removed after giving two days of medication. During removal of cannula broke and part of it remained in the vein of patient. Local practitioner informed him about the same and asked him not to worry and visit again if there is any complaint. After seven days patient felt a small swelling in the region of prick of i/v cannula on the forearm, which increased gradually. He was able to feel the broken part of cannula. On examination a tender swelling was present with local rise of temperature. On the basis of history and examination a diagnosis of intravascular foreign body i.e. broken i/v cannula was made. He was advised admission, but he refused and asked for medication. He was advised required medicines i.e. antibiotic, anti-inflammatory and thrombophobe ointment for local application.
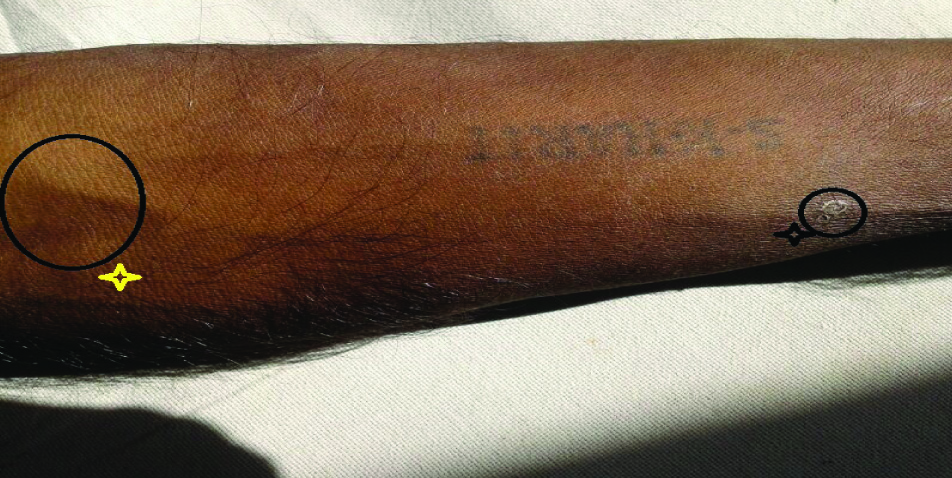
Patient again presented to the OPD next day with increases in intensity of pain and swelling near right cubital fossa. On palpation, a longitudinal firmness was felt along the course of superficial vein. Shifting of the tender swelling towards cubital fossa with palpation of longitudinal firmness indicated towards a broken intravenous cannula in one of the superficial vein of forearm [Table/Fig-1]. A tourniquet was applied proximal to the fossa to prevent further migration. Ultrasound scan was not helpful to locate the cannula. CT scan confirmed presence of an iatrogenic foreign body [Table/Fig-2].
Migration of the Swelling (Foreign Body) Marked as Black Star to Yellow Star
Arrow Showing the Broken I/V Cannula in the superficial vein of cubital Fossa

Patient was immediately taken to the operation theatre for removal of foreign body. The broken cannula was palpated and tourniquet was secured proximal to the swelling. Through a transverse incision at the upper end of the cannula, superficial vein having broken cannula was identified and rolling suture was passed to prevent further cephalic migration of foreign body. Phlebotomy was done and the broken part of the cannula was removed using artery forceps [Table/Fig-3]. Vein was ligated above and below the incision site. Incision in the skin was closed by interrupted sutures. It was noticed that the broken cannula had migrated 13 cm [Table/Fig-4].
Showing part of broken cannula projecting out of phlebotomy incision

Shows the distance of migration by the cannula

Discussion
Foreign bodies in humans are encountered on day to day basis by clinicians and surgeons. Foreign body ingestions or insertions are generally seen in children, mentally retarded persons and iatrogenic, as in our case.
The type of foreign bodies commonly encountered varies from one society to another, determined by a host of cultural factors – psychosocial and dietary being the most important [1]. The candidates for the iatrogenic, spontaneous fracture and migration of the intravenous cannula are generally the cancer patients. Spontaneous fracture and migration of intravenous cannula is a known complication and necessitates immediate removal. Distal venous embolisation of a peripheral intravenous cannula tip can occur if it loses its structural integrity which can happen either through repeated failed attempts of insertion of the same cannula or inferior quality of the intravenous cannula or prolonged peripheral intravenous cannulation which is contrary to protocols for intravenous access [2]. Hypodermic needles can also constitute foreign bodies in blood vessels especially in drug addicts [3]. Generally peripheral embolisation follows a benign course. Intravenous cannula are fractured at the site of entry into vein [4]. Another category of intravascular foreign bodies are the guide wires which generally occur during central venous catheterisation [5].
Insertion of an intravascular cannula is the most common invasive procedure with its uses ranging from infusion of intravenous fluids and medications to measuring blood pressure and blood sampling in infants. As the technology has improved each aspect of medical science, technological innovations have occurred in catheter materials. However, there are disadvantages also, which can range from loss of limb to loss of life [6].
For administration of fluids and other intravenous medications venous cannulas are very important therapeutic devices which has its own share of complications which may range from thrombophlebitis to serious complications like catheter rupture and embolism. This embolism may be diagnosed immediately, but there have been instances where it goes unnoticed for a long time and it may present as an incidental finding. Symptoms may vary from to local to severe systemic signs [7].
Various studies have been conducted on the handling and care of the peripheral intravenous cannula. One such study concludes that out of 60 cases care and handling of cannula was unsatisfactory to very unsatisfactory in 52%of the cases. Longer the cannula had been in situ greater were the complications which ranged from redness to suppurating infection [8]. The peripheral intravenous cannulation should be done as and when indicated by a trained professional using the optimum guage. One study also mentions that successful intravenous cannulation was unaffected by the catheter size [9].
Study conducted a few years back also mentions that doctors do not use local anaesthetic prior to inserting intravenous cannula [10]. Our patient had to undergo intravenous cannulation for treatment of gastroenteritis and the cannula was removed on the second day. This case is unique because the broken intravenous cannula remained asymptomatically intravascular for nearly a week. On repeated touching by the patient due to pain and irritation it may have been dislodged and migrated.
Conclusion
Broken intravenous cannula is a dangerous situation as are all the intravascular foreign bodies. They should be managed at the earliest by knowing the exact site of the foreign body using Computed Tomography. If the exact site of the foreign body is made out by Computed tomography, it becomes easier and fruitful procedure to remove the foreign body. Intravenous cannulation is the most common invasive procedure, but there is no proper training on the use of the same. Most of the doctors learn it as they go along in their residencies. Proper size and site of cannulation is very important, as is the method because as the size increases the pain also increases. In addition ignorance about the size of the cannula should be cleared.
Gloves should always be worn and cleaning solutions should be used, local anaesthetics can also be used as it makes both the patient and the doctor comfortable. Once the cannula is inside the vein proper monitoring should be done and signs such as redness, pain and swelling should be looked for. The problem of Quacks should be addressed in India as they insert cannula and give antibiotics to make easy money.
[1]. Goh YN, Tan NG, Radiological features of unusual ingested foreign bodiesSingapore Med J 2001 42(3):129-30. [Google Scholar]
[2]. Khadim MF, Leonard D, Moorehead RA, Hill C, Back to basics: iatrogenic intravenous cannula embolusAnn R Coll Surg Engl 2013 95(7):110-11. [Google Scholar]
[3]. Hart BL, Newell JD, Davis M, Pulmonary needle embolism from intravenous drug abuseCan Assoc Radiol J 1989 40(6):326-27. [Google Scholar]
[4]. Burbridge B, Stoneham G, Szkup P, Otani R, Kriegler S, Catheter fracture and embolization associated with arm implantation of the cook vital portCan Assoc adiol J 2013 64(3):269-73. [Google Scholar]
[5]. Gunduz Y, Vatan MB, Osken A, Cakar MA, A delayed diagnosis of a retained guidewire during central venous catheterisation: a case report and review of the literatureBMJ Case Rep 2012 2012 [Google Scholar]
[6]. Ramasethu J, Complications of vascular catheters in the neonatal intensive care unitClin Perinatol 2008 35(1):199-222. [Google Scholar]
[7]. Surov A, Buerke M, John E, Kösling S, Spielmann RP, Behrmann C, Intravenous port catheter embolization: mechanisms, clinical features, and managementAngiology 2008 59(1):90-97. [Google Scholar]
[8]. Lundgren A, Jorfeldt L, Ek AC, The care and handling of peripheral intravenous annulae on 60 surgery and internal medicine patients: an observation studyJ Adv Nurs 1993 18(6):963-71. [Google Scholar]
[9]. Leibovici D, Gofrit ON, Fredman B, Shemer J, Noga Y, Heruti RJ, Intravenous ine diameter: is bigger really better?Mil Med 1997 162(3):183-85. [Google Scholar]
[10]. Yentis SM, Use of intravenous cannulae by junior hospital doctorsPostgrad Med J 1993 69(811):389-91. [Google Scholar]