Metastatic Renal Cell Carcinoma: An Unusual Cause of Bleeding Pancreatic Mass
Smeeta Gajendra1, Ritesh Sachdev2, Ishani Mohapatra3, Ruchika Goel4, Shalini Goel5
1 Attending Consultant, Department of Pathology and Laboratory Medicine, Medanta-The Medicity, Gurgaon, Haryana, India.
2 Senior Consultant, Department of Pathology and Laboratory Medicine, Medanta-The Medicity, Gurgaon, Haryana, India.
3 Consultant, Department of Pathology and Laboratory Medicine, Medanta-The Medicity, Gurgaon, Haryana, India.
4 Associate Consultant, Department of Pathology and Laboratory Medicine, Medanta-The Medicity, Gurgaon, Haryana, India.
5 Associate Consultant, Department of Pathology and Laboratory Medicine, Medanta-The Medicity, Gurgaon, Haryana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ritesh Sachdev, Senior Consultant, Department of Pathology and Laboratory Medicine, Medanta-The Medicity, Sector – 38, Gurgaon-122 001, Haryana, India. E-mail : sachdev05@gmail.com
Renal Cell Carcinoma metastasizing to pancreas is uncommon, occurring in 1-2% of cases; lung being the most common site. It is usually asymptomatic, or may present as abdominal pain, weight loss, pancreatitis or gastrointestinal bleeding. Herein, we present a case of 75-year-old male presented as intraabdominal bleeding to the Emergency Department. Contrast enhanced computed tomography with angiography of abdomen showed lobulated soft tissue mass in the uncinate process region, infiltrating into the distal third and proximal fourth part of duodenum. A clinico-radiological diagnosis of carcinoma head of pancreas infiltrating into duodenum was made and the patient underwent Whipple’s operation. With past history of nephrectomy 3 years back, microscopy and the immunoprofile; a final diagnosis of clear cell renal cell carcinoma metastasizing to pancreas was given on histopathology. A high index of suspicion is required for patients with a history of RCC and they should be monitored lifelong for early detection of metastases and to improve survival.
Clear cell carcinoma, Immunohistochemistry, Pancreatic metastasis
Case Report
A 75-year-old male came to the Emergency Department with acute abdomen. Ultrasonography of abdomen revealed intra-abdominal bleed from the pancreatic head. Contrast enhanced computed tomography (CT) with angiography of abdomen showed lobulated soft tissue density mass measuring 6.1 x 4.1 cm in the uncinate process region extending and infiltrating into the distal third and proximal fourth part of duodenum [Table/Fig-1a].
CECT showing a lobulated soft tissue density mass with heterogeneous arterial enhancement in the uncinate process region extending and infiltrating into the distal third and proximal fourth part of duodenum;
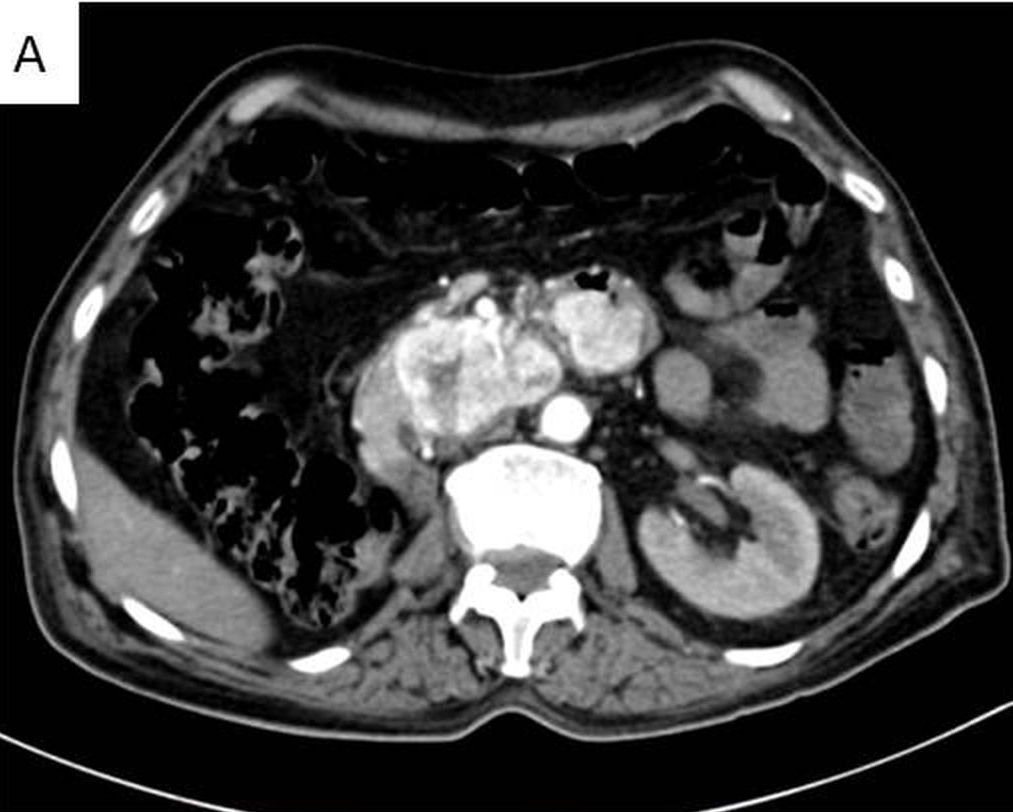
The mass was closely abutting the superior mesenteric vessel; posteriorly indenting the infrahepatic inferior vena cava. Superior mesenteric artery was free and was far from the space occupying lesion. There was no evidence of up stream pancreatic duct/ common bile duct dilation. Rest of the pancreas was normal in size, shape and contrast enhancement. Left kidney was normal in size, shape and contrast enhancement along with a tiny simple cortical cyst at the lower pole. Right kidney was not seen in right renal fossa. There was no evidence of calculus or hydronephrosis. Two tiny nodules were seen in the right lung, one in the anterior basal segment and another in posterior basal segment of right lower lobe with tiny calcified speck. A clinico-radiological diagnosis of carcinoma head of pancreas infiltrating into duodenum was made and the patient underwent Whipple’s operation.
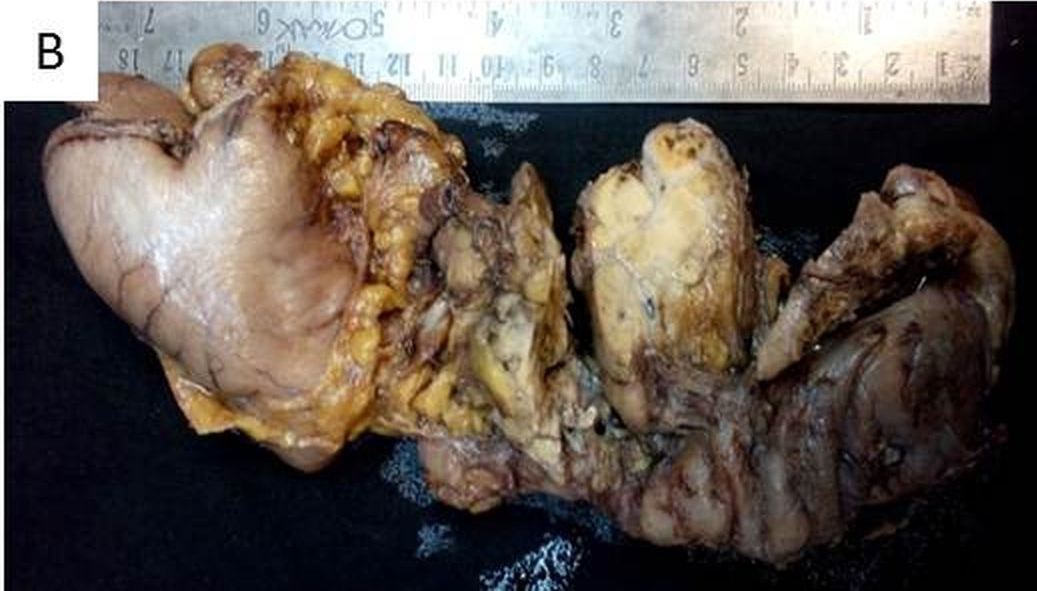
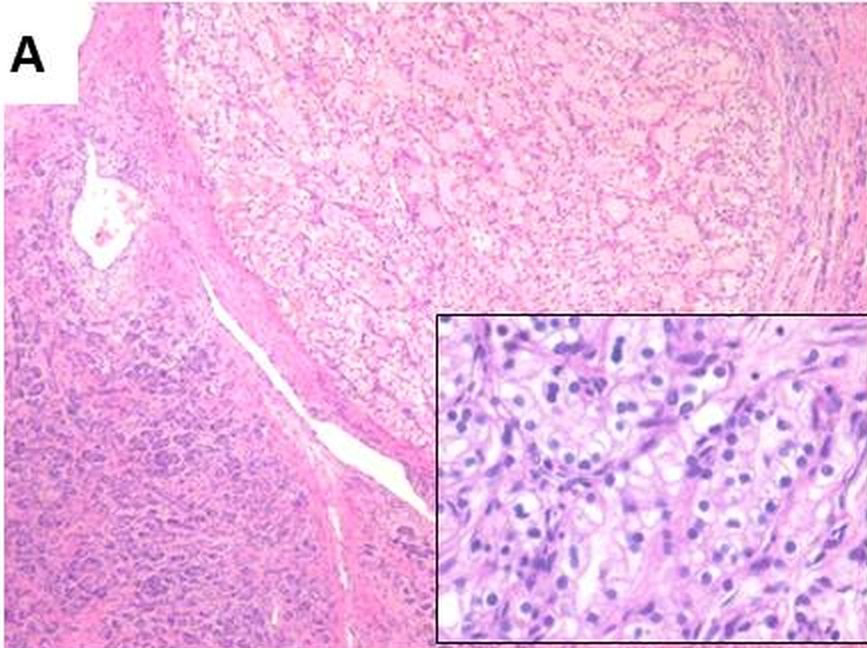
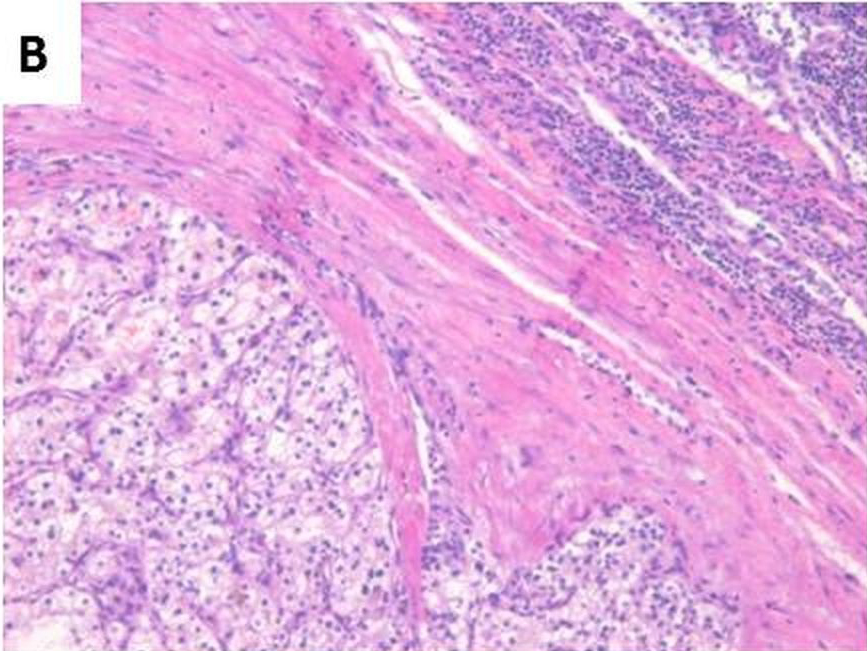
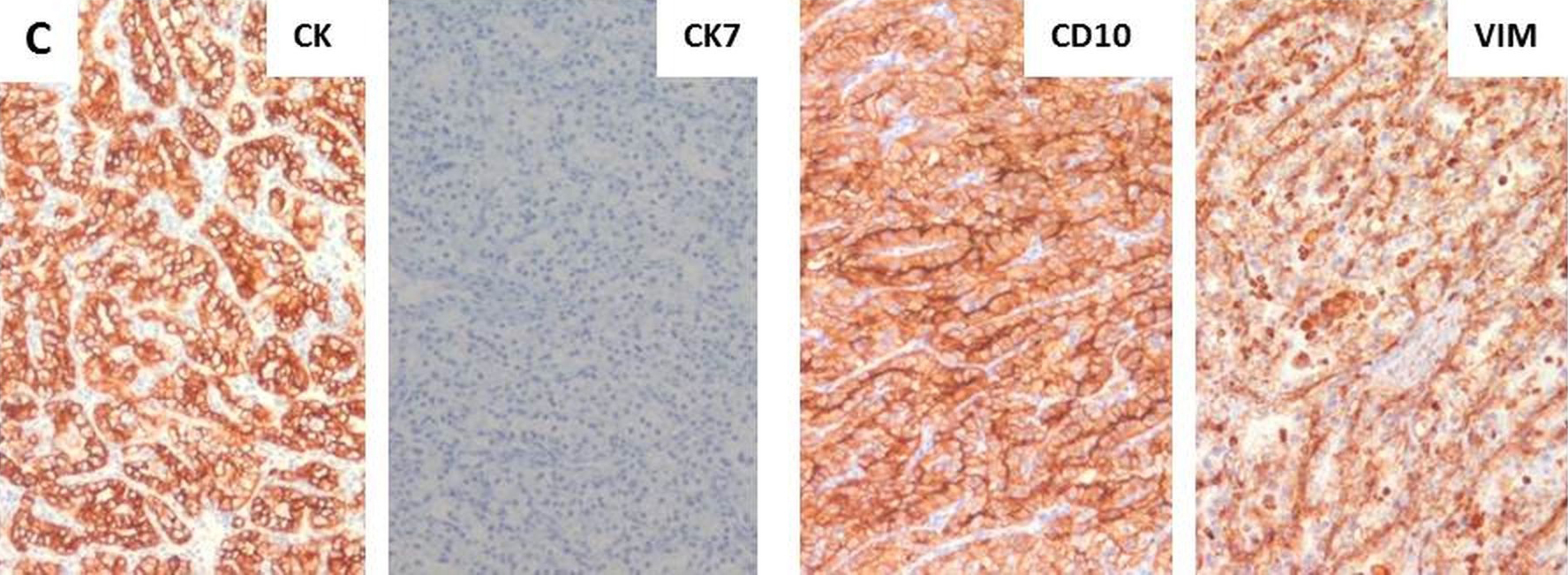
Pancreatico-duodenectomy specimen with partial gastrectomy and gall bladder was received. Grossly, the tumour mass in pancreatic head measured 4.5x4.0x3.5cm. On cut section of the tumour, variegated appearance consisting of yellow white areas, haemorrhagic areas and areas of necrosis were noted [Table/Fig-1b]. Further, sections revealed tumour infiltrating into the duodenal wall. On microscopy, well circumscribed tumour composed of sheets and nests of clear cells with hyperchromatic nuclei and many with nucleoli with intervening blood vessels [Table/Fig-2a]. There was presence of single lymph node involvement [Table/Fig-2b] with lymphovascular invasion without perineural invasion. Immunohistochemistry showed tumour cells positive for Cytokeratin (CK) (Biogenix; AE1 + AE3), Vimentin (Dako; V9), CD10 (Dako; 56C6) and negative for Synaptophysin (Dako; SY38), CK7 (DAKO; OV-TL12/30), CK20 (DAKO; KS20.8) and CA19.9 (Biogenix; C241:5:1:4) [Table/Fig-2c]. The microscopy and the immuno-profile were suggestive of Clear cell RCC with pancreatic metastasis. Till this stage no other significant history had been provided by the patient/patient party. In view of absence of right kidney in renal fossa, presence of clear cells and immuno-profile favouring RCC, the patient was further inquired about any other previous surgical history. A past history of nephrectomy 3 years back was then revealed and previous slides and blocks were requested. The slides reviewed showed tumour cells with morphology as described above. A final diagnosis of metastatic clear cell carcinoma of renal origin was given.
Surgical specimen of the Whipple operation demonstrating a 4.5x4x3.5 cm tumour in the head of the pancreas
Well-circumscribed tumour surrounded by pancreatic parenchyma. Tumour consists of large polygonal cells with clear cytoplasm, uniform round nuclei and inconspicuous nucleoli with prominent vasculature (H&E x100, inset 400X);
Tumour metastasis to lymph node (H&E 100X);
Immunohistochemistry showing tumour cells positive for CK, CD10 and Vimentin and negative for CK7
Discussion
Renal cell carcinoma (RCC) accounts for approximately 2% of all adult malignancies [1]. Lung is the most common site of metastasis in RCC [2]. The frequency of pancreatic metastases ranges from 2% to 5% of all pancreatic malignant tumours. Malignancies that can metastasize to the pancreas are RCC, melanoma, lung cancer, colorectal cancer, soft-tissue sarcoma and breast cancer. Clear cell RCCs are known for their ability of late metastases to unusual sites after resection of the primary tumour. About 20% to 30% patients of RCC have metastases at presentation and 40%-50% will develop widespread metastatic disease many years after nephrectomy. RCC metastasizing to pancreas commonly occurs in seventh decade of life. Patients are usually asymptomatic or can present as weight loss, jaundice, abdominal pain, gastrointestinal bleeding due to duodenal involvement or pancreatitis due to pancreatic duct obstruction [3]. Few cases with pancreatico-duodenal metastasis in RCC presenting with upper gastrointestinal bleeding were described in the literature in which bleeding was the first manifestation of disease or bleeding heralded disease recurrence. Upper GI bleeding was present with overt haematemesis or signs of occult blood loss [4–8]. Our case presented as acute abdomen with intra-abdominal bleeding from the pancreatic head. The sites and extent of metastatic lesions and the feasibility of pancreatic surgery can be determined by radiological investigations as CT/magnetic resonance imaging (MRI) scan. Periodic CT scan in patients of RCC allows earlier detection of small pancreatic metastasis in most cases and it is also an important tool for guidance of biopsy for a definite diagnosis. Metastases from RCC have typical characteristics of hypervascular lesions and show intense homogeneous contrast enhancement in the arterial phase, greater than normal pancreatic parenchyma. In rim enhancement with a hypodense central area of necrosis may be observed [3,9]. On MRI (with contrast), smaller lesions show homogeneous enhancement whereas rim enhancement is noted in larger lesions [3]. The radiological differential diagnosis includes primary pancreatic endocrine tumour, metastasis from hypervascular neoplasm, intrapancreatic accessory spleen, arteriovenous fistulas and aneurysms of the splenic artery [3]. In our case a lobulated mass was observed in CT with angiography in head of pancreas infiltrating into duodenum, so a clinico-radiological diagnosis of carcinoma head of pancreas infiltrating into duodenum was made. Although, majority of metastases occur within 3 years of nephrectomy for RCC, it can occur many years after nephrectomy even after 20 years of surgery. In our case pancreatic metastasis in RCC was observed after a disease free period of more than 10 years after nephrectomy. When isolated pancreatic metastasis occurs many years after primary diagnosis, it is difficult to differentiate it from primary adenocarcinoma of pancreas [10]. The 5-year survival rate decreased from 95% to less than 10%-15% once metastases have spread [11,12]. Management of duodenal metastsis from RCC depends on the general condition of the patient, site and extent of the lesion. In the case of duodenum metastasis procedures from classic pancreatico-duodenectomy (Whipple operation) to interventional embolization have been reported depending on the general condition of the patient, site and extent of the lesion. In our case the patient was managed by Whipple’s operation. Surgical pancreatic resection can be considered as part of the multidisciplinary management of patients of isolated metastasis to pancreas to achieve long overall survival [13,14]. Common prognostic factors for metastatic RCC included time from diagnosis to adjuvant treatment >12 months, haemoglobin values higher than the lower normal limit, and <2 metastatic sites [15]. The patient did not reveal the past history of nephrectomy and Whipple’s operation was done. As RCC metastasizing only to pancreas is rare, it should be kept in mind in patients’ undergone nephrectomy, even after many years of resection of primary tumour. Imaging modalities like Ultrasonography or CT scan is not much helpful in differentiating pancreatic metastasis from renal cell carcinoma from primary neuro-endocrine tumour of the pancreas because both lesions show rapid enhancement during the early phases of helical CT scan and MRI [16]. Endoscopic ultrasound guided fine needle aspiration is a useful diagnostic modality for differentiating primary from secondary pancreatic tumours by immunocytochemical analysis, by which a correct decision about further management can be taken. A long overall survival of the patients can be achieved by complete surgical resection of isolated pancreatic metastasis.
Conclusion
RCC metastasizing only to pancreas is rare, may occur many years after resection of primary tumour. A high index of suspicion is required for patients with a history of RCC, and they should be monitored life long for early detection of metastases and to improve survival.
[1]. Karimi KM, McFadden DW, Pancreatic resection for metastatic renal cell carcinoma to the pancreasAm Surg 2007 73:1158-60. [Google Scholar]
[2]. Tanis PJ, van der Gaag NA, Busch OR, van Gulik TM, Gouma DJ, Systematic review of pancreatic surgery for metastatic renal cell carcinomaBr J Surg 2009 96(6):579-92. [Google Scholar]
[3]. Ballarin R, Spaggiari M, Cautero N, Pancreatic metastases from renal cell carcinoma: the state of the artWorld J Gastroenterol 2011 17(43):4747-56. [Google Scholar]
[4]. Sadler GJ, Anderson MR, Moss MS, Wilson PG, Metastases from renal cell carcinoma presenting as gastrointestinal bleeding: two case reports and a review of the literatureBMC Gastroenterology 2007 7:4 [Google Scholar]
[5]. Chang WT, Chai CY, Lee KT, Unusual upper gastrointestinal bleeding due to late metastasis from renal cell carcinoma: a case reportKaohsiung J Med Sci 2004 20(3):137-41. [Google Scholar]
[6]. Cherian SV, Das S, Garcha AS, Gopaluni S, Wright J, Landas SK, Recurrent renal cell cancer presenting as gastrointestinal bleedWorld Journal of Gastrointestinal Oncology 2011 3(6):99-102. [Google Scholar]
[7]. Machado NO, Chopra P, Pancreatic metastasis from renal carcinoma managed by Whipple resection. A case report and literature review of metastatic pattern, surgical management and outcomeJOP 2009 10(4):413-18. [Google Scholar]
[8]. Espinoza E, Hassani A, Vaishampayan U, Shi D, Pontes JE, Weaver DW, Surgical excision of duodenal/pancreatic metastatic renal cell carcinomaFront Oncol 2014 4:218 [Google Scholar]
[9]. Shi HY, Zhao XS, Miao F, Metastases to the Pancreas: Computed Tomography Imaging Spectrum and Clinical Features: A Retrospective Study of 18 Patients With 36 MetastasesMedicine (Baltimore) 2015 94(23):e913 [Google Scholar]
[10]. Katsourakis A, Noussios G, Hadjis I, Alatsakis M, Chatzitheoklitos E, Late solitary pancreatic metastasis from renal cell carcinoma: a case reportCase Rep Med 2012 2012:464808 [Google Scholar]
[11]. Janzen NK, Kim HL, Figlin RA, Belldegrun AS, Surveillance after radical or partial nephrectomy for localized renal cell carcinoma and management of recurrent diseaseUrol Clin North Am 2003 30:843-52. [Google Scholar]
[12]. David AW, Samuel R, Eapen A, Vyas F, Joseph P, Sitaram V, Pancreatic metastasis from renal cell carcinoma 16 years after nephrectomy: a case report and review of the literatureTrop Gastroenterol 2006 27(4):175-76. [Google Scholar]
[13]. Reddy S, Wolfgang CL, The role of surgery in the management of isolated metastases to the pancreasLancet Oncol 2009 10(3):287-93. [Google Scholar]
[14]. Konstantinidis IT, Dursun A, Zheng H, Wargo JA, Thayer SP, Fernandez-del Castillo C, Metastatic tumours in the pancreas in the modern eraJ Am Coll Surg 2010 211(6):749-53. [Google Scholar]
[15]. Mekhail TM, Abou-Jawde RM, Boumerhi G, Malhi S, Wood L, Elson P, Validation and extension of the Memorial Sloan-Kettering prognostic factors model for survival in patients with previously untreated metastatic renal cell carcinomaJ Clin Oncol 2005 23(4):832-41. [Google Scholar]
[16]. Tatovica D, Farrugiab D, Jewell F, Ulahannana T, Late metastases to the pancreas from resected renal cell carcinoma masquerading as multiple endocrine neoplasiaGrand Rounds 2009 9:14-17. [Google Scholar]